This sample Family Medicine Research Paper is published for educational and informational purposes only. Free research papers are not written by our writers, they are contributed by users, so we are not responsible for the content of this free sample paper. If you want to buy a high quality paper on argumentative research paper topics at affordable price please use custom research paper writing services.
Abstract
Family medicine, even though probably the oldest form of medicine, is a recent but rapidly expanding branch on the complex tree of medical specialties. Most countries in the world have a system of family medicine, but varieties are large. This entry shows that its position within the ordinary lives of people and some of its central tenets, especially the importance of continuity, make the ethical issues raised by and in family medicine particular.
Ethical dimensions of family medicine relate to the focus on families, both in terms of biology and in terms of a social system. They include questions about genetics and susceptibility and about trust and shared decision-making within families and also questions about the nature of the knowledge a family physician uses.
Family medicine is a comprehensive discipline, based on more or less intimate knowledge of the medical life histories of persons – the use of such knowledge may have great advantages but has its own pitfalls that are discussed.
Family medicine changes and so will the ethical issues it faces. Some of the most obvious changes are the breaking up of traditional family structures; the changing power position of patients, thanks to the Internet; and the introduction of more medical technology in the homes of people.
Apart from restating the relevance of ethics for family medicine, the conclusion also highlights the way developments in family medicine may inspire bioethical investigation.
Introduction
Bioethics has focused, by and large, on “big medicine”: the ethical problems and questions arising within hospital medicine. On problems associated with technological and scientific advances on the one hand, and with the most serious phases of disease, on the other, much of the ethical literature is about what happens in intensive care units, on neonatal wards, in psychiatric hospitals, and in genetics laboratories. Not exclusively, but predominantly at least, bioethics has focused on the unusual.
But disease always occurs within the mundane: within homes, families, and neighborhoods. It originates in, and has repercussions on, the ordinary lives of people, which is the domain of ordinary medicine: family medicine, general practice, or primary care. Three terms do not reflect different philosophies of the practice but highlight its different elements. “Family medicine” will be mainly used to indicate all of these descriptions.
This entry is about the ethical issues arising in the practice of family medicine. It will show how the specific roles of family doctors account for specific ethical issues, related to, but in no way restricted to, the issues arising in hospitals.
History And Development
Throughout history, most doctors have been family doctors in the sense of a generalist doctor who had no specific disease or specific organ system to take care of. But of course, this was a far cry from the health-care systems in parts of the world, where every or almost every citizen has access to a family doctor as the entry point to professional health care. Even so, family medicine or general practice has long been synonymous with “medicine.”
Most historians of family medicine trace its beginnings as a medical specialty and an academic discipline at around 1950 or somewhat earlier. It was the era of rampant specialization in medicine, where medicine divided into an ever-growing number of specialties and sub-subspecialties. Some of its historians describe the origins of family medicine in revolutionary and prophetic terms: “The initial promise of family medicine was that we would rescue a fragmented health care system, put it together again, and return it to the people” (Taylor 2006, p. 184).
Another, related strand of thought was that a specialty of family medicine was needed to reaffirm a holistic or, as it was later called, a biopsychosocial approach in medicine that would put the health problems of patients back in their everyday context.
In the USA, family practice was recognized as a specialty in 1969; in the Netherlands, one of the pioneer countries in family medicine, the first professor of general practice was appointed in 1966 at Utrecht University. From the 1970s onward, historians describe the history of family medicine as one of the integration in the “system they were designed to fix.” In most medical schools in the West, family medicine has a firm footing in pre and postgraduate training. It has become a recognized specialty with a professional training program in most Western countries (Sturman and Saiepour 2014).
In many other countries, family medicine is on its way to becoming a separate specialty. The world organization of family medicine World Organization of National Colleges, Academies and Academic Associations of General Practitioners/Family Physicians (WONCA), established in 1972, now claims to have 118 member organizations in 131 countries and territories with membership of about 500,000 family doctors and more than 90 % of the world’s population (http://www.globalfamilydoctor.com). Even so, there clearly are large differences in the stage of development of the discipline in various countries. In most sub-Saharan African countries, family medicine is at its very beginning, (De Maeseneer and Flinkenflögel 2010) whereas in countries like Indonesia, China, and large parts of Latin America, it is firmly developing as an academic discipline (Dai et al. 2013).
