This sample Long Term Care in Health Services Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
For the most part long-term care (LTC) has not been among the main concerns of health policy makers. Cost-containment issues, perhaps an excessive focus on specialized medical care, and the fact that families have always been and remain the major providers of LTC have contributed to a slow development of public long-term care services (WHO, 2000). However, demographic transitions are resulting in dramatic changes in health needs around the world. Care for the chronically ill and for those with disabilities and a steep rise in the numbers of elderly are a growing challenge in practically all societies.
Definition And The Target Population In Need Of LTC
LTC includes activities undertaken for persons who are not fully capable of self-care on a long-term basis by informal caregivers (family and friends), formal caregivers, and volunteers.
The target population includes those who suffer from any kind of physical or mental disability requiring assistance with the activities of daily living.
LTC encompasses a broad array of services such as personal care and assistive devices that are designed to minimize, restore, or compensate for the loss of independent physical or mental functioning.
Disability also results in difficulties in accessing health care and in complying with health-care regimes, and it affects the ability of the individual to maintain a healthy lifestyle to prevent deterioration in functional status. Therefore, LTC includes efforts to ensure access to acute, chronic care and rehabilitation services and to prevent deterioration of the functional capacity of the disabled (such as, for example, preventing bedsores and preventing depression). The central role of the family in providing LTC requires significant efforts to inform and guide the families (WHO, 2002).
The Uniqueness Of Long-Term Care
Whereas more traditional health care is concerned with cure and recovery, LTC attempts mainly to contribute to alleviating suffering, maintaining the best possible quality of life, reducing discomfort, improving the limitations caused by diseases and disability, and maintaining the best possible levels of functioning (Larizgoitia, 2003).
An additional significant difference between LTC and the acute sector is that the provision of LTC is heavily based on unspecialized, labor-intensive, and relatively unskilled providers. Professionals (physicians, nurses, social workers, and others) are involved to a degree that is significantly less than that in acute care. LTC allows lay volunteers, in particular the family, to take part in its implementation. Indeed, in most countries, care is still predominantly a family task – mainly performed by women. Despite the increasing role of the government, nongovernmental organizations (NGOs) and the private (for-profit) sectors in service provision, informal care has remained the dominant form of care (Wiener, 2003). However, the increasing proportion of women in the labor market and the declining ratio between those needing care and those who are potential caregivers are raising questions of whether informal care will maintain its predominant role.
Issues In The Organization And Provision Of LTC Services
All developed countries have established LTC programs under the auspices of health and welfare services, and many developing countries are in the initial stages of some development. Programs usually include some combination of health, social, housing, transportation, and support services for people with physical, mental, or cognitive limitations. However, there is no single paradigm and there are a number of different approaches in the organization and provision of LTC. An understanding of the nature of the variance among countries is important to provide insight for development of care policies.
Countries differ in the way they have resolved basic design issues. Among the most central issues are the nature of entitlements, targeting and finance; service delivery strategies; and issues of integration between LTC and health and social services.
Nature Of Entitlements, Targeting And Finance
Among the most significant key policy design issues are the principles of eligibility for publicly subsidized LTC services and the nature of entitlements. Underlying these issues are two fundamental decisions:
- Who does a country decide to support – everyone or only the poor?
2.. Should access to services be based on an entitlement (insurance principle) or subject to budget constraints (tax-funded principle)?
Such questions also arise in the provision of acute care. What is unique, however, to LTC is the additional possibility that the family might at least in part meet these needs for many individuals. Thus, underlying this determination is society’s view of the appropriate and expected roles of the people with disabilities and their families.
The choice among different options is often between selective (or means-tested) and universal approaches to service provision. Support for the poor is obviously based on a concern for their inability to purchase these services and can lead to an exclusive focus on this group. Even if such is one’s primary goal, this can lead to a strategy that supports the nonpoor, if it is believed that including them in a more universal program is the best way to mobilize support for the poor and to avoid the problems associated with programs for the poor, such as low quality. Support for the broader population can have several rationales, including:
- The catastrophic potential nature of LTC costs when broad segments of the population may find it difficult to pay; when resources are depleted, they become a burden on public programs;
- Concern with the broader social costs of care provision and an interest in easing the burden on families (particularly women);
- Reducing utilization of more costly acute care (particularly hospitalization) services by substituting LTC and in part by medicalizing it.
