This sample Equality and Equity Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of research paper topics, and browse research paper examples.
Abstract
Three common “Es” have high ethical and political content for health policy: efficiency, equity, and equality. This research paper examines the links between the three, with especial attention given to (a) the claimed conflict between efficiency and equity, (b) the equity of inequalities, and (c) the conflict between six equity principles: equal health, equal health gain, equal value of additional health, maintaining existing distributions, allocation according to need, and equal per capita resources. Conclusions include: efficiency and equity do not inherently conflict, an inefficient allocation can be equitable, an efficient allocation can be inequitable, an inefficient allocation can become more efficient without increasing inequity, what is equitable often requires inequality in health and inequality in resource distribution per capita, equality in health requires inequality in resource allocation, equality in resource allocation typically leads to inequality in health, and allocation according to need typically leads to inequality in health.
Introduction
Three common “Es” have high ethical and political content for health policy: efficiency, equity, and equality. Having an efficient health-care system is morally important because health care is one important element that determines people’s health – and good health is a central part of both individual and societal well-being: good both for its own sake and because it enables individuals and communities to achieve other good things that contribute to well-being. Health does not equate to well-being, despite a famous World Health Organization (1948) axiom to the contrary (“Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity”), but it is usually a necessary condition for it. This is particularly true in poor counties and the many poor communities that exist in rich and middle-income countries.
There can be no doubt that a principal (though not the only) objective of health-care systems is to maximize health. In the UK there has been ministerial authority for that, for example, “The purpose of the NHS [National Health Service] is to secure through the resources available the greatest possible improvement in the physical and mental health of the people of England” (Department of Health 1996). Although it is never expressed quite like this, the underlying axiom is nearly always that “other things equal, more health is always to be preferred.” The more interesting, nonfactual, ethical assertion is that systems of heath care ought to prefer more health to less (other things equal). A related question is whether this objective is in conflict with the pursuit of equity. We shall identify five ideas of an equitable distribution of health and explore how these may conflict with the pursuit of the “underlying axiom” (i.e., with “efficiency”).
The ethical underpinnings for maximizing population health (or at any rate for increasing it) lie in the importance of good health for people to lead flourishing lives, which is taken as an ultimate good. In general, along with the idea that flourishing is an ultimate good is the understanding that good health is normally a necessary condition for it. In short, health is needed in the twin senses that it is both necessary (as a matter of fact) and that it also serves an ethically commendable end. This gives an otherwise merely technical relationship between a means (health) and an end (flourishing) its ethically persuasive quality and raises the need for health care to high ethical significance (in a way that is not true for my need for a Rolls-Royce, even though owning a “roller” would undoubtedly be an effective way of achieving one of my life’s ambitions: impressing my students).
To take the argument further, health care (including medical care) is often a necessary condition for realizing better health, though not always sufficient. If so, health care too is needed (i.e. is necessary if improved health is to be attained), and it too derives an ethically compelling character from the ethicality of the flourishing that is the ultimate good. So, not only may it be reasonably assumed that individuals want health care, they also need it, with all the moral weight that the word “need” carries in the context of social policy. If all that is accepted, promoting population health is an ethical objective, and so is “being efficient,” in the sense that the resources used in health care are used to promote health to the greatest possible extent and with the least sacrifice of other wanted and needed entities. As a shorthand, let us term the “promotion of health to the greatest possible extent” (for a given resource commitment) “health maximization” (subject to resource constraints).
Fairness, or equity, also acquires a high priority and for the same reasons. If health is of such moral importance, then its distribution too must be morally important and so must the distribution of health care. But what is it to be “equitable”? And can we integrate considerations of equity with those of health promotion or “efficiency”?