Family doctors, therefore, operate in greatly varying health-care systems, leading to quite different ethical issues. For example, in a system that lacks universal coverage of any sort, family physicians will be confronted with patients who cannot pay for their services, leading to specific ethical questions about advocacy.
Family doctors also operate in widely varying cultural and religious environments, where a question about, for instance, autonomy and competence may be raised in forms that differ dramatically from the way they have been raised in Europe or the USA. Some of the ethical issues related to medical high tech may be irrelevant in countries lacking basic health care, and other ethical questions may be unthinkable in some cultures (e.g., euthanasia).
The Concept Of Family Medicine
What is family medicine? Let us take its characterization by WONCA as a starting point. They consider family medicine/general practice as a medical specialty (not generalists versus specialists but different sorts of specialists) with the following characteristics.
The figure below shows the six pivotal characteristics of family medicine. In what follows, four of them will be discussed, because they seem to be ethically most distinctive for family medicine: its community orientation (3 and 11 in the box above), the comprehensive approach (1, 8, 9), its focus on the person (3–6), and the holistic elements (12) (Fig. 1).
The underlying concept of these core elements of family practice is continuity, both in time and in context. Family medicine is concerned with the medical life course of individuals, and it is concerned with the context in which these individuals get ill. Unlike hospital medicine, it typically does not sever the link of the patient with her community or with her life as she lives it.
This focus on continuity has important consequences for the kind of knowledge family physicians use in their work. Apart from scientific knowledge on the prevention and treatment of disease, they use historical knowledge about individuals and social knowledge about context.
Family medicine is concerned with families and relationships on the one hand and with narratives and episodes on the other. These concepts inform subsequent sections. The entry concludes with a section about the relevance of ethics for family medicine and the other way around.
Ethical Dimension
Medicine In And Of Families
Long before the genetic background of these diseases was known, family physicians knew about asthmatic families and about families with schizophrenia or alcoholism. These diseases do not fit the classic monozygotic paradigm, known in diseases such as Huntington’s, in which the presence of a gene determines that the carrier will get the disease. Genetic factors in diseases like asthma increase susceptibility, but the disease needs more than a genetic disturbance to develop, for instance, a particular lifestyle, and lifestyles typically are family matters, or a life in a nonpolluted environment.
The ethical issues related to monozygotic inheritance are related to procreational decisions but also, when it regards an incurable disease, to the right not to know about the trouble ahead if there is nothing to do about it. And, of course, ethicists rightfully addressed the possible social consequences, such as difficulties obtaining life insurance.
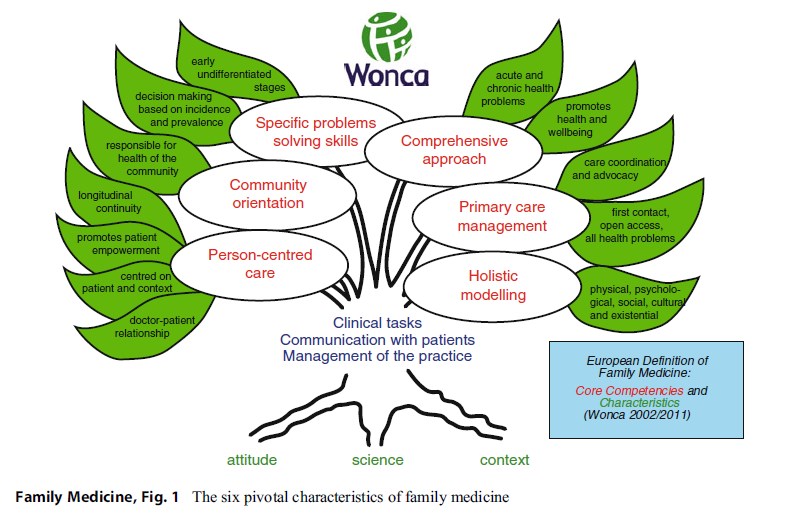 Figure 1. The six pivotal characteristics of family medicine
Figure 1. The six pivotal characteristics of family medicine
The ethical issues raised by susceptibility inheritance, which is closer to common knowledge about diseases running in families than monozygotic inheritance, are of a different nature. Because there is no one-to-one connection between genetic defect and disease, prenatal diagnosis raises new ethical problems that family physicians may be confronted with. Would it be ethically acceptable to test the fetus for the presence of BRCA in a mother who had this gene which predicts not a 100 % but something around 50 % chance for developing breast cancer later in life? Would an abortion be acceptable if the fetus shows the presence of this gene? Some ethicists say it is, others disagree. In any case, the ethical question becomes one of degrees: which degree of susceptibility would be enough to justify prenatal diagnosis and possibly abortion?
