This sample Eating Disorders Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Public Health Significance
Eating disorders comprise a related group of mental disorders characterized by disturbance in dietary patterns, body image, and/or efforts to control weight. Taken together, anorexia nervosa and bulimia nervosa have the highest mortality rate (tied with substance use disorders) of any mental illness (Harris and Barraclough, 1998). Given that these disorders most frequently have their onset in adolescence, this high mortality rate is particularly striking. Premature death in individuals with these disorders is attributable both to suicide – there is a suicide rate of 23 times expected in these disorders (Harris and Barraclough, 1997) – and to medical complications from low weight, poor nutrition, and purging behaviors.
Although eating disorders are considered mental illnesses, their associated behaviors – including restrictive pattern eating, binge-pattern eating, and purging and other behaviors meant to neutralize the effects of overeating or to control weight – commonly result in malnutrition, obesity, and a wide variety of complications that affect nearly every organ system. Individuals with an eating disorder may induce vomiting or misuse laxatives, enemas, diuretics, or stimulants to lose weight. Others restrict eating or exercise compulsively. Those with comorbid insulin-dependent diabetes mellitus have been known to underdose insulin with the intent to lose weight. This is particularly dangerous because it can lead to diabetic ketoacidosis. Chronic purging may cause erosion of dental and gastrointestinal dysfunction (Becker et al., 1999). Metabolic disturbances, such as hypokalemia, may result from chronic vomiting or chronic laxative or diuretic misuse and can contribute to potentially fatal cardiac arrhythmia and renal disease.
Classification
The Diagnostic and Statistical Manual for Mental Disorders (DSM)-IV (APA, 1994) consists of three diagnostic categories of eating disorders: Anorexia nervosa (AN), bulimia nervosa (BN), and eating disorder not otherwise specified (EDNOS). The criteria for AN include refusal to maintain adequate body weight (e.g., 85% expected), fear of weight gain, disturbance in how weight/shape are experienced, and amenorrhea. Criteria for BN include objective binge eating and inappropriate compensatory behaviors at least twice weekly for 3 months, plus extreme importance of weight/shape to self-evaluation. If a patient meets criteria for both AN and BN, the diagnosis of AN supersedes the diagnosis of BN. It should be noted, however, that diagnostic criteria, especially 85% expected body weight in AN, are not absolute, and should not be used alone as thresholds for clinical care, especially in children, according to APA (2006) and NICE practice guidelines (Wilson and Shafran, 2005).
EDNOS is the category reserved for eating disorders of clinical severity that do not meet diagnostic criteria for either AN or BN. Although nominally a residual category, EDNOS is the most common eating disorder diagnosis made in most outpatient settings other than those attracting highly specialized referrals (Fairburn and Bohn, 2005). Accumulating evidence suggests that EDNOS and AN or BN are indistinguishable on severity of psychopathology and related impairment.
Within EDNOS, binge eating disorder (BED) was proposed as a disorder requiring further study in DSM-IV, and uncertainty remains as to whether it constitutes a separate clinical category (see Wilfley et al., 2003). BED is characterized by recurrent episodes of binge eating without the compensatory behaviors in BN or other extreme methods of weight control. Night eating syndrome (NES), characterized by wakeful nighttime eating, is a unique combination of eating disorder, sleep disorder, and mood disorder. Various diagnostic criteria for NES have been proposed, and the disorder warrants further research.
Prevalence And Cultural Issues
The majority of individuals with an eating disorder in the United States do not access formal health care for their illness (Hudson et al., 2007). One major reason for this is that up to half of cases presenting in primary care settings are unrecognized by clinicians (Becker et al., 1999). A reluctance to relinquish symptoms that characterize AN and BN, the frequent absence of clinical signs in BN, BED, and EDNOS, and clinician referral patterns (Becker et al., 2003) may contribute to this suboptimal access to care. Even individuals who do access treatment have an unacceptably high rate of continued symptoms (Keel and Mitchell, 1997).