Equity
The treatment of individuals is invariably judged to be inequitable if it is capricious or relates to irrelevant characteristics. This is common to all notions of equity. Commonly cited irrelevant characteristics of this sort include race, religion, gender, ethnicity, and gender orientation. These may sometimes become relevant – for example, dietary restrictions on medical grounds or grounds of religion may be regarded as legitimate grounds for patients to be treated differently. These are exceptions, however, to the general rule. What is less frequently perceived is that equality and equity, and inequality and inequity, are not the same, although they are intimately related. At the most general level, equity in health care is held to require that patients who are alike in relevant respects be treated in like fashion and that patients who are unlike in relevant respects be treated in appropriately unlike fashion. In short, there can be equitable inequalities. Giving more resources to the more needy is an example of an (possibly) equitable inequality. These requirements are usually referred to as horizontal and vertical equity and derive from Aristotle.
Horizontal equity requires the like treatment of like individuals and vertical equity requires the unlike treatment of unlike individuals, usually in proportion to the differences between them. Suppose that need is selected as the only relevant factor, then the two principles would imply that like needs should receive like attention and resources (horizontal equity) and that greater needs should receive greater attention and resources (vertical equity). Horizontal and vertical equity considerations apply also to entities other than health. One closely related entity is the financial contribution to health care. A horizontal principle here might be “equal contributions from households having an equal ability to pay,” and the corresponding vertical principle is “higher contributions from households with a higher ability to pay.” These are (by these criteria) fair inequalities. A fair inequality is one that meets the test of vertical equity. A classic Marxist political slogan combines two vertical criteria: to each according to their need, from each according to their ability.
Efficiency
Some countries make their commitment to efficiency explicit. Many do not. Nonetheless, it will be taken for granted that health-care efficiency, in the form of using health-care resources, like the health-care workforce (human knowledge and understanding, human skills) and capital goods (buildings, equipment), is a good and ethical thing. Inefficiency, as when more people are used to accomplish something than is necessary, or a more expensive medicine is prescribed when a less expensive one would be no less effective, or more highly skilled staff are used when less highly trained individuals would be at least as good, is a bad and unethical thing. The main reason for taking this view is that the same chain of reasons why health care is instrumental for health and health is instrumental for flourishing applies to being efficient in producing health. Being inefficient implies that population health is less than it could be with the available resources. Given the moral significance of good health, to tolerate such a state of affairs would require a powerful countervailing argument. Such arguments undoubtedly exist. For example, if workers in the health system were outrageously (or even modestly) exploited, and better pay and conditions would reduce the amount of health care a given budget could produce, then a reduction in health (even that of the workers in question) might be judged a price worth paying.
Although efficiency is a minor focal point of this research paper, it provides a useful point of departure, partly because the reasons why efficiency matters morally are basically the same reasons why equity, which is our main topic, also matters morally: efficiency ensures there is as much of the ethically relevant human characteristic “health” as can be obtained from the resources available; equity ensures that the same ethically relevant characteristic is as fairly shared as it can be. Both derive their ethical significance from the significance of health for the flourishing life. There are many principles of equity that are worthy of exploration and clarification. However, there are questions of equitable health-care financing, equity in the ownership of health-care resources, equity in accessing career opportunities in health care, or equity in policies concerning the non-health-care determinants of health, like the equity of the distribution of purchasing power, or good quality housing, or good social care, or clean air, or workplace safety, or political influence but none of these are discussed here. Ethical issues relating to processes of health care are also excluded, for example, issues of accountability (whose and to whom and for what?), transparency of decisions (why were decisions made as they were, by whom, with what evidence in support, and what values embodied?), and participation (who may participate in decision making at various levels from the doctor-patient decisions to public policy decisions, who may be consulted, who has a vote or a veto?).
Values And Equity
It is common to refer to, and applaud, “evidence-based” decision making. In truth, however, few if any decisions can ever be truly evidence-based. No more can they be truly only ethics-based. Good decisions do indeed need to be informed by evidence and a good appreciation of how variable and contestable evidence can actually be; and they need also to be informed by values and good appreciation that values are not always shared, may conflict, and vary in moral worth. Both sets of issues require (morally, politically) deliberation between those likely to be affected by the decision (commonly referred to as “stakeholders”) and prior “constitutional” decisions about the suitability of various processes involved in such consultation and deliberation.