There is another effect of the shift toward susceptibility inheritance in families: because the genetic defect is but one of many factors, the focus in prevention will be on other factors, such as lifestyle. The genetics of susceptibility makes it possible to pinpoint, within a family, those who will get the “disease that runs in the family” and will need to adapt their lifestyle and those who won’t or have a smaller chance.
This may raise ethical questions for the family physician. Suppose it is known that, in family X, some children have an established susceptibility to obesity (metabolic syndrome), while others do not. Should the family physician go further in attempts to change their lifestyle than for their siblings who are not susceptible or for others who have not been tested?
Another issue with modern genetics is that probably everybody will have one or more susceptibilities to disease, be it to serious and possibly lethal ailments like cancer or to a relatively minor disease such as eczema.
Speaking With Patients And Families: Trust And Shared Decision-Making
Shared decision-making (SDM) has recently become the paradigm of the doctor-patient relationship, especially where chronic disease is involved, but more generally in all non-acute forms of medicine. However, theories of SDM tend to forget that the context in which shared decisions about matters of health are taken often is the family. Patients usually discuss their medical problems and the advice doctors give with their next of kin.
Viewed in this way, a doctor in the consultation room not only talks to the patient in front of her but also to a more or less extended but physically absent family. Do family physicians need to take these “absent presents” into account when they talk to patients, and if so, what importance should they get?
Like SDM, trust is a social phenomenon, distributed over networks of people rather than between two people. The trust patients have in their family physicians depends heavily on the trust others have in her. It is asymmetrical trust: even though the physician needs to be able to trust the patient, this seems less crucial, and it certainly is to a lesser degree dispersed over networks.
Trust has a placebo effect: some say the doctor is the most important medicine. A treatment given by a trusted doctor is more likely to help than where there is no trust in their relationship. The placebo effect has a long history in medicine. Even though there is ample evidence proving the effect of placebo in all its forms (pills, surgery, persons), it has an odor of deceit that makes it suspect from an ethics of autonomy and transparency.
So if trust is, at least in part, a placebo device, an important ethical question for family doctors is when the border between the prudent use of trust and deceit may be transgressed.
Treatment, Care, And Support: The Nature Of The Knowledge Of Family Physicians
The family physician cannot restrict herself to strictly medical treatment in the way other specialists sometimes can. Problems patients face do not come in categories; they are, more often than not, complex mixtures of somatic disturbances, fears and worries, and social issues of sorts: unemployment, loneliness, or relationship problems. The task of the family doctors is not only treatment but also care and support. How to give due attention to all of these domains within the time constraints and the demands of just distribution of care? The demand for care may seem to be without limits, whereas the family doctor’s caseload obviously has limits.
Family physicians in Europe were among the first doctors to be enthusiastic about evidence based medicine (EBM): the Dutch association of general practitioners was the first to issue a large and theoretically exhaustive number of evidence-based clinical guidelines, covering the whole of family medicine. The reasons for this pioneer position need not concern us here; the important question here is what could be called the ethics of knowledge, in which EBM sometimes seems to crowd out other, less systematized forms of knowledge, for instance, knowledge about the particular life history of a patient, about the work he has been doing most of his life or about particular difficulties in his family.
Even though the theory of EBM does not claim a dominance of randomised controlled trial (RCT)-based scientific knowledge, such evidence often gets a dominant position as a result of it being used in funding decisions (Goodman 2002).
Let us imagine a patient who has gone through a period of mourning after the death of a relative presents with symptoms of a recent sinusitis and asks for a prescription of antibiotics. All evidence based guidelines would almost certainly advise against giving antibiotics, because there is no epidemiological evidence that they shorten or alleviate the symptoms. On the other hand, the family physician might, on the basis of her knowledge of what her patient has gone through and because she thinks the patient would be reassured by getting the prescription, decide to give the prescription.
