This sample Bioethics Education Research Paper is published for educational and informational purposes only. Free research papers are not written by our writers, they are contributed by users, so we are not responsible for the content of this free sample paper. If you want to buy a high quality paper on argumentative research paper topics at affordable price please use custom research paper writing services.
Abstract
This entry focuses on bioethics education in the formation of healthcare professionals. The emergent paradigm is borne out by a centripetal model in whose center are ethics explicit activities – mainly courses in ethics and law along with small group practices of ethics case deliberation. In a broader circle, one finds a diverse, mainly experiential and situation specific activities in ethics-related competences, mainly empathy, communication, and self-reflection. In the periphery of the hypothetical model, one finds all aspects of healthcare education, which must be infused with “professional” conduct and awareness of ethical issues. There is a broad consensus that bioethics education should be spread over horizontally (e.g., across all disciplines and educational activities) and vertically (e.g., throughout the process of education from beginning to graduation).
Introduction
Teaching and learning are ubiquitous, found among animals as well. Like love, trust, and care, education is a fundamental, intuitive human concept, whose philosophical explication is quite elusive. In theories of education, there are three fundamental levels. The first is knowledge in the sense of recall intellectual knowledge. The second is a set of abilities or skills. The third is the cultivation of attitudes, which is part of the motivational and emotional dimensions of personal identity. Overall, the term competence refers to an integration of all three levels in a specific area, such as “communication with patients” and “diagnosis”. Whereas it is relatively easy to monitor progress in knowledge and skill, the cultivation of attitudes and competences is elusive, and spreads over long stretches of time, much beyond the range of ordinary quantitative research.
Every curriculum in medical education contains elements of medical ethics. It is hardly possible to separate medical education from education to ethical practice. The ever-growing bureaucratization of medicine and its subjection to legal oversight render formalization of ideas and programs indispensable to the contemporary practice of medicine.
A systematic inquiry study of education in bioethics begins with the following issues:
- What is “bioethics”/medical/clinical ethics?
- What is the corpus of knowledge, skill, and attitudes needed for the practice of a particular healthcare role (e.g., physician, expert physician, nurse, etc.)?
- When should ethics education take place and how much time should be dedicated to each phase of education? The settings of educational endeavors are a function of the time and timing, and vice versa.
- The questions of methodology – How to convey this corpus of knowledge and skill, and how to integrate ethics education with the broader healthcare curriculum and actual practice.
- Who are the persons and what are the processes responsible for the development, execution, and monitoring of education?
- Ethical problems related to education and to education in bioethics.
Education has always been perceived as much more than the passage of abstract knowledge from one person to another. While being target oriented (i.e., education to… education in.. .), education is mainly about the betterment of the person in the direction of excellence, the interiorization, and understanding of values through the undertaking of responsibilities. In liberal, humanistic education, these are the responsibilities of a free citizen in society. In bioethics, these are also the responsibilities of healthcare in professional and scientifically informed settings. It is about the seeding of motivation, identification, and moral fortitude (power of will). Because of the moral nature of medical practice, the often-stressful work conditions of clinicians and the direct and fateful bearings of practice on life, death, dignity, and integrity of persons, medical education and education in medical ethics pose special and substantial challenges.
The first challenge is to delineate a field of discourse on “education in bioethics” that does not overlap with medical education as such. Rather, one should also avoid an overlap with education in medical humanities (which emerged in the 1990s) and education in communication (e.g., “breaking bad news”), and similarly related dispositions and competences. While it is impossible to conceive of an ethical caregiver who is deficient in empathy, empathy as such guarantees neither moral judgments nor moral conduct. Education in bioethics builds upon successful education in related skills and traits, but ethics is irreducible to the sum of its psychological and social constituents.
Education is about socialization in a certain way of life, and professional education is about socialization into a certain role. Paradoxically, in addition to socialization, education in ethics must also inspire and empower criticism and reform of the way of life and the professional role itself. Hence, at the heart of ethics education, something is beyond integration in any role or culture.