Health inequities are of concern in most rich countries. The problem is far more pressing in low and middle-income countries. In 2012, the under-five mortality rate in low-income countries was 82 deaths per 1000 live births – more than 13 times the average rate in high-income countries. Global life expectancy at birth among men ranged from a high of 75.8 years in high-income countries to a low of 60.2 years in low-income countries – a difference of 15.6 years. For women, a gap of 18.9 years separates the life expectancy figures in high-income countries (82.0 years) and low-income countries (63.1 years). These are averages. Within the low-income countries, there are figures far worse than these. These huge inequalities in health appear in all measures and for all age groups. There are huge inequalities in the distribution of and access to health care, as well as huge inequalities in health itself. The availability of public and private money for health care is woefully inadequate in the face of the need. All the more important, therefore, is what resources there are for health care are used with maximum effect and to address at least the worst avoidable inequalities.
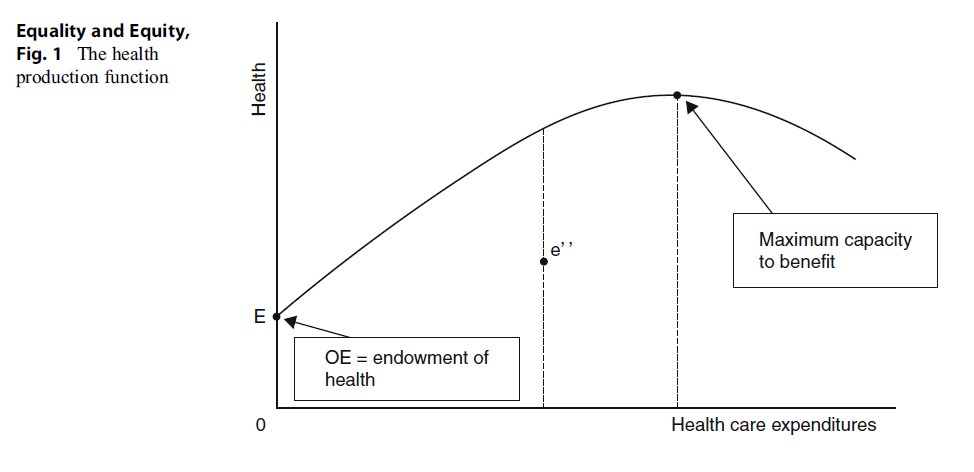 Figure 1. The health production function
Figure 1. The health production function
Yet one of the sad truths about health and health care in low and middle-income countries is that policy makers are constantly bombarded with claims – many from health economists and public health physicians – for the inclusion in public health plans of interventions whose only virtue is that they are effective. But being effective is not enough. Thousands of interventions are effective but not all – far from all – can be provided. Most of these interventions are simply not effective enough to be included, and even quite effective interventions may not be cost-effective. Childhood interventions, particularly vaccinations, often have the greatest impact per dollar on health. In sub-Saharan Africa, for example, rotavirus vaccination has been associated with a cost per disability-adjusted life year (DALY) averted of $43, and treatment of severe malnutrition costs $53 per DALY averted. Even within HIV, prevention of mother-to-child HIV transmission costs below $150 per DALY averted using available interventions, yet a large coverage gap remains across all low and middle-income countries. These high-impact and highly cost-effective interventions are seriously under-provided, while advocates routinely make recommendations on the basis of absurdly high cost-effectiveness thresholds, aiming to promote access in poor communities to new and more expensive therapies with cost-effectiveness ratios ten times worse than these. Poor countries have lists of so-called essential medicines including controversial drugs such as bevacizumab in addition to paclitaxel and carboplatin for treating ovarian cancer and ranibizumab for treating macular eye disease. The first of these is regarded as not cost-effective by the National Institute for Health and Clinical Excellence (NICE) in the context of England and Wales, and the second is recommended only if the manufacturer offers substantial discounts. These, in other words, are “bad buys” in one of the world’s richest countries. They stand, nonetheless, on poor countries’ lists of “cost-effective” “essential” medicines. These depressing facts reveal a carelessness of attitude to efficiency and equity in countries where they are of the utmost importance.