Would that be ethically defensible even though it may have no proven effectiveness? This is clearly a question about which effects count (and get investigated in clinical trials) and which don’t. And that is an ethical question: is the disappearance of the infection the only valuable effect (then don’t give antibiotics), or could the alleviation of worries also be valuable (then one could consider giving them). If the answer to the latter is “yes,” there is a subsequent question: should such an effect be proven through a randomized trial? Or could it still count as an effect, even if it can never be proven according to standards of proof? But proponents of EBM might argue that this would be “epistemological injustice,” because for some treatment goals, hard evidence would be required, and for others, not.
Continuity And Generalism
So far, continuity has been discussed in terms of context, but family medicine offers continuity in the temporal sense, as well. This bears a close relationship to its generalist mode of working. Because family physicians are the entry point to health care for all sorts of trouble, they are in a position to know the medical life history of patients, who come back to the same family doctor with all consecutive episodes of disease. That is why the doctors in the example of the mourning patient with a sinusitis would know about his history in the first place.
Narratives
Family doctors often know patients for many years and through many episodes of sickness and other forms of trouble and, also, periods of happiness such as the birth of children. Even though the number of patients enlisted with the same doctor over years or even decades may be on the decline, temporal continuity is still one of the family physician’s assets. Which values are expressed in this much-cherished ideal? Why would it be better to have a physician who intimately knows your disease history than to see a different doctor for each episode? One answer would be that having one physician for all episodes would increase attention for the relationships between episodes, based on the idea of some form of coherence, or logic, in the diseases one individual contracts over a life. One could say that personal continuity would decrease the chance of harm due to the dismemberment of what in reality is a coherent story.
But there are pitfalls, as well: one of them is overreliance on the story the physician knows so well. Imagine, for instance, a patient who has been known to his family physician for many years as a regular visitor with physical complaints that could never be explained as a distinct disease, even after referrals to specialists using the most sophisticated diagnostic technology. This almost inevitably, and understandably on the part of the physician, leads to the presumption that each new or persisting problem will be due to what has eventually been categorized as pathological fears. There have been numerous (court) cases in which this has led to harm because an important diagnosis was missed.
As said before, it is becoming rare for family doctors to treat patients throughout their life course. Still, they do treat patients in all phases of life. Whereas most specialists treat either children or adults or older patients, family physicians in most countries treat patients from age 0 to >100. Family physicians thus are confronted with all the ethical issues that are related to the beginning and the end of life. It is impossible to address all of these in this entry, but one of the central problems that the very young and the very old often (but by no means always) have in common is absent or decreasing competence. In the area of incompetence, family physicians are in a particular position because when cognitive competence disappears or is not yet there, the family becomes crucially important. Since they always treat the patient within her or his context, they have expertise in what could be called relational autonomy as opposed to individualistic forms of autonomy.
Looking Ahead: Prevention
The fact that family physicians are life course physicians implies a responsibility for what lies ahead for their patients, as far as it can be known and influenced. They integrate prevention into the care they provide. What are the foundations of this responsibility and what are its limits? Lifestyle was discussed earlier, so secondary prevention will be discussed here (the screening for possible risk factors and treating them).
Does the family physician have an obligation to screen for possible risk factors? Imagine a patient in his fifties who presents with a sprained ankle. Should the family physician offer a cardiovascular risk check, consisting of BMI, cholesterol, and blood pressure measurement? A bit like the shopkeeper who offers merchandise that the client has not asked for? Or should he take the patient’s reason for encounter as his sole responsibility? When does appropriate care turn into unjustifiable interference? This probably depends heavily on a number of characteristics of the context: on the complaints of the patient (it might be inappropriate to propose a new source of worries to an already fearful patient), on the number of patients in the waiting room, etc. The rule here would be one of minimal interference with the reason for which the patient comes in the first place and of sensitivity to what the situation demands.
There is another, more fundamental issue at stake, too: should complaint-independent screening be offered in the context of individual health care at all? This question relates to the so-called prevention paradox that says that the effects of most screening program are population effects not individual effects. A program that may be useful for the population may be next to useless for the individual. For instance, neonatal screening is offered in many countries for up to 50 very rare metabolic diseases. Each individual child has a very small chance of benefiting, but the population of newborns (and probably also the health budget) will probably benefit. With no more than a bit of exaggeration, one might say that participation in a screening program is an act of altruism: you don’t do it for your own benefit but for the benefit of all. If that is the case, should individual doctors advise individual patients to undergo screening tests? And if so, should they explain the prevention paradox to their patients (which may have a negative impact on participation)? Ethical questions that escape general answers but that remain important for family medicine nonetheless.