The reported prevalence of eating disorders may underestimate true prevalence, as both self-report and interview-based ascertainment may miss cases if an individual is unwilling to disclose his or her symptoms. Moreover, differential access to care may contribute to prolonged duration of illness and elevated prevalence in some populations. Point prevalence of eating disorders in Western Europe and the United States is estimated at 0.3% for anorexia nervosa and 1% for bulimia nervosa in young women. Point prevalence of BED is at least 1% among all adults (Hoek and van Hoeken, 2003). The incidence of BN appears to have increased over the last half of the twentieth century and data support that incidence of BED may have increased over this time period as well (Hoek and van Hoeken, 2003; Hudson et al., 2007). Fewer data on subsyndromal and atypical eating disorders are available, but lifetime prevalence of AN together with anorexia-like syndromes is estimated at over 3% and of BN together with bulimia-like syndromes is estimated at 8% (CDC, 2006). Moreover, data from the 2005 Youth Behavioral Risk Survey (YRBS) reported by the Centers for Disease Control and Prevention (CDC, 2006) provide some insight as to how commonplace extreme weight-control behaviors are. Female students in the United States who participated in YRBS indicated that within the past month, 6.2% had engaged in self-induced vomiting or laxative abuse to control weight, 8.1% admitted to using diet pills or other products, and 17% fasted for a period of 24 h or more (CDC, 2006).
Female gender is a well-established fixed marker for AN and BN, with at least 90% of cases occurring among females (APA, 1994; Jacobi, 2005). BED is also significantly more prevalent among females, although the gender ratio is not as high (APA, 1994; Jacobi, 2005; Hudson et al., 2007).
Comparison of prevalence estimates of eating disorders across cultures suggests that BN may emerge exclusively in social environments characterized by exposure to so-called Western ideals. In contrast, AN has been reported across diverse social contexts, although the rationale for food refusal is tied to the local cultural context (Keel and Klump, 2003). For example, phenomenological variation in AN between Western and Asian populations is striking (e.g., an absence of fat phobia in the latter; Lee, 2001). Finally, population data have strongly suggested that acculturation, immigration, and modernization contribute to the vulnerability for an eating disorder (Becker et al., 2004).
Within the United States, data vary concerning the relative prevalence of eating disorders among Whites and Blacks. Whereas some large studies suggest they are less common among Blacks, other data suggest that rates of eating disorder symptoms may be quite similar across the major U.S. ethnic groups. In fact, rates of eating disorders may be even greater among Native Americans, Blacks, and Latinos when compared with non-Latino Whites (Crago et al., 1996; Fitzgibbon et al., 1998; Becker and Fay, 2006; Caldwell et al., 2006).
Etiology
Eating disorders have complex, multifactorial etiology, involving the interaction of genes and environment. More than 30 variables have been reported as putative risk factors for the development of eating disorders (Jacobi et al., 2004), including biological, psychological, and sociocultural factors. A taxonomy of risk factor typology and identification methods has been proposed, taking into account timing of risk relative to outcome, study design, and specificity, among other factors (Jacobi et al., 2004). Psycho-developmental risk factors that are common across eating disorders include elevated weight and shape concerns and dieting, early childhood eating and gastrointestinal problems, negative self-evaluation, sexual abuse and other adverse experiences, and general psychiatric morbidity. Factors specific to AN include perfectionism and obsessive-compulsive syndromes. Factors specific to BN include childhood obesity and early onset of puberty. In terms of sociocultural factors, there is strong evidence that social transition (e.g., transitional migration, urbanization, modernization), Western media exposure, and certain peer influences contribute to risk for eating disorders (Becker et al., 2004). Research on biological contributions has focused on genetic factors and neurobiological disturbances (e.g., altered serotonin). Family and twin studies support a strong genetic diathesis to eating disorders, with heritability estimates ranging from 58 to 76% for AN (an estimate similar to that of schizophrenia and higher than most other mental disorders), and 30–83% for BN. Molecular genetic studies have yet to identify well replicated susceptibility loci, a challenge made more difficult by nosological issues and lack of reliable, valid phenotypes. Vulnerability for the development of an eating disorder may also be related to disturbance in serotonergic activity. As such disturbance seems to persist following recovery, it remains unclear, however, whether such disturbance is a long-term consequence of an eating disorder, rather than a premorbid trait.