Indeed, bioethics and formal programs in bioethics education have emerged as responses to horrific moral failures, as well as in reaction to criticism of deeply rooted practices of otherwise good and well-intentioned clinicians and scientists. Among the horrific failures, one may count the Nazi medical crimes, and the Tuskegee syphilis study; among the rejected practices, one may count withholding information from very sick patients, psychiatric confinement without due process of law, imposition of medically indicated treatment on nonconsenting patients, and exclusion of women from admission to medical schools. These, and many other reforms and initiatives have not resulted from mere advancement in emotional intelligence, but from rational, deliberative, and critical self-reflection, and have always involved fierce debates among all stakeholders.
History And Development
The history of medical education goes back all the way to Hippocrates and other sources from antiquity. This kind of education has always contained ethical and legal norms. Medical education in either ethics or humanities is absent from the 1910 Flexner port, a landmark document on medical education in the USA, and actually in the emergent scientific biomedical environment of the industrialized world. One reason for this lacuna in the Flexner Report might be that the cultivation of a robust character through humanistic education was considered the essence of the college system. Because a college degree was prerequisite by academic medical schools, educators considered formal college education in “sociology,” “economics,” and “psychology” as the moral foundations relevant to medical students. The first academic reflections on medical education, mainly the early articles in Academic Medicine (established in 1926), do not use the words “ethics” or “morals.” The authors advocate the extension of biomedical training into the college (pre-med) period, rather than the expansion of humanistic education to the clinical years. Within 50 years, this trend reversed, and the contemporary discourse on “bioethics” (= a word born in the early 1970s) education, and education in medical ethics and humanities as part of medicine (and other healthcare professions), became a chief concern in clinical medical education.
In continental education (i.e., mainland Europe), ethics education has developed in diverse academic settings. For example, in Germany, ethics has developed mainly within a very strong tradition of “history of medicine.” In Italy, ethics has been part of “legal medicine.” A recent comprehensive survey of new trends in ethics education in Europe has found a picture very similar to the one originating in the English-speaking world (Kennedy et al. 2013).
Bioethics education is an outgrowth of three recent developments of the past 40 years. The first is the rise of education as a distinct academic discipline, one with very strong statistical and applied orientations. The second is the growing awareness of the humanistic dimensions of medical practice and the ensuing flourishing of courses and activities in medical humanities and ethics. The third is the emergence of “bioethics” and medical ethics as discrete bodies of discourse and professional training.
Concepts
In care settings (and care ethics), we strive to act upon natural capacities such as sympathy, attentiveness, and recognition of the Other (i.e., nonsolipsism, nonnarcissism). One such capacity is self-reflection on circumstances in which reliance on a dominant moral emotion or drive to act might be inadequate, even immoral (Noddings 2013). Every curriculum in ethics education proper must prepare the student to discover such “moral moments” and confront them with the aid of bioethics as a corpus of knowledge, skills, and a social practice. Discussed here are three discrete steps.
- Sensitivity to moments of “friction” and doubt that brings forth recognition of a moral problem.
- Conscientious reflection on the problem.
- Deliberation aiming at a resolution with the relevant stakeholders.
Ideally, this whole process leads to restoration of routine care based on expected decisions, often automatic, and smooth actions. Yet the restored routine will be a little different, because it will embody deeper and more comprehensive integration of values, knowledge, and personal growth of the parties involved. This entails a movement from ethics in the sense of specific other-oriented duties to morality in the sense of the development of personal identity, responsibility, and social roles. Some authors believe that holistic acculturation comes first. They often call it “education to professionalism.” They also believe that once the professional character has been formed, appropriate responses to moral moments ensue, as if automatically. This educational model seems to mirror certain streaks in virtue ethics, in which identity and character antecedent and predicate specific behaviors. This approach conceives of education as holistic experience of growth through immersion in good practice accompanied by emulation of paragons. However, the more emphasis bioethics grants to critical skills, the less satisfactory the immersion model becomes.
A fundamental insight of contemporary bioethics is that even the most benevolent and kindest attitude does not guarantee genuine beneficence, especially benefit that is respectful of human dignity, alternative worldviews, and basic values of democracy. The ethical disposition is a critically reflective competence. Whereas education involves a great deal of imitation and feedback by experts, a morally attuned person should be able to criticize prevailing norms and reform well-established practices, when conflicts of values arise.