A second key question is whether access to LTC services should be based on an entitlement or subject to budget constraints. An entitlement program means that, irrespective of available budgets, everyone who fulfills the eligibility criteria must be granted benefits.
Entitlement programs are generally financed through insurance-type prepayments, whereas nonentitlement programs are usually financed through general taxation. A prepayment is generally viewed as granting a right to a service.
It should be kept in mind that an entitlement approach can influence the targeting of services. With contributory entitlement, strict income testing is unlikely to be adopted so as to prevent exclusion from benefits for the many who contribute to financing the program. Nonentitlement programs, focused primarily on the poor, will usually have a relatively strict means test.
The decision to adopt an entitlement approach and a contributory finance system has implications for additional eligibility criteria. The nature of family availability and support will not typically be taken into account in an insurance framework.
A third implication is that under an entitlement system, benefit levels are set relatively lower because family support is not a criterion, and benefits will be provided to many who might already be receiving significant family support. Setting low benefit levels also reflects concern with cost control. In an entitlement system, cost is not easily predictable or defined because it is determined by the number of eligible applicants.
We can illustrate the variation in these fundamental design issues by using a couple of examples. On the one hand, in the UK, provision of LTC is normally income tested and provided on a budget-restricted basis. On the other hand, Scandinavian countries (e.g. Sweden) have a policy commitment to maintaining high levels of services to the entire population and not only for the poor, even though services are financed through general taxation. There are user charges related to income, but given the high level of pensions, this has not been a significant barrier for those who need LTC services. Most Canadian provinces are somewhere in between countries like the UK and the Scandinavian countries with respect to targeting the poor (UK Royal Commission on Long-Term Care, 1999).
The Medicaid program in the United States is an interesting example of a system that while focusing on the poor and financed by general tax revenues provides an entitlement subject to a strict means test.
In recent years, a number of countries have adopted a broader insurance-based approach and a full entitlement. This model includes Germany, Austria, Holland, Israel, and more recently Japan (Brodsky et al., 2000).
Service Delivery Strategies: Balancing Care In The Home, In The Community, And In Institutions
Another element of variation among countries is reflected in the actual package of services offered to people with disabilities. There is no universally agreed-upon package of LTC services. For one thing, countries are in different stages of economic development, and some can afford a more comprehensive package than others. In addition, countries have different sociodemographic and epidemiological patterns, cultures, and values, which can all play an important role in defining the needs and priorities. For example, in Sweden most families do not feel obligated to look after older parents, believing that this is just as much the role of government. In contrast, in Israel much more is expected of family members (and less by government).
One of the most important distinguishing dimensions among services is the location in which these services are to be provided, collectively referred to as a continuum of care: home-based, in ambulatory settings in the community, or in a LTC institutional setting.
Home-Based Programs
Such programs may include
- Home health services – include skilled medical/ nursing care, health promotion, prevention of functional deterioration, training and education, facilitation of self-care, and palliative care;
- Personal care – care related with activities of daily living (ADL) (e.g., bathing, dressing, eating, and toileting);
- Homemaking – assistance with instrumental activities of daily living (IADL) (e.g., meal preparation, cleaning, and shopping);
- Assistive devices, physical adaptations of the home, and special technologies (alarm systems).
Ambulatory Settings
Ambulatory settings in the community can provide a different package of services, which may be more health related or more social related. For example, some models of day-care provision focus on health-related services such as monitoring of health status and rehabilitation, whereas others focus on providing the disabled person opportunities for recreation and socialization.
Institutional Services
This model includes a wide range of institutions which provide various levels of maintenance and personal or nursing care. There are LTC institutions aimed mainly at addressing housing needs and providing opportunities for recreation and socialization, whereas others (usually referred to as nursing homes or skilled nursing homes) address health-related needs. The first type serves the moderately disabled, whereas the second type the more severely disabled.
Assistive Living, Service-Enriched Housing, And Sheltered Housing
This model includes special housing units that offer independent living but also services and care to an extent, which, in some cases, comes close to a modern, noncustodial institution. These kinds of sheltered accommodations are now substituting the traditional residential homes, and to some extent also nursing homes.