Assessment
Multidimensional assessment of eating disorders includes diagnostic interview, medical, nutritional, and family assessments, and self-report questionnaires. Diagnostic interviews can establish past and current eating disorder symptomatology, mental status including suicidality and self-harm, psychiatric comorbidities, including substance abuse, mood, and anxiety disorders, as well as personality disorders. A review should include the patient’s height and weight history, restrictive eating patterns, binge eating, purging and compensatory behaviors, and exercise habits. Assessment of body image is essential, although body image disturbance may manifest in different ways across patients. Another important aspect to assess is patient’s motivational status, given its influence on course, outcome, and treatment planning. Self-report questionnaires, helpful for ascertaining symptom patterns and progress in treatment, include measures of eating behaviors, dieting, and related beliefs and behaviors, and multidimensional aspects of body image disturbance. Assessment of medical status via full physical examination is strongly recommended, with particular attention to vital signs, physical status, cardiovascular and peripheral vascular function, and dermatological manifestations (APA Workgroup, 2006). Ongoing medical evaluation of changes in weight, cardiovascular indications, and electrolytes may be warranted. Dietary intake and deficiencies may be assessed through self-monitoring (i.e., food records) or interview. While self-monitoring is itself a therapeutic technique, the accuracy of self-reported intake has been challenged, and adherence can be a problem. Family assessment may be important, especially among adolescent patients or patients living with significant others. Family assessment is an opportunity to gather information about family dynamics, especially regarding the topics of food and weight, and also provide psychoeducation to family and significant others.
Course And Outcome
Peak incidence of AN and BN is in adolescence, whereas the onset of BED is typically in late adolescence to the early twenties (APA, 1994). However, clinical experience suggests that eating disorders are becoming common in prepubertal children and middle-aged adults. Patients with eating disorders are often quite conflicted about giving up their symptoms. While most say that they want to be free from disordered eating, many are fearful of gaining weight or finding alternate coping strategies to deal with stress or anxiety. As such, many are reluctant to seek treatment. Patients with AN often come to medical attention more quickly by virtue of low body weight and/ or change in eating and exercise patterns that are often noticed by friends and family. Individuals may protest when clinicians suggest that there is reason for concern; patients will often avoid being weighed or will wear layers of clothing to appear heavier. They may also drink excessive water or carry weights on their bodies to fool providers into thinking that their weight is normal. Similarly, patients struggling with BED may come to attention fairly quickly, particularly if they are overweight. Individuals with BN can be more difficult to detect, as they tend to stay within a relatively normal weight range. In addition, patients struggling with BN are often very reluctant to volunteer their symptoms due to shame. However, when savvy providers identify them, patients with BED and BN are far more likely to accept treatment than are patients diagnosed with AN. This is likely due to the fact that symptoms of binging and purging can be very distressing. Similarly, many individuals are motivated to lose weight for both cosmetic reasons and to avoid long-term health consequences. Those engaged in extreme dietary restriction, on the other hand, tend to take pride in their behaviors and are reluctant to change.
Even with treatment, the natural course of AN tends to be chronic, with symptoms relapsing and remitting several times over the years. However, some patients are able to sustain full recovery after a single episode of illness, sometimes without seeking any formal treatment. Early recovery tends to be more tenuous, with relapse more common in the first 2 years following treatment (Fichter et al., 2006). Relapses tend to be associated with periods of increased psychosocial stress and body image disturbance. Those who recover may continue to experience symptoms. While they may be able to maintain a healthy weight, some continue to observe very rigid behaviors around nutrition and exercise. Others begin binge eating and purging, and some may transition to full-fledged BN (Keel et al., 2005). However, remission rates do improve with time. Poor outcome is strongly associated with chronicity and severity of the eating disorder and mortality also increases over time.