At this point the reader might throw hands in the air and declare that it is all too complicated, too awry, too technical, and altogether too difficult to see clearly what should be done. While answering the question “what should be done?” always requires its consideration in the local context, with local history, local values, locally available budgets for health care, and other distinguishing marks of local identity, being clear at the level of principle and making clear distinctions is less subject to such local variation. The procedure in the rest of this research paper will be to build as simple a model as possible in order to explore the relationships between efficiency, equity, and equality, exploding some myths as we go along and identifying helpful ways of thinking. A simple model of a health-care system is used to illustrate what is meant by both efficiency and equity.
A Simple Model Of Efficiency And Equity
We begin with the idea of a health production function that links aggregate health-care expenditures to some index of population health. The production function shows the capacity of a group (or an average individual) to benefit from changes in some specified determinant of health. Here, it is health care, as represented by healthcare expenditures. The production function is a measure of the effectiveness of health-care expenditures in terms of their impact on the health of a population. Such a function is depicted in Fig. 1. The curve from point E shows how health rises as health-care expenditures rise, enabling additional treatments to be deployed and for existing interventions to be scaled up across the population – but at a diminishing incremental rate, additions to expenditure add to health, but at a falling rate per dollar as, for example, less productive interventions are used, and harder-to reach groups are covered. Point E is the endowment, or starting point, of current health or the counterpart to the burden of disease. It is determined by existing factors and measured by an appropriate generic state-of-health indicator such as the quality-adjusted life year (QALY) or averted DALYs. The peak of the curve represents the maximum ability to benefit from additional expenditures on health care, beyond which lies a range of iatrogenesis, as further health-care expenditures actually reduce average health. Needless to say, we are for practical purposes concerned only with the rising section of the health production function. The curve locates the maximum impact on health, or the burden of disease, that any given rate of additional expenditure can have, given the available technologies. The production function therefore embodies an assumption of cost-effectiveness: that more resources than are necessary for achieving an outcome are not used. At point e’, for example, the system is generating only 50 % of its potential health gain, and it cannot therefore be a point on the production function. It is inefficient.
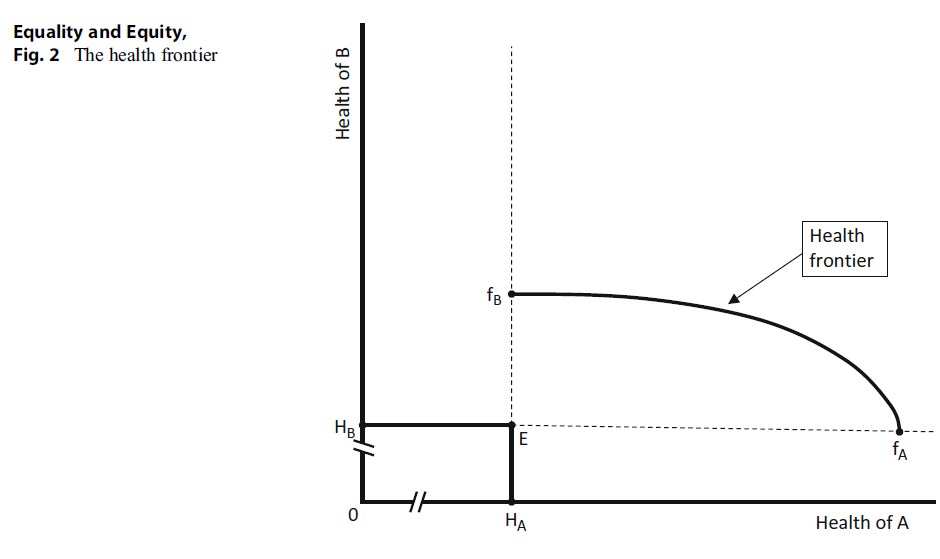 Figure 2 . The health frontier
Figure 2 . The health frontier
Let us suppose that such curves exist, at least in principle, for all sections of the community and that they typically vary from disease to disease, from social and economic context to context, and from one average type of patient to another. We might consider production functions for people with chronic orphan diseases for whom treatments are not very effective and are usually very costly, relative to others. Or we might consider the rural poor in a low-income country, for whom the most effective treatments are very effective and also quite cheap, again compared with the well-to-do urban population in that country, or a group of multiply deprived people compared to the rest of the population, or just simply the “poor” and the “rich” or the “sick” and the “well.” This is, of course, a stylization of reality. Its purpose is, through simplifying and removing inessential details, to enable us to clarify the kinds of impacts that different allocations of expenditure may have and to compare frequently met generic concepts of equity in health and health care.