Indeed, a little after the nascent of “bioethics” as a word, style of discourse and academic discipline, a shift took place in education to medical ethics. This is well articulated by the 1987 Pond Report, a Nuffield Foundation project on education in medical ethics in the UK (Boyd 1987). According to the report, until the second half of the twentieth century it was widely held that ethical skills develop by “osmosis” from role-model practitioners to younger ones, while ethical judgment and matters of personal conviction and faith were beyond the consensus of medical education, the way it is conceived in a modern and secular state. However, when the Pond Report was published, a few new trends were gaining currency. First, a landmark study on the socialization of novice nurses demonstrated the presence of a pervasive “hidden curriculum,” the “osmosis” of habits and nonofficial rules, some of which were blatantly unethical, but they nevertheless dominated daily practice as matters of necessity and personal and professional “survival.” Second, the growing subjection of medical law and practice to the basic values of human dignity and human rights has posited a set of shared basic values that hedges the leeway for personal choice and cultural differences. Third, developments in medical education and disciplines, such as moral psychology, social psychology, sociology and communication, have shown that people may reflectively improve their own judgments and conduct, in line with their own authentic values. Hence, education in ethics is neither indoctrination (in the sense of making people unreflectively reproduce a given set of behaviors and opinions), nor invasion into the personal realm. It can and it should help the person achieve excellence, as much as training in athletics and in art may help people develop their own distinct capacities and voices.
The revolution in bioethics education is well articulated in a 2007 publication of a Wellcome Foundation Seminar on the topic (Reynolds and Tansey 2007). Even though both publications focus on the UK, they capture well a new paradigm in education to healthcare ethics. This paradigm contains the following elements.
- It is essential to cultivate awareness and knowledge of practitioners’ own thoughts, emotions, and judgments. Many authors believe that this includes a certain level of academic knowledge in history, sociology, psychology, and philosophy of medicine.
- It is also essential to develop fluency in the bioethical jargon, enabling practitioners to participate fruitfully in ethical deliberation. It is the medium allowing personal conscience to bear on joint decision-making.
- Bioethics education must be grounded in optimization of relevant activities and competences (e.g., role modeling, resilience to “burn out,” storytelling, communication skills) in ways that promote ethical conduct, rather than smooth out difficulties, and failures.
- Another key target is the promotion of an institutional ethical culture. Such culture creates conditions that promote ethical behavior.
- Because bioethics education is a young field of practice, it requires attention to secondary education, which is the education of the ethics teachers and clinical tutors in general.
Every curriculum in bioethics education must have specific goals. They usually fall in a middle way between attempts to cover all competences in “professionalism,” “ethics,” and interpersonal skills, on the one hand, and complete merger of ethics in broader curricula in the humanities and clinical skills, on the other. Whereas it is evident that deliberation does not exhaust ethical practice, experience and skill in deliberation are the most specific goals in bioethics education modules within curricula in healthcare. Put in other words, while all medical education programs aim at the cultivation of good care giving, the immediate and specific goal of education in bioethics is competence in ethical deliberation.
Specific Issues In Bioethics Education
This section surveys practices and ideas, which are both prevalent in existing programs and considered important by leading educators.
Syllabus. Content of bioethics education may be classified into a few categories.
The first is a list of values and value-related concepts. One such list is found in the UNESCO’s Bioethics Core Curriculum, which is posted in UNESCO’s website freely and fully. This program’s syllabus refers to: dignity and rights, autonomy and personal responsibility, consent, persons without capacity to consent, vulnerability and personal integrity, privacy and confidentiality, equality and justice, benefit and harm, nondiscrimination and nonstigmatization, respect for cultural diversity and pluralism, solidarity and cooperation. This is not a canon, but an example. Different rearrangements of the bioethics building blocks may occur in diverse circumstances of learning.
Whereas the values and related concepts are the warp of the bioethics discourse, paradigmatic cases (e.g., “end-of-life” issues) composite its weft. The values spread all over ethical discourse; the cases may vary according to the field of practice (e.g., nursing, dentistry, obstetrics). Some curricula expose the student to landmark historical cases (e.g., Tuskegee syphilis study).