Patients with BN may also have a chronic course, with periods of improvement followed by relapse. Transition to AN is rare, but many continue to engage in binge eating, purging, or compulsive exercise. Again, relapse is common in early remission, but rates of remission increase over time. Often, the frequency of symptoms decreases to a point where diagnostic criteria are no longer met. In a recent long-term follow-up study, 70% of patients no longer met DSM-IV criteria for an eating disorder 12 years after inpatient treatment for BN, 13% met criteria for EDNOS, 10% met criteria for BN, 5% met criteria for AN, and 2% died (Fichter and Quadflieg, 2004). Authors found that the presence of psychiatric comorbidity was the best predictor of outcome in this population.
Lifetime comorbidity with another psychiatric disorder is very common among individuals with an eating disorder, reported as 56% in AN, 95% in BN, and 79% in BED (Husdon et al., 2007).
Treatment
Multidisciplinary team treatment of eating disorders is the standard of care, with coordination among medical, nutritional, and psychiatric treatments. Services range from intensive inpatient programs to residential, partial hospital, day treatment, and varying levels of outpatient care, which may entail general medical treatment, nutritional counseling, individual, group, and family psychotherapy. Level of care should be determined according to a patient’s overall physical status, including body mass index and medical stability, as well as psychological symptoms and social circumstances. Hospital-level care is necessary in the context of serious medical complications or seriously impaired psychological function and may also be necessary when there is rapid or persistent decline in intake or weight, inadequate response to lower levels of care, or when psychosocial factors or comorbid illness interfere with effective outpatient management.
Across the eating disorders, psychotherapeutic interventions are the most effective and recommended firstline treatment. Psychopharmacologic treatment can be useful in augmenting psychotherapy for BN and BED but there is inadequate empirical support to recommend specific pharmacologic treatment for the primary symptoms of either AN or EDNOS. In the United States, only one pharmacologic agent has FDA approval for treatment of an eating disorder – fluoxetine for BN – and use of all other agents is considered off-label. The heightened risk for electrocardiographic QT prolongation among individuals with AN and BN requires that clinicians carefully consider risk of QT prolongation prior to initiating certain psychotropic agents in this patient population.
For adult patients with AN, few psychotherapies have been evaluated in randomized control trials and none have demonstrated effectiveness. In contrast to treatment for adults, however, treatment for adolescents with AN has shown promise, and family therapies with this population are recommended (Wilson and Shafran, 2005). Patients may benefit from interventions targeting comorbid anxiety, depression, and obsessive-compulsive symptoms, and psychotherapeutic interventions should comprise the main thrust of the treatment plan. Symptoms of depression and anxiety are exacerbated by the malnutrition that often accompanies eating disorders. Furthermore, individuals with low body weight are more susceptible to troublesome medication side effects (APA Workgroup, 2006), and many patients are reluctant to take medications that could potentially cause weight gain. Typically, slow, monitored, and actively managed weight gain is the most helpful intervention for these individuals. Clinicians should avoid introducing psychotropic agents known to suppress appetite. There are preliminary data to suggest that atypical antipsychotics (risperidone and olanzapine) may have some benefits in ameliorating symptoms of anorexia nervosa.
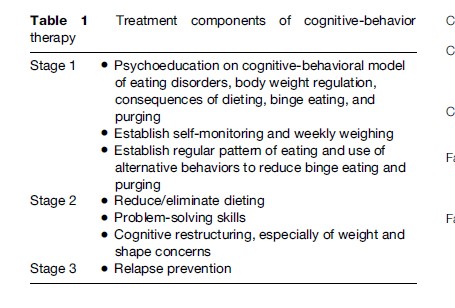
Cognitive-behavioral therapy (CBT) is the best-established of several empirically supported treatments for BN; numerous randomized controlled trials have shown reliably good outcome, low relapse rates, and superiority to treatment with antidepressants alone. CBT, described in a manual by Fairburn et al. (1993), is delineated in Table 1. Interpersonal therapy is also an effective treatment for BN. CBT and interpersonal psychotherapy (IPT) have been tested in both individual and group formats in randomized controlled trials and have empirical support (Wilson and Shafran, 2005). Fluoxetine at doses up to 60 mg per day is FDA-approved for the treatment of BN and is the best established pharmacologic agent for treatment of BN (Fluoxetine Bulimia Nervosa Collaborative Study Group, 1992). Combination therapy with both fluoxetine and CBT does seem to provide modest additional benefit (Walsh et al., 1997). Topiramate, an antiepileptic medication, has demonstrated efficacy in reduction of symptoms of BN (Nickel et al., 2005). Other classes of agents have shown efficacy (e.g., some tricyclic antidepressants and some monoamine oxidase inhibitors) but utility is limited by unacceptable side effects. Moreover, bupropion is relatively contraindicated in this population due to increased incidence of seizures in patients who actively binged and purged while taking this medication. CBT – both individual and group – is also the best-established treatment for BED. Topiramate has also been shown effective in the treatment of BED (McElroy et al., 2007) and several pharmacologic agents show promise, although further studies are necessary to establish clear treatment recommendations.