Guide, Advocate, And Gatekeeper
Family physicians are the entry point to the health-care system for all manner of disease. Even if family doctors treat about 90 % of ailments on their own, the WONCA description cited above says that after referral to another specialist, they remain the guide and the advocate of the patient on his trajectory. In many health-care systems, the family physician acts as what has been called, with an unfortunate term, the gatekeeper to other specialists. The idea is simple: the majority of health problems do not exceed the competencies of the generalist and should not be treated by a more expensive hospital specialist. The reason is not only financial: treating a mundane disease with too sophisticated treatments may even be a hazard to the patient.
There may be a conflict of values in the concept of the gatekeeper. If a family physician dissuades a patient from wanting to be seen by another specialist for health-related reasons, there does not seem to be a problem. If, however, budget reasons come in, there may be more than a few people who worry about double agency and its consequences for trust. There is a delicate balance to be struck, here. Physicians should obviously think about the consequences of their advice for health costs and distributive justice, and they should avoid unnecessary expenses but not to the extent that they would deny necessary treatments to their patients.
The term “gatekeeper” has unfortunate associations with border controls and barriers, both quite contrary to patient advocacy, one of the basics of family practice. Using terms like “guide” might be more appropriate. The values of family medicine imply that family doctors are (cost-effective) caregivers, guides, and advocates but not gatekeepers.
Family Medicine In A Changing World
The story of family medicine itself is constantly changing in response to changing environments. Without at all pretending to completeness, three changes will be discussed that will probably alter the position of family medicine and the ethical issues family doctors will face: the first is that families tend to spread more than before, the second is that patients will increasingly determine what happens in health care, and the third is that medical technology will get more adapted to primary care and thus will enter the patient’s home.
Spreading Families
Traditionally, families were large and geographically well defined: two or three generations could live in one village or one neighborhood and, consequently, usually had the same doctor. This picture is changing. Children, at least in the West, now frequently live at considerable distance from their parents, also when the latter are in need of care. What does this mean for (the ethics of) family medicine? Can and should family medicine still follow the value of being a medicine of families when families get more dispersed?
Two possible answers may be imagined. One is that families may disperse physically but not virtually. Social media and the use of the Internet for telecare replace older forms of family life. But are these new forms as good from a perspective of care as the old ones? Or might they even be better? Studies in empirical ethics show a mixed picture: whereas people miss face-to-face contact, they appreciate the possibility of more frequent contact.
A second answer could be that the family aspect of family medicine is effectively disappearing. This could mean that it would be replaced by other people in the context people live in, for instance, forms of caring communities without family ties. The ethics of such caring communities still await investigation.
The Position Of The Patient Changes
The possibilities of the Internet will alter the position of the patient and the relationship between doctors and patients anywhere on the planet. Not only that information about disease is more easily accessible through the Internet than ever before, patients (or healthy citizens) will increasingly use Internet-based diagnostic and lifestyle tools. Examples are the thousands of health apps made available for use on smartphones and tablets.
The effects for the work of family physicians might go in two opposite directions: it might either increase the possibilities of self-management by patients and, in doing so, decentralize or even marginalize the role of the doctor in health care; but it might just as well lead to an increase in dependence on professionals because of new questions and uncertainties induced by the sheer amount of (dis)information available. Will this raise new ethical challenges? Yes it will: doctors will have to learn to deal with, and will sometimes become part of, new Internet communities that may start to replace the traditional family but could also mean the final breakdown of the traditional power position of the physician. An ethics of health communities is still to be developed.
Mundane Technology
The Internet will continue to exert important influences on daily life, family medicine included. However, non-ICT forms of technology also enter the homes of people. Increasingly, medical technology is liberated from the confines of the hospital, gets miniaturized, and is migrating into the homes of people.