Bioethics education should address conflicts of interests openly, extensively, and with psychological and moral depth. This involves personal issues (e.g., time needed for rest vs. time with a needy patient), economical aspects (e.g., financial incentives vs. the good of the patient), and institutional dynamics (e.g., the good of the patient vs. loyalty to peers and the “system”).
The second category is a list of concepts that are useful in critical understanding of healthcare related issues. Among such concepts, one may find “medicalization,” Talcott Parsons’ “sick role” and “professional role,” Erwin Goffman’s studies on medical institutions, Michel Foucault’s “biopower,” the “no-shame no-blame” institutional culture, and, recent, emergent ideas such as “quaternary prevention.”
The third category is a list of issues in local biomedical law. Although it is crucial that distinction and differences between law and ethics be part of the syllabus, it is also important to assist the students to connect the disciplines as complementary frameworks of normativity.
The fourth category rises above the levels of concepts and their arrangement and moves into the syntax and style of bioethical reasoning. This relies on other philosophical skills, such as the capacity to construct arguments and criticize them. Short and basic curricula cannot but touch the art of rational deliberation. Advanced programs should refer to specification, casuistry, balancing of values, syllogism, the avoidance of undue rhetoric (e.g., hyperbole, ad-hominem, straw-man strategies), moral imagination, mainly in the use of hypothetical variants of the situation under discussion, narrative skills, and hermeneutics. Academic education in ethics, such as found in philosophy departments, exposes the students to a diversity of ethical theories (e.g., utilitarianism, virtue ethics) and metaethical issues (e.g., the nature of the “good”). Paucity of resources (mainly academic hours) usually do not allow the incorporation of this kind of education in healthcare curricula.
Time and place. There is a broad consensus that ethics education should be spread over horizontally (e.g., across all disciplines and educational activities) and vertically (e.g., throughout the process of education from beginning to graduation). In line with the convention of instituting “basic science” prior to clinical teaching, many curricula offer the academic courses in ethics early on, entrusting the ethics aspects of clinical years in the holistic modules of clerkship and immersion in practice. Early familiarity with concepts and ideas empowers the students to engage themselves in critical reflection on their overall experience, especially in the clinic.
However, certain aspects of moral formation depend on personal maturity and the actual experience of moral challenges. The more advanced and mature the student is, the more receptive he or she becomes to the incorporation of abstract academic knowledge in practice. Hence, a “vertical approach” to bioethics education is like a spiral, seeding formal knowledge first, and then revisiting it in later stages with increased sophistication and integration. For example, a first year student should learn about the idea of human dignity; a mature graduate should be able to employ it as part of comprehensive discussions of a clinical cases.
It is crucial that clinical curricula designate space and time for bioethics. It is highly advisable that in such dedicated time students practice oral deliberation as well as written assignments. Both modalities should simulate the real-life practice of ethics rather than academic tasks. For example, deliberation should resemble sessions in ethics committees, rather than a debate club; written assignment should resemble ethics sections in grant applications, rather than college papers.
Methodologies. For centuries, medical education relied on two methodologies – podium lecturing and bedside observation and apprenticeship. Recently, many novel pedagogical ideas have entered medical education. In this section, the prevalent methodologies are surveyed.
(1) Lectures. Podium lecturing has fallen from grace in contemporary medical education. Students usually dislike classroom learning and abstract theory; experts in education criticize its unidirectional and authoritative style. However, lecturing is still common owing to a few strong advantages. One person addressing dozens (sometimes hundreds) of students facilitates the foundation of common knowledge, language, and practice. Medical schools and other educational programs, who are often short in money and in teachers, may employ few high level scholars, allowing all students to hear firsthand, at least for a few times, leaders in the field. In addition to the respect paid to both students and program, lectures are openings to future interpersonal interactions between interested students and top-level faculty.
The flourishing of e-learning over distances and TED talks has revived podium lecturing. Even though education in ethics requires interpersonal interaction, one may learn from successful Internet lectures that it is possible to improve didactics and render lecturing a highly engaging and efficient modality of learning.