In Fig. 2, the health of two such different groups is measured on the two axes. The point E again indicates current health, in this case, its distribution between the two. The deprived group (B) has on average the health level HB, and the relatively healthier group A has on average the level of health HA. The breaks (//) indicate equalsized gaps in the scale of expenditure just to keep the figure on the page. We now suppose that there is additional resource available (say, the budget for public health care rises or insurance premium income rises). This means that the health of both groups can be increased. Given the production function for the As, if all the extra budget were spent on them, the maximum increase in health possible is the distance EfA. Were it all to be spent on the Bs, the maximum increase is, we assume, much less, at EfB. Such a differential pattern might be consistent with the As being both relatively deprived of health to begin with and not very responsive to health care (the orphan disease case).
Alternatively, the increased funding could be shared between the two groups. The health frontier fBfA shows all the possible combinations of health given a specific increase in funding and the two production functions. A formal derivation of the frontier from the production functions and the budget constraint is in Culyer and Wagstaff (1993).
The health frontier necessarily has the convex shape of fBfA given the assumed shape of the production functions (i.e., they display diminishing marginal returns as expenditure rises). An important characteristic of this curve is that from any point on it, the average health of the As can be increased only at the expense of less health for the Bs (and vice versa). This feature is termed Pareto efficiency: a situation is Pareto efficient if no redistribution can take place without harm to at least one agent. It embraces costeffectiveness as embodied in the production functions, so there is either no waste in the health-care system or no change in its cost-effectiveness, waste included. Any point under the health frontier is by definition inefficient: increases in health are possible for at least one group without reducing the health of the other. (In all cases considered here, we abstract from uncertainty. It may be a more comfortable assumption for some readers to assume that what is measured along each axis is “expected health”).
If the budget for health care were to rise, the frontier would shift outward. Conversely, should the budget be reduced, it will shrink toward the origin 0.
Although every point on the frontier is efficient, every point is not equitable. To select the equitable point, additional criteria are needed. We can now explore some such criteria.
Different Views Of Equity
Compare three frequently met views of equity in health: equal health, equal health gain, and equal value of additional (marginal) health. These are shown in Fig. 3. The 45 line passing though the origin 0 indicates equal average health for each group. Any point on this line would be judged equitable on the criterion of equal health for each individual. Where this line intersects the frontier (at the point marked a), we have an allocation that is both efficient and equitable. This allocation requires the lion’s share of the new money to go to the Bs – the relatively deprived group. The 45 line passing through E indicates equal health gain on average. This intersects the frontier at b, an allocation that is more to the advantage of the As. It is efficient, lying as it does on the frontier, and it is also equitable (according to the criterion of equal health gain). The allocation at point c meets the criterion of equal marginal value. In cost-effectiveness analysis, where health is often measured in QALYs, this is popularly termed the QALY = QALY = QALY rule, meaning that a QALY is judged to be of equal social value to whomever it accrues. The point on the frontier at which this condition is met is where its slope is equal to 1, i.e., where a small gain to one (in either direction) is equal to the loss of the other. Thus point c indicates an allocation that is again both efficient and equitable (but this time equitable by the principle of equal marginal value). This equity rule is the most favorable for the As and results from the assumed low productivity of resources when applied to improving the health of the B.