This began with the fever thermometer in the nineteenth century and has continued with all kinds of self-tests in the twentieth century. Portable blood pressure meters or peak flow meters, used to monitor asthma, are obvious examples. But also more advanced forms of technology, such as artificial respiration, reach the homes of people, involving the family physician. This raises new ethical issues related to responsibility: if such technology is moved out of a context bristling with well-trained professionals into homes with, most of the time, only nonprofessional carers, how will this impact on the responsibilities of professionals and family members? Morphine pumps, for instance, allow for rapid adjustment of morphine dosages in the home, but what if a spouse keeps underdosing out of a fear to cause the death of his wife or at least to bring her in a state of unconsciousness? Can he be held responsible for the unnecessary pain she suffers because of this (Schermer and Van Kammen 2004)?
Another question related to the transfer of medical technology into the ordinary life of people relates to the preservation of the home even as it becomes something close to an intensive care unit of family relationships as what they are – this may be called aesthetical as opposed to an ethical interest related to the effects of medical technology. Aesthetics is an undervalued element of normativity, but it will probably play an increasingly important role in questions about the good in health care, now that we witness a shift from acute to more chronic disease. Chronic disease involves a lifelong relationship to medicine and medical technology and therefore raises questions about good and dignified ways of living – these are questions of aesthetics as much as of ethics in the more traditional sense. If medical ethics can learn something from the long-term relationships that are part of family medicine, it may be a turn toward aesthetics.
Conclusion
The importance of bioethics for family medicine lies in its potential to support the central values of the practice in a changing environment. The changing of the environment is a double process: in countries where family medicine has an established position, the context changes, raising some of the new questions that have briefly been discussed in the previous sections. On the other hand, in countries where family medicine starts developing as a new discipline, it needs to take into account the specificities of the society it develops in.
But what about the relevance of family medicine for bioethics? Above, a possibly unexpected effect of family medicine for bioethics was mentioned: that it leads to raising aesthetical as much as ethical questions. There is, however, another important point of inspiration for bioethics, also related to the increase in chronic diseases and to the specific position of family medicine. Unlike hospital medicine that, despite all differences in sophistication, has a roughly similar structure wherever you go, the differences in contexts that family physician works in are enormous. This alone makes one-off solutions to ethical questions increasingly improbable; it makes the use of a model of ethics as the application (even prudently) of a set of principles, a bad idea indeed.
Ethics of family medicine has to be situated in order to be of any value at all. Being situated, in turn, implies that ethics needs thorough knowledge of the situation at hand. In other words, ethics for nonstandard situations such as family doctors work in should be an empirical ethics. It needs fine knowledge, often of a qualitative nature, of the situation family medicine operates in. It works with narratives as one of its forms of evidence.
Bibliography :
- Dai, H., Fang, L., Malouin, R. A., Huang, L., Yokosawa, K. E., & Liu, G. (2013). Family medicine training in China. Family Medicine, 45(5), 341–344.
- De Maeseneer, J., & Flinkenflögel, M. (2010). Primary health care in Africa: Do family physicians fit in? British Journal of General Practice, 60(573), 286–292.
- Goodman, K. W. (2002). Ethics and evidence-based medicine: Fallibility and responsibility in clinical science. Cambridge: Cambridge University Press.
- http://www.globalfamilydoctor.com. Accessed 20 Apr 2015.
- http://www.woncaeurope.org/gp-definitions. Accessed 19 Apr 2015.
- Schermer, M., & Van Kammen, J. (2004). Advanced home care technology: Moral issues surrounding a new health care practice. The Hague: Center for Ethics and Health. Retrieved from www.ceg.nl. Accessed 5 June 2015.
- Sturman, N., & Saiepour, N. (2014). Ethics and professionalism in general practice placements: What should students learn? Australian Family Physician, 43(7), 468–472.
- Taylor, R. B. (2006). The promise of family medicine: History, leadership, and the age of aquarius. Journal of the American Board of Family Medicine, 19(2), 183–190.
- Hurwitz, B., & Zulueta, P. (2006). Everyday ethics in primary care. London: BMJ.
- Ogle, K., Sullivan, W., & Yeo, M. Ethics in family medicine: Faculty handbook. Mississauga: College of Family Physicians of Canada. Retrieved from http://www.cfpc.ca. Accessed 5 June 2015.
- Rogers, W., & Braunack-Mayer, A. J. (2006). Practical ethics for general practice. Oxford: Oxford University Press.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.