(2) Role modeling. Inspired by sociologist Talcott Parsons, role modeling is a multidimensional concept. It may be divided into a well-defined core, which seems to be noncontroversial, and variations used in practice (Kenney et al. 2003). The core definition of education through role modeling contains the following elements:
- A competent and experienced practitioner. Especially in relation to ethics education, this “role model” should be rounded in diverse, if not all practice-related competencies.
- The practitioner is engaged in a variety of real-life activities, for example, interview and physical examination of a patient rather than demonstration on a volunteer.
- Would-be or novice practitioners are present, thus witnessing and experiencing the practice first hand, as observant-learning participants.
- The participant-observation occurs with sharing of responsibilities. Indeed, medical students are part of the team, drawing blood, taking interviews, and the like.
- An opportunity to reflect critically on the experience post factum. This is crucial for the cultivation of proper balance between reliance on heuristics and critical, even non-conformist, reflection.
Some programs bring together “role models” and students for discussions in neutral spaces, such as private meeting rooms; others build on long-term arduous copresence of younger and senior practitioners. Role modeling may spill from one role to another; medical students may benefit a lot from the role modeling of a nurse mentor. Some programs contain ward-based teaching, in which the ethics instructor, often accompanied by the clinical tutor and other team members, discusses ethical issues at the bedside, very similar to the teaching of clinical skills.
The well document “success bias” may render students susceptible to emulate successful doctors (e.g. famous, rich and powerful), even if luck, even immoral conduct has made them so.
In actuality, few “role models” are icons of ideal practice. Some are exemplary under stress; others excel at listening. Almost every “role model” has moral and other weak spots. Rather, uncritical reproduction (emulation) is morally dangerous even when the role model’s conduct is illustrious. A realistic approach to mentoring acknowledges a differentiation of apprenticeship from role modeling. Apprenticeship is emulative learning through practice alongside more experienced and capable practitioners. Role modeling is about critical learning from examples of real-life behavior of experienced and good practitioners. Because human behavior is highly complex, nuanced, and partially unconscious, sometimes there is no alternative to personal witnessing of the learned conduct from a position of shared responsibilities. However, in genuine role modeling, the lesson taken is at a higher level of abstraction from the behavior observed. Role modeling is distinct from exemplary demonstration or a set of demonstrations, and from all other forms of “situated” and “experiential” learning from experienced and successful performers. Indeed, many clinical skills and professional manners are acquired through apprenticeship like modes of precise repetition and expert feedback. The essence of bioethics education through role modeling is interiorization of insights and attitudes critically filtered through numerous, arduous, long, and diverse sessions of observation-participation. Historically, a novice would apprentice with one master. However, learning ethics through role modeling requires immersion in the practice of a few practitioners, as to empower the learner to develop his or her personal modes of conduct. Almost every practitioner cherishes in his or her heart one or more role models who were a source of extraordinary inspiration and learning. Whereas it is a blessing to come of age along such paragons, it is impractical to design curricula on ideal and idealized sporadic experiences.
(3) Small group studies. Education and teaching in small groups have many advantages, allowing significant, active engagement of every learner, greater personal attention of mentors, facilitation of team work, and development of related skills. It also seems that work in small groups supports constructivist growth (i.e., every student develops his or her talents, blazes his or her unique pathway of growth and understanding). Small group studies, usually centered on problem-based learning (PBL) and reliant on self-study at home, have become increasingly popular in medical education. In bioethics education, small group work may involve two additional kinds of learning experience.
The first constitutes ethics-related activities such as Balint groups, cultural awareness activities and communication workshops.
These activities are at the heart of many curricula in medical education, often under the title “professionalism,” and experiential learning.
The second kind of small group activities in bioethics education are sessions of moral deliberation, whose structure may vary from program to program. For example, some programs contain role-playing (e.g., one student prepares the role of a “chaplain”; another is “the patient’s brother,” etc.), performance of deliberation in front of the whole class, parallel sessions of variants of one case, and the like. Owing to the centrality of deliberation in bioethics and bioethics education, it is crucial that teachers and students be aware of the differences between Balint style small group and sessions of deliberation. Arguably, Balint style activities also help prepare students and practitioners to become more adept at ethical deliberation and cope better with the burden or moral responsibility. Nevertheless, the activities and their respective purposes are quite distinct. This is shown in Table 1.