Whereas almost all industrialized countries offer a broad package of services, the absolute level and the relative importance of the service mix vary. There is also noticeable convergence. In most industrialized countries, the share of the older population (over 65) in institutions varies between 5 and 7%. This percentage does not appear to have grown dramatically in recent years despite continued aging of older populations, and in some countries such as Canada and Holland, it has even declined.
Partly because of the rising cost of institutional care, a focus on community care has taken place in many industrialized countries. ‘Aging in place’ is perceived as preferred by the elderly and, in the majority of cases, as a less expensive alternative to institutional care. One of the hopes of those planning various LTC programs was that their broader availability would reduce costs by reducing acute care hospital utilization and the demand for long-term institutional care. In Japan and Canada, for example, there is an overuse of acute beds by those needing LTC. As a result, reforms have been introduced in Quebec. The Netherlands is one of the countries in which the level of institutional care has been particularly high. The Dutch government has actively implemented experimental programs aimed at reducing institutionalization.
Although the infrastructure of supportive services has grown, the expectation of diverting a significant number of disabled elderly people from nursing homes has been somewhat scaled down in many countries. The extent to which the various LTC programs have influenced patterns of referral to institutions has depended in part on the extent and type of community care available. When such services are limited, they are less likely to offer an alternative to institutionalization, particularly for the more severely disabled elderly.
More recently, some countries have highlighted the potential of health services such as post-acute care and rehabilitation in delaying or preventing long-term institutionalization. Over and above the availability of community services, other factors may affect an elderly client’s ability to choose between community and institutional services, including the supply of beds and the level of copayments for institutional care. In Germany, for example, a copayment of 25% is levied on people entering LTC to keep such care from becoming financially preferable to home care. Japan has made similar efforts to damp down institutional demand.
There is a wide variation in the provision of home care. For example, home help (nursing and assistance in activities of daily living) has been estimated to be provided to between 5 and 17% of the population, depending on the country (OECD, 1999).
In some countries, greater individual flexibility in choice of care delivery has been considered, for example, the provision of cash benefits in addition to or instead of services in-kind. There are three basic forms of provision: services in kind (e.g., Israel); cash allowances without restrictions which enables a client to use the funds as he or she sees fit (e.g., Germany and Austria); and cash allowances with a restriction to purchase services (e.g., experimental programs in Holland and the United States).
Long-Term Care Assessment
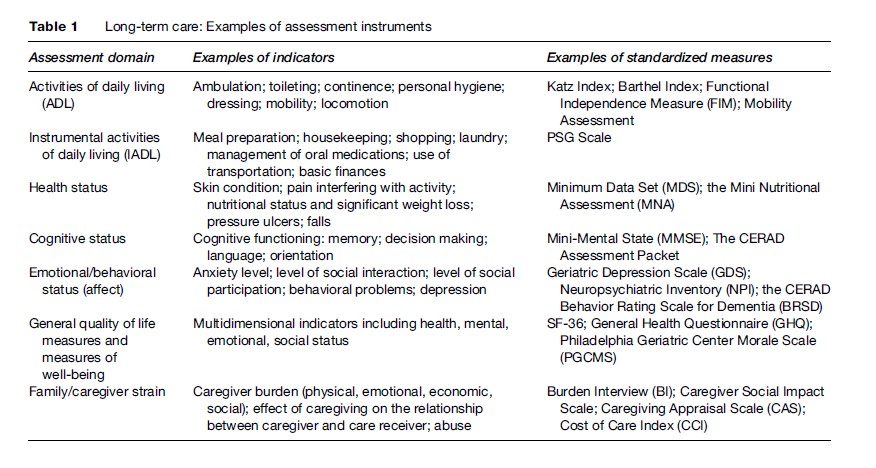
Assessment in LTC serves multiple purposes: to determine eligibility for services, develop the most appropriate care plan according to clients’ needs, monitor clients’ status over time, and assess services’ outcomes in relation to functional needs or maintaining maximum function and enhancing the quality of life of people with disabilities and of their families. At a health-service level, measures may be used to monitor quality of care, allocate resources based on case mix, and even to plan for the development of appropriate resources (Berg and Mor, 2001). The desired characteristics of an assessment instrument will vary relative to the objective of the assessment, but the same instruments can sometimes be used for multiple purposes. Comprehensive assessment should address different domains of impairment (e.g., cognitive status, strength, sensory and perceptual deficits), disability (e.g., measures of activities of daily living), and health related quality of life (e.g., mental health and emotional well-being). For each domain, there is no single best measure. There is general agreement as to the types of domains and indicators that should be included in assessment for long-term care, although the relative weights to be placed on these various domains are more debatable.