Conclusion
Eating disorders typically have onset in adolescence and young adulthood and are most prevalent among females. Although effective treatments have been developed, access to care for an eating disorder is unacceptably low and eating disorders often follow a chronic course. In addition, they can result in serious medical complications and are associated with high mortality compared with other mental illnesses. Optimal treatment is multidisciplinary and includes medical stability and nutritional counseling in addition to psychotherapeutic and psychopharmacologic interventions.
Bibliography:
- American Psychiatric Association (1994) Diagnostic and Statistical Manual of Mental Disorders, 4th edn. Washington, DC: American Psychiatric Association.
- American Psychiatric Association Work Group on Eating Disorders (2006) Practice Guideline for the Treatment of Patients With Eating Disorders. American Journal of Psychiatry 163(supplement).
- Becker AE and Fay K (2006) Socio-cultural issues and eating disorders. In: Wonderlich S, de Zwaan M, Steigar H, and Mitchell J (eds.) Annual Review of Eating Disorders, pp. 35–63. Chicago, IL: Academy for Eating Disorders
- Becker AE, Grinspoon SK, Klibanski A, and Herzog DB (1999) Eating disorders. New England Journal of Medicine 340: 1092–1098.
- Becker AE, Franko D, Speck A, and Herzog DB (2003) Ethnicity and differential access to care for eating disorder symptoms. International Journal of Eating Disorders 33: 205–212.
- Becker AE, Keel P, Anderson-Fye EP, and Thomas JJ (2004) Genes (and/) or jeans? Genetic and socio-cultural contributions to risk for eating disorders. Journal of Addictive Diseases 23: 81–103.
- Caldwell M, et al. (2006) National Institute of Mental Health Workshop on Eating Disorders. Bethesda, MD, 29 June 2006.
- Centers for Disease Control and Prevention (2006) Youth Risk Behavior Surveillance System: Adolescent and School Health. Atlanta, GA: http://apps.nccd.cdc.gov/YRBSS/index.asp (accessed January 2008).
- Crago M, Shisslak CM, and Estes LS (1996) Eating disturbances among American minority groups: A review. International Journal of Eating Disorders 19: 239–248.
- Fairburn CG and Bohn K (2005) Eating disorder NOS (EDNOS): An example of the troublesome ‘‘not otherwise specified’’ (NOS) category in DSM-IV. Behaviour Research and Therapy 43: 691–701.
- Fairburn CG, Marcus MD, and Wilson GT (1993) Cognitive behaviour therapy for binge eating and bulimia nervosa: A comprehensive treatment manual. In: Fairburn CG and Wilson GT (eds.) Binge Eating: Nature, Assessment, and Treatment, pp. 361–404. New York: Guilford Press
- Fichter MM and Quadflieg N (2004) Twelve-year course and outcome of bulimia nervosa. Psychological Medicine 34: 1395–1406.
- Fichter MM, Quadflieg N, and Hedlund S (2006) Twelve-year course and outcome predictors of anorexia nervosa. International Journal of Eating Disorders 39: 87–100.