(4) Simulation. In the past 15 years, simulation has been gaining currency in medical education. Simulation is especially helpful in the cultivation and evaluation of algorithmic skills such as resuscitation, surgical procedures, and safe driving. Simulation is also helpful as an alternative to the distressful experience of bedside learning in emotionally loaded moments, such as “breaking bad news.” Because it may not be polite to ask some patients consent to videotape actual sessions and perform other interventions that might boost the learning experience and the monitoring of its quality, such as OSCE (Objective Structure Clinical Examination), simulation allows training with less burden on patients. A third context where simulation is especially helpful is in the preparation of practitioners to rare occurrences, which students are not likely to meet in real-life training. It is less clear to what extent simulation might really simulate the emotional and relational intensity of direct encounters with dying patients, battered wives, birthing teenagers, and many similar crises. Because simulation is very expensive, it is unclear which kind of simulation is cost effective.
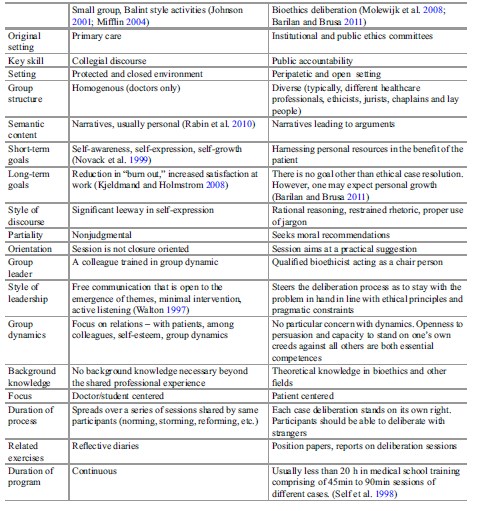 Table 1. Balint style small group activities and group deliberation: a comparison
Table 1. Balint style small group activities and group deliberation: a comparison
Designing a bioethics curriculum. One may expect the cardiology department, for example, to assume responsibility over the entire curriculum in cardiology. However, education in medical ethics is the task of all parties involved in medical education. Bioethicists and similarly qualified academicians may design and lead specific programs, such as academic courses, and sessions of deliberation. Little should be expected from a learning environment that relegates all ethics teaching to one group of practitioners.
From an ethics perspective, curriculum development is a centripetal layout encompassing all medical education (see Fig. 1). In an inner circle, there are curricula in ethics related modules. At the core, we find specific modules in ethics that are both differentiated from and continuous with all the rest. In many programs, a basic course in ethics should suffice in an academic healthcare program in medicine, nursing, and other healthcare professions. Most programs offer much less. Small group activities in ethical deliberation are integral to the program’s core.
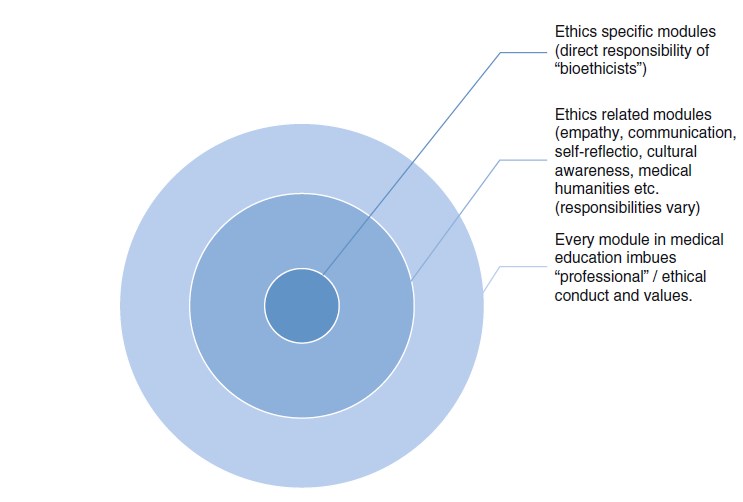 Figure 1. The centripetal model of ethics education in medical education
Figure 1. The centripetal model of ethics education in medical education
It would be highly unusual if a senior and respected endocrinologist undertakes teaching in cardiology. But many leaders and curriculum developers in ethics are enthusiastic professionals with little formal background in ethics. The encouraging things about this odd situation is that medical ethics is not the turf of a coterie of dedicated experts, and that so many distinguished professionals care to work in ethics education. The downside of this phenomenon is that in the contemporary healthcare setting, motivation, earnestness, and rich clinical experience rarely suffice. The most devoted and opinionated may not be the best qualified and knowledgeable. Ironically, in the face of growing awareness of “evidence-based practice” and the rigors of scientific research, medical educators often cling with zeal to didactic methods and educational approaches that lack “evidence-based” substantiation. The ever-growing popularity of ethics in curriculum development in medical education is also associated with numerous revisions of educational programs and torrents of novel initiatives and ideas. Overall, it seems that a good bioethics curriculum is the product of pragmatic use of all available resources in light of theory, in both medical education and bioethics. Modes of evaluation and revision need be part of the program and may require very long-range visions.