There are numerous available assessment instruments that focus on particular aspects of LTC. Table 1 gives selective examples of some of the most established instruments developed in the United States and Europe. Some of these instruments are quite culturally specific and would need to be adapted not only to other languages but also to other cultures and worldviews.
In the United States, Medicare and Medicaid authorities, along with the development of managed care, have given a tremendous push to research in this area (Shaughnessy et al., 1994). One of the best-known LTC assessment tools is the Minimal Data Set (MDS). Its main aim is to provide a reliable, uniform, and universal set of data across settings and for different purposes, which are used to inform care planning to provide a basis for external quality surveys and internal continuous quality improvement and in the case mix adjusted reimbursement systems. Although MDS began in institutions in the United States, it has since been expanded for home care and other settings, and has been used in both English and non-English-speaking countries.
Issues Of Integration Between LTC And Health And Social Services
A major concern involves the continuum of care between the acute and LTC systems, and between the health and social service systems. However, one of the major problems in many countries is fragmentation of such services (Clarfield et al., 2001). The interest in integration arises out of a number of concerns for the quality and efficiency of care. These include the ability to provide for coordinated care packages, consider alternative services in the most optimal way, and ease the access to services by offering one easily identified source of provision. Nevertheless, it is by no means simple to provide integrated LTC because services are the responsibility of many jurisdictions, and the various components tend to work in parallel with separate funding streams and budgets.
Links between LTC and acute health systems can encourage continuity of care. These connections may reduce acute hospital stays and create an incentive to provide adequate home health care and rehabilitation, especially if the health-care providers can enjoy the benefits of reduced institutional long-term care. At the same time, there are concerns about linking LTC with primary health care that generate interest in independent models of LTC. The impact of integration on incentives to provide adequate LTC are neither certain nor easily predictable. Within health systems, there is concern for a preference toward addressing acute care needs over those that are more chronic or function related. A related concern is for the overmedicalization of LTC services if provided in a medically oriented system and the consequences of higher costs as a result. In addition, in the United States, for example, the integration of acute and LTC has depended on integrating medical and social care funding streams. There is a belief that such integrated funding is the basis for program integration. However, although such linkage is necessary, it is insufficient. Successful integration requires a major reorganization of the programmatic infrastructure, which can then be reinforced with funding approaches (Kane, 2003).
In general, most developed countries have not fully integrated LTC within the acute system. Some countries have made an effort to partially integrate components of LTC (e.g., Germany), where it is administratively but not financially integrated. Other countries have implemented demonstration projects that fully integrate acute and LTC such as the PACE program in the United States and the SIPA program in Quebec (Be´land et al., 2006).
The PACE – program for all-inclusive care of the elderly – was implemented experimentally in one neighborhood in San Francisco in the 1970s and has been expanded to some 36 locations throughout the United States. The model enables the resources for acute and long-term care to be pooled. Disabled elderly who join the program receive a variety of services under one roof. Those eligible for the program are disabled elderly who are eligible to enter long-term care facilities from Medicaid, but who remain in their homes. The program is funded on a capitation basis by Medicare and Medicaid.
SIPA – French acronym for system of integrated care for older persons – is an integrated system of social, medical, and short and long-term hospital services offered in both the community and institutions to vulnerable elderly persons. It has been implemented in Canada. Its distinguishing features are community-based multidisciplinary teams with full clinical responsibility for delivering integrated care through the provision of community health and social services and the coordination of hospital and nursing home care; all within a publicly managed and funded system.