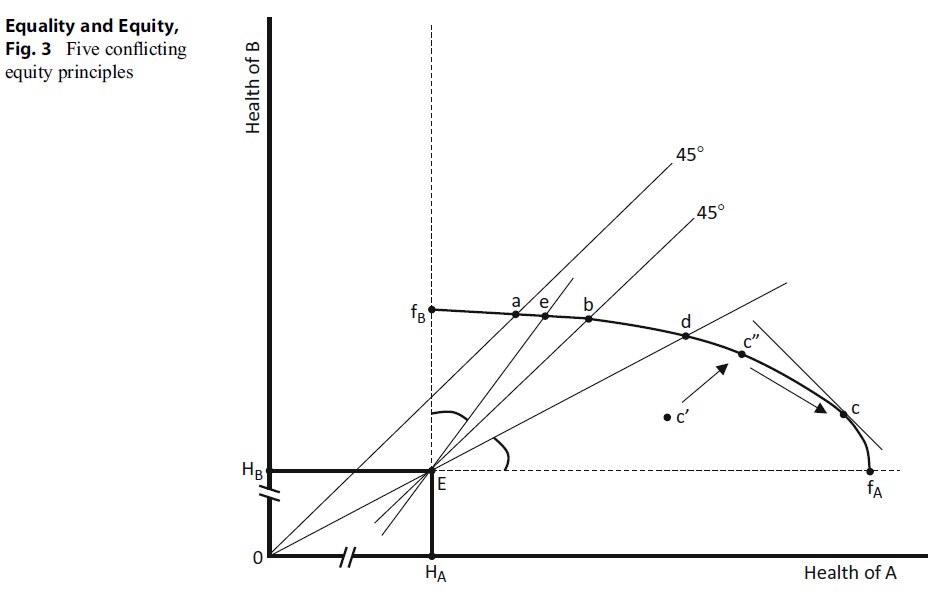 Figure 3. Five conflicting equity principles
Figure 3. Five conflicting equity principles
Each of these allocations is efficient. Each is equitable according to one criterion. What characterizes the differences in the distribution of health (and of the underlying health-care resources) is the idea of equity being used. There is a notion of equality embodied in each but it varies, underlining the importance of being clear about what one means when talking of equality. Also to be noted is that the points on the frontier are all equally efficient, which underlines the importance of not assuming that equity can be attained only at the expense of efficiency. Each of these allocations is efficient. If there is a conflict, it is between different concepts of equity rather than between efficiency and equity.
Comparisons between inefficient and equitable allocation can also be made. In Fig. 3, any point under the frontier is inefficient, since there is always some change that can increase one group’s health without reducing that of the other. If such a point also lies on either of the 45 lines, then it would be equitable (according to the ethics of whichever line it lies on) but also inefficient. But there is still no conflict between efficiency and equity, since efficiency could be improved by moving along the 45 line toward the health frontier, thereby gaining efficiency (i.e., more health for both the As and the Bs for a given expenditure) without any loss of equity. Considering the QALY = QALY = QALY rule, a point like c is a point again at which efficiency can be improved without harm to equity. Removing the inefficiencies would enable a (conceptual) move that could enhance the health of both groups (moving, say, to “c”) and then moving along the frontier to the preferred distribution at c as indicated by the arrows.
Three further criteria remain to be explored: maintaining existing distributions, allocation according to need, and equal per capita resources. The implications of a conservative equity rule are illustrated in Fig. 3 by the line from the origin (0) through E. Where this line intersects the frontier, as at point d, the distribution of average health is the same as at E. Again the system is efficient. Again, inefficient allocations under the frontier but on the line 0d would be deemed equitable (and inefficient), and greater efficiency does not require any necessary sacrifice of equity. “Need” is an ambiguous concept but is most commonly taken as being proportionate to health itself. In this view, the lower one’s health, the greater one’s need. In Fig. 3, the line through E to e is the inverse of the conservative line Ed: the angle made by it and the vertical line are the same as the angle between Ed and the horizontal line.