Curricula and syllabi do not exhaust the growth of conscientious and morally capacious caregivers. A significant body of research in social psychology shows that behavior is no less a product of the given human and material environment and physiological conditions (e.g., social dynamics, noise, sleeplessness) than character traits (Merrit and Doris 2012). Hence, a comprehensive vision of bioethics education is a dialectic and revisionary process in which the environment (i.e., faculty, material conditions, and institutional culture) and students change and grow interactively. The faculty bears the triple responsibility for patient care, education of young practitioners, and self-care.
Ethical Issues In Bioethics Education
Education, academic education, medical education, and education in medical ethics involve a diversity of ethical issues. Two key issues that are more specific to medical education and its ethical aspects relate to balancing selection with formation, and balancing duties to patients with duties to the students (and, indirectly, the students’ future patients).
Because the demand to enter medical schools is high, many programs screen out candidates, seeking those blessed with empathy and graced with emotional and social intelligence. Rarely do medical educators expel students for lack of professional behavior.
Selection procedures suffer three fundamental weaknesses. The first is legitimization. Second weakness is lack of validated selection methodology, even by prevailing criteria. Ultimately, one may argue that the formation of healthcare providers is a matter of education rather than selection; that with the exception of a small minority of persons with personality disorders and similarly extreme problems, everybody who cares to be a healthcare professional may become one, provided he or she receives proper education. Healthcare involves very diverse roles and competences. Even within the medical profession, it is almost impossible to pile up together the “professional” conduct of an administrator, family doctor, neurosurgeon, and an imaging specialist. Because talent is rare and diversity of cultural background key to just and respectful care, it might be wise to open the ranks to the gifted from all walks of life, and let education fill up the gaps in knowledge, empathy, communication, and other relevant competencies.
Patients often expect top quality care and avoidance of risk that may be associated with exposure to novices, while seniors have the dual duty of care and education. Informed consent does not penetrate the heart of the dilemma, because patients have little choice, and because nobody might know how to set the proper balance between teaching on the one hand and safety and respect on the other. A possible clue may come from seeing education and medicine as different manifestations of care. Students are less vulnerable, but their education might bear on the health of many future patients.
Conclusion
This entry focused on bioethics education for healthcare professionals. This special kind of education has some unique features in medical education. Bioethics education is both about socialization in a profession and awareness of the personal moral duty to revisit and often revise professional norms, institutions, and practices. Bioethics education is also an act of care, within a broader context of cares. Whereas medical education is typically modular (e.g., physiology, cardiology), there is a consensus that bioethics education should be spread “horizontally” and “vertically” and thus be present somehow in every educational module. This very ambitious and holistic calling needs anchoring and balance in a gradient of ethics oriented modules. In it, we find ethics-supportive modules, such as in communication, and medical humanities. At the core tier, one finds the theoretical and practical preparation of the learners for participation in ethics deliberation. This is a specific and sizeable target. Additionally, there are strong reasons to believe that work towards this target has a unique potential of penetrating all aspects of medical education and of radiating inspiration and moral power both inwardly (personal conscience) and horizontally (ethical patient care as a product of responsible team work), as well as outwardly (public accountability and global responsibilities). The differentiation of bioethics education from medical education is a novel trend. Like medical education in general, it is about helping practitioners care for their patients; but it also helps them flourish as colleagues and persons.