In the absence of integrated systems, many countries have been experimenting with various coordinating mechanisms such as care management.
Conclusions
Care for people with disabilities is a major challenge in industrialized as well as in developing countries. We have shown that although almost all industrialized countries offer a broad package of services, their level and mix vary among countries. In some areas there seems to be more convergence, whereas in others, policies have taken a different route and differ on principles of targeting, entitlement, and finance. There is much to be learned from the experience of industrialized countries in defining the range of options and in learning from some of the disadvantages and advantages of these systems. Unfortunately, the ability to learn from the experience is limited by the lack of adequate systems for monitoring outcomes and evaluating implementation, as well as in difficulty in ‘comparing apples and oranges.’ As LTC programs continue to develop, it is hoped that more attention will be given to systematic and comparative evaluations.
Bibliography:
- Be´ land F, Bergman H, Lebel L, et al. (2006) Integrated services for frail elders (SIPA): A trial of a model for Canada. Canadian Journal of Aging 25(1): 25–42.
- Berg K and Mor V (2001) Long term care assessment. In: Maddox (ed.) The Encyclopedia of Aging, 3rd ed., pp. 631–633. New York: Springer.
- Brodsky J, Habib J, and Mizrahi I (2000) Long-Term Care Laws in Five Developed Countries. Geneva. Switzerland: World Health Organization, WHO/NMH/CCL/00.2.
- Clarfield AM, Bergman H, and Kane R (2001) Fragmentation of care for frail older people – an international problem. Experience from three countries: Israel, Canada and the United States. Journal of the American Geriatric Association 49(12): 1714–1721.
- Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, and Gornbein PH (1994) The neuropsychiatric inventory: Comprehensive assessment of psychopathology in dementia. Neurology 44: 2308–2314.
- Folstein MF, Folstein SE, and McHugh PR (1975) Mini mental state: A practical method for grading the conginitive state of patients for the clinician. Journal of Psychiatric Research 12: 189–198.
- Golberg DP and Hillier VF (1989) A scaled version of the general health questionnaire. Psychological Medicine 9: 139–145.
- Heyman A, Fillenbaum G, and Nash F (eds.) (1997) Consortium to Establish a Registry for Alzheimer’s Disease: The CERAD experience. Neurology 49 (suppl 3, whole issue).
- James LM, Mack J, Patterson M, and Tariot P (1999) Behavior rating scale for dementia: Development of test scales and presentation of data for 555 individuals with Alzheimer’s disease. Journal of Geriatric Psychiatry and Neurology 12(4): 211–223.
- Kane R (2003) The interface of LTC and other components of the health and social services systems in North America. In: Brodsky J, Habib J, and Hirschfeld M (eds.) Key Policy Issues in Long-Term Care, pp. 63–90. Geneva, Switzerland: World Health Organization.
- Katz S, Ford AB, Moskowitz RW, Jackson BA, and Jaffe MW (1963) The Index of ADL: A standarized measure of biological psychosocial function. Journal of the American Medical Association 185: 914–919.
- Keith RA, Granger CV, Hamilton BB, et al. (1987) The Functional Independence Measure (FIM): A new tool for rehabilitation. Advances in Clinical Rehabilitation 1: 6–18.
- Kosberg JI and Cairl RE (1986) The cost of care index: A case management tool for screening informal care providers. The Gerontologist 26(3): 273–278.
- Larizgoitia I (2003) Approaches to evaluating LTC systems. In: Brodsky J, Habib J, and Hirschfeld M (eds.) Key Policy Issues in Long-term Care, pp. 227–242. Geneva, Switzerland: World Health Organization, ISBN 92 4 156225 0.
- Lawton MP (1975) The Philadelphia Geriatric Center Morale Scale: a revision. Journal of Gerontology 30(1): 85–89.
- Lawton MP and Brody EM (1969) Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 9: 179–186.
- Lawton MP, Kleban MH, Moss M, et al. (1989) Measuring caregiving appraisal. Journal of Gerontology 44(3): 61–71.
- Mahoney FJ and Barthel DW (1965) Functional evaluation: The Barthel Index. Medical Journal of Rehabilitation 14: 61–65.