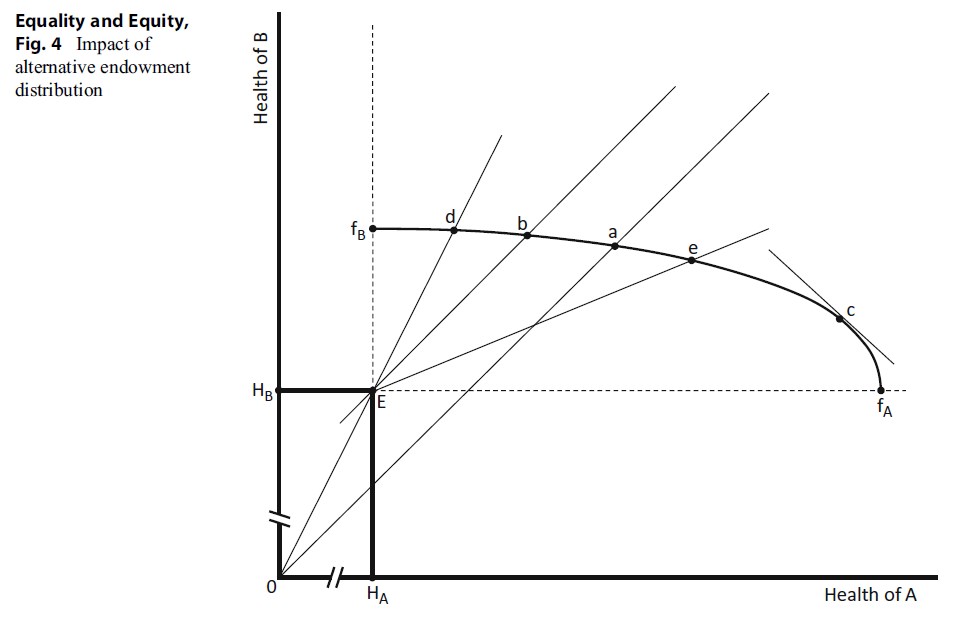 Figure 4. Impact of alternative endowment distribution
Figure 4. Impact of alternative endowment distribution
As one would expect, it is relatively favorable to the relatively deprived group and, again, is efficient. The application of the rule of allocating in proportion to need does not, however, generate equality of health: e is not a. Points inside the frontier but on Ee would also be counted as equitable, though unequal in health, but they would also be inefficient. Greater efficiency again does not imply less equity as judged by the needs principle.
Corresponding to each of the allocation solutions discussed above is a distribution of healthcare resources bought out of the given budget. Only in exceptional circumstances would the rule of equal health imply equal resources to each group (in fact it requires there to be identical production functions for all). Similarly, a different allocation of resources corresponds to each of the various distributions of health. One can also ask the question: “what distribution of health results from an equal allocation of resources to each?” The answer depends upon the production functions and the endowment (initial burden of disease) but is likely to produce an unequal health distribution.
Each of the various distributions of health depends upon the initial distribution of the burden of disease; the production functions for types of patient, classified not only by diagnosis but also by any other factor affecting the impact of health care on their health; the available budget; the extent to which health maximization and health gain are objectives of the system; and the equity criteria employed.
In foregoing, it has been assumed that the least healthy also have the poorest prospects of health improvement. If we assume a different endowment distribution of health or disease burden, the resultant distributions from applying the various criteria can change dramatically. Assuming instead that people with the less productive health production function have the lower initial burden of disease will change the ordering of points on the frontier. Such a case is shown in Fig. 4. Here point E now represents a different initial distribution of burden. Point a, representing equally distributed health, is now to the left of b and d on the health frontier, and allocation at e is now well to the right.
It is a relatively straightforward matter to show that, even if the initial distribution of health is equal, maintaining its equality will generally require discrimination in favor of those with lower capacities to benefit. This raises an interesting ambiguity in the idea of horizontal equity. Given an equal initial distribution of health and therefore need, the horizontal principle “equal expenditure for equal need” will imply increasing inequality unless the production functions are identical. On the other hand, “equal per capita resources” requires ignoring need and capacities to benefit. In each case, equity is associated with a particular form of equality – but it becomes important to inquire “equality of what?” In the special case where there is an equal distribution of the burden of disease and each has on average an equal capacity to benefit (i.e., identical production functions), then the Aristotelian principle of horizontal equity will apply – equal expenditures are implied in every case. Otherwise, inequalities in the endowment and in capacities to benefit will generally require vertical adjustments to achieve any of the desired end points.