Bibliography :
- Barilan, Y. M., & Brusa, M. (2011). Triangular reflective equilibrium a conscience-based method for bioethical deliberation. Bioethics, 25, 304–319.
- Boyd, K. M. (Ed.). (1987). Report of a working party on the teaching of medical ethics – Chairman Sir Desmond Pond (The Pond Report). London: IME Publications.
- Johnson, A. H. (2001). The Balint movement in America. Family Medicine, 33, 174–177.
- Kennedy, C., Lilley, P., Kiss, L., Littvay, L., & Harden, R. (2013). Curriculum trends in medical education in Europe in the 21st century. Report to AMEE 2013 Conference Participants www.medine2. com/Public/docs/outputs/wp5/DV5.18.1_CURRICULUM_TRENDS_FINAL_REPORT.pdf
- Kenney, N. P., Mann, K. V., & MacLeod, H. (2003). Role modeling in physicians’ professional formation: Reconsidering an essential but untapped educational strategy. Academic Medicine, 78, 1203–1210.
- Kjeldmand, D., & Holmstrom, I. (2008). Balint groups as a means to increase job satisfaction and prevent burnout among general practitioners. Annals of Family Medicine, 6, 138–145.
- Merrit, M. W., & Doris, J. M. (2012). Character. In J. M. Doris (Ed.), The moral psychology handbook (pp. 355–401). Oxford: Oxford University Press.
- Mifflin, B. (2004). Small groups and problem-based learning: Are we singing the same hymn sheet? Medical Teacher, 26, 444–450.
- Molewijk, A. C., Abma, T., Stopler, M., & Widdershoven, G. (2008). Teaching ethics in the clinic: The theory and practice of moral case deliberation. Journal of Medical Ethics, 34, 120–124.
- Noddings, N. (2013). Caring: A relational approach to ethics and moral education (2nd updated ed.). Berkeley: University of California Press.
- Novack, D. H., Epstein, R. M., & Paulsen, R. H. (1999). Towards creating physician-healers: Fostering medical students’ self-awareness, personal growth and wellbeing. Academic Medicine, 74, 516–520.
- Rabin, S., Maoz, B., & Elata-Alster, G. (2010). Doctors’ narratives in Balint groups. British Journal of Medical Psychology, 72, 121–125.
- Reynolds, A. M., & Tansey, E. M. (2007). Medical ethics education in England 1963–1993. London: The Welcome Foundation.
- Self, D. J., Olivarez, M., & Baldwin, D. C. (1998). The amount of small-group case study discussion needed to improve oral reasoning and skills among medical students. Academic Medicine, 73, 521–523.
- Walton, H. (1997). Small group methods in medical teaching. Medical Education, 31, 459–464.
- Barilan, Y. M. and M. Brusa (2013) Deliberation at the hub of medical education: beyond virtue ethics and codes of practice. Medicine Healthcare and Philosophy 16:3–12.
- Campbell, A. V., Chin, J., & Voo, T. (2007). How can we know that ethics education produces ethical doctors? Medical Teacher, 29, 431–436.
- Emerich, N. (Ed.). (2013). Medical ethics education: An interdisciplinary and social theoretical perspective. New York: Springer.
- Lehnman, L. S., Kasoff, W. S., Koch, P., & Feldman, D. D. (2004). A survey of ethics education at U.S. and Canadian medical schools. Academic Medicine, 79, 682–689.
- Mattick, K., & Bligh, J. (2006). Teaching and assessing medical ethics: Where are we now? Journal of Medical Ethics, 32, 181–185.
- Sirrat, G. M., Johnson, C., & Gillon, R. (2010). Medical ethics and law for doctors tomorrow: The 1998 consensus statement updated. Journal of Medical Ethics, 36, 55–60.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.