- Fitzgibbon ML, Spring B, Avellone ME, Blackman LR, Pingitore R, and Stolley MR (1998) Correlates of binge eating in Hispanic Black, and White women. International Journal of Eating Disorders 24: 43–52.
- Fluoxetine Bulimia Nervosa Collaborative Study Group (1992) Fluoxetine in the treatment of bulimia nervosa. A multicenter, placebo-controlled, double-blind trial. Archives of General Psychiatry 49: 139–147.
- Harris EC and Barraclough B (1997) Suicide as an outcome for mental disorders. A meta-analysis. British Journal of Psychiatry 170: 205–228.
- Harris EC and Barraclough B (1998) Excess mortality of mental disorder. British Journal of Psychiatry 173: 11–53.
- Hoek HW and van Hoeken D (2003) Review of the prevalence and incidence of eating disorders. International Journal of Eating Disorders 34: 383–396.
- Hudson JI, Hiripi E, Pope HG, and Kessler RC (2007) The prevalence and correlates of eating disorders in the national comorbidity survey replication. Biological Psychiatry 61: 348–358.
- Jacobi C, Hayward C, de Zwaan M, Kraemer HC, and Agras WS (2004) Coming to terms with risk factors for eating disorders: Application of risk terminology and suggestions for a general taxonomy. Psychological Bulletin 130: 19–65.
- Jacobi C (2005) Psychosocial risk factors for eating disorders. In: Wonderlich S, Mitchell JE, de Zwaan M and Steiger H (eds.) Eating Disorders: Review Part I, pp. 59–86. Oxford, UK: Radcliffe Publishing
- Keel PK and Klump KL (2003) Are eating disorders culture-bound syndromes? Implications for conceptualizing their etiology. Psychological Bulletin 129: 747–769.
- Keel PK and Mitchell JE (1997) Outcome in bulimia nervosa. American Journal of Psychiatry 154: 313–321.
- Keel PK, Dorer DJ, Franko DL, Jackson SC, and Herzog DB (2005) Postremission predictors of relapse in women with eating disorders. American Journal of Psychiatry 162: 2263–2268.
- Lee S (2001) Fat phobia in anorexia nervosa: Whose obsession is it? In: Nasser M, Katzman M and Gordon R (eds.) Eating Disorders and Cultures in Transition, pp. 40–54. London: Routledge
- McElroy SL, Hudson JI, Capece KB, Fisher AC, and Rosenthal NR for the Topiramate Binge Eating Disorder Research Group (2007) Topiramate for the treatment of binge eating disorder associated with obesity: A placebo-controlled study. Biological Psychiatry 61: 1039–1048.
- Nickel C, Tritt K, Muehlbacher M, et al. (2005) Topiramate treatment in bulimia nervosa patients: A randomized, double-blind, placebo-controlled trial. International Journal of Eating Disorders 38: 295–300.
- Walsh BT, Wilson GT, and Loeb KL (1997) Medication and psychotherapy in the treatment of bulimia nervosa. American Journal of Psychiatry 154: 523–531.
- Wilfley DE, Wilson GT, and Agras WS (2003) The clinical significance of binge eating disorder. International Journal of Eating Disorders 34: S96–S106.
- Wilson GT and Shafran R (2005) Eating disorders guidelines from NICE. Lancet 365: 79–81.
- Fairburn CG, Cooper Z, and Shafran R (2003) Cognitive behaviour therapy for eating disorders: A ‘‘transdiagnostic’’ theory and treatment. Behavior Research and Therapy 41: 509–528.
- National Institute for Clinical Excellence (2004) Eating Disorders: Core Interventions in the Treatment and Management of Anorexia Nervosa Bulimia Nervosa, and Related Eating Disorders: Clinical Guideline 9. London National Institute for Clinical Excellence 2004. http://www. bps.org.uk/downloadfile.cfm?file_uuid=C1173310-7E96-C67FD396-ADF1B891FSA3text=pdf/.
- Shaw H, Ramirez L, Trost A, Randall P, and Stice E (2004) Body image and eating disturbances across ethnic groups: More similarities than differences. Psychology of Addictive Behaviors 18: 12–18.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