- Morris JN, Fries BE, Steel K, et al. (1997) Comprehensive clinical assessment in community setting: applicability of the MDS-HC. Journal of the American Geriatric Society 45(8): 1017–1024.
- OECD (1999) A Caring World. Paris, France: Organization for Economic Cooperation and Development.
- Poulschock SW and Deimling GT (1984) Families caring for elders in residence: Issues in the measurement of burden. Journal of Gerontology 39(2): 230–239.
- Royal Commission on Long-Term Care (1999) With Respect to Old Age: Long-term Care – rights and Responsibilities. United Kingdom: The Stationery Office.
- Shaughnessy PW, Crisler KS, Schlenker RE, et al. (1994) Measuring and assuring the quality of home health care. Health Care Financing Review 16(1): 35–67.
- Sheikh JI and Yesavage JA (1986) Geriatric Depression Scale (GDS): Recent Evidence and Development of a Shorter Version. Clinical gerontology: A Guide to Assessment and Intervention, pp. 165–173. New York: The Haworth Press
- Tinetti ME (1986) Performance-oriented assessment of mobility problems in elderly patients. Journal of the American Geriatric Society 34(2): 119–126.
- Vellas B, Guigoz Y, Garry PJ, et al. (1999) The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition 15(2): 116–122.
- Ware JE, Jr. and Sherbourne CD (1992) The MOS 36-Item Short-Form Health Survey (SF-36). Medical Care 30(6): 473–483.
- WHO (2000) WHO Study Group on Home-based Long Term Care. Geneva, Switzerland: World Health Organization, Technical Report Series, No. 898.
- WHO (2002) Lessons for Long-term Care Policy. Geneva, Switzerland: World Health Organization, WHO/NMH7CCL/02.1.
- Wiener J (2003) The role of informal support in long-term care. In: Brodsky J, Habib J, and Hirschfeld M (eds.) Key Policy Issues in Long-term Care, pp. 3–24. Geneva, Switzerland: World Health Organization.
- Zarit SH, Reever KE, and Bach-Peterson J (1980) Relatives of the elderly: Correlates of feelings of burden. The Gerontologist 20: 649–655.
- Brodsky J, Habib J, and Hirschfeld M (eds.) (2003) Long-Term Care in Developing Countries: Ten Case Studies. Geneva, Switzerland: World Health Organization.
- Brodsky J, Habib J, Hirschfeld M, and Siegel B (2002) Care of the frail elderly in developed and developing countries: The experience and the challenges. Aging Clinical and Experimental Research 14(4): 279–286.
- Feldman PH and Kane RL (2003) Strengthening research to improve the practice and management of long-term care. The Milbank Quarterly 81(2): 179–220.
- Jacobzone S (1999) Ageing and Care for Frail Elderly Persons: An Overview of International Perspectives. Paris: Organization for Economic Cooperation and Development (OECD), Labour Market and Social Policy– Occasional Papers, No. 38.
- Ikegami N and Campbell JC (2002) Choices, policy logics and problems in the design of long-term care systems. Social Policy and Administration 36(7): 719–734.
- Kane RA, Kane RL, and Ladd R (1998) The Heart of Long-Term Care. New York: Oxford University Press.
- Kodner DL (2004) Following the logic of long term care: Toward an independent but integrated sector. International Journal of Integrated Care 4. http://www.ijic.org (accessed November 2007).
- Morris JN, Fries BE, Steel K, et al. (1997) Comprehensive clinical assessment in community settings: applicability of the MDS-HC.’’ Journal of the American Geriatrics Society 45(8): 1017–1024.
- OECD (1996) Caring for Frail Older People, Policies in Evolution. Paris, France: Organization for Economic Cooperation and Development, Social Policies Studies No. 19.
- Pacolet J, Bouten R, Lanoye H, and Vesieck K (1999) Social Protection for Dependency in Old Age in the 15 EU Member States and Norway. Luxemburg: Employment & Social Affairs – Social Security and Social Integration, European Commission, Office for Official Publications of the European Communities.
- Stone R (2000) Long-Term Care for the Elderly with Disabilities: Current Policy, Emerging Trends, and Implications for the Twenty-First Century. New York: Milbank Memorial Fund.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