Conclusion
The general points to be made are the following:
- The concept of efficiency we use is that of Pareto efficiency: an allocation of expenditures between groups such that no redistributions can be made to benefit one group without reducing the health of another.
- This concept of efficiency includes that of cost-effectiveness: each health outcome is produced using the technologies requiring the minimum necessary expenditure.
- Efficiency and equity are not in inherent conflict.
- An inefficient allocation can be equitable.
- An efficient allocation can be inequitable.
- An inefficient allocation can become more efficient without increasing inequity.
- What is equitable depends upon the criterion selected but does not negate any of the foregoing implications.
- What is equitable often requires inequality in health care.
- Inequality in resource distribution per capita can be equitable.
- Equality in health usually requires inequality in resource allocation.
- Equality in resource allocation usually leads to inequality in health.
- Allocation according to need typically leads to inequality in health.
- Greater equality in health requires investments in interventions that favor those with the greater burden of disease even if they have a lower capacity to benefit.
- In most cases one is dealing with vertical equity, with horizontal equity applying only to members within the groups being compared, each group being assumed to be in this sense ethically homogeneous, no one having any greater ethical claim on resources than any other.
Of the various distributive principles, each may make a choice. My own preference is for equality of health (or at least the removal of avoidable inequalities in it), mainly on the grounds that, since health is necessary for flourishing, an ultimate human good, and there seems to be no ethically acceptable reason to prefer that some should flourish more than others, all avoidable health inequalities should be removed. The contribution of health care to their removal will accordingly vary according to individuals’ initial states of health (their endowment of health) and their production functions (or capacities to benefit). It follows that the resources going to each will be unequal – but determined by the best estimate possible of the contribution they make to greater health equality. Needless now to say, those resources should also be deployed in a cost-effective way. This will imply that the assumption that a QALY = QALY = QALY be not used. Instead greater weight will be given to the health gains of the less healthy groups in society.
But the man point of all this is that different concepts of what it means to be equitable can have substantially different outcomes in terms of the distribution of health and the consequential distribution of health-care resources. This does not represent a conflict between efficiency and equity, as has sometimes wrongly been claimed, but a conflict between equity and equity. Different notions of equity can have dramatically different implications for how resources and corresponding benefits are allocated to those with various needs and abilities to benefit, with some (such as QALY = QALY = QALY) serving those who are already better off while foregoing important gains for those more disadvantaged. You need to decide where you stand on these matters, or, if you seek to advise, you need to discover where your client stands.
Bibliography :
- Culyer, A. J., & Wagstaff, A. (1993). Equity and equality in health and health care. Journal of Health Economics, 12, 431–457.
- Department of Health. (1996). Priorities and planning guidance for the NHS 1997/98. London: Department of Health.
- WHO (1948) Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference. New York: World Health Organisation. 19–22 June 1946.
- Aristotle (1972) Nicomachean Ethics. Book V. (trans: Ross, D.). Oxford: Oxford University Press. Chalkidou, K., Tunis, S., Lopert, R., Rochaix, L., Sawicki,
- T., Nasser, N., & Xerri, B. (2009). Comparative effectiveness research and evidence-based health policy: Experience from four countries. Milbank Quarterly, 87, 339–367.
- Culyer, A. J. (1998). Need – Is a consensus possible? Journal of Medical Ethics, 1998(24), 77–80.
- Culyer, A. J. (2006). The bogus conflict between efficiency and equity. Health Economics, 15, 1155–1158.
- Culyer, A. J. (2007). Need – An instrumental view. In A. Richard, D. Angus, D. Heather, & M. M. John (Eds.), Principles of health care ethics (2nd ed., pp. 231–238). Chichester: Wiley.
- Culyer, A. J., & Lomas, J. (2006). Deliberative processes and evidence-informed decision-making in health care – Do they work and how might we know? Evidence and Policy, 2, 357–371. Lomas, J., Culyer, A. J., McCutcheon, C., McAuley, L., & Law, S. (2005). Conceptualizing and combining evidence for health system guidance. Ottawa: Canadian Health Services Research Foundation.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.





