This sample Neonatology Research Paper is published for educational and informational purposes only. Free research papers are not written by our writers, they are contributed by users, so we are not responsible for the content of this free sample paper. If you want to buy a high quality paper on argumentative research paper topics at affordable price please use custom research paper writing services.
Abstract
Neonatology is the branch of medicine that deals with the medical conditions of the newborn baby. The patients in neonatology are preterm babies with conditions of prematurity and term babies with conditions acquired during pregnancy or labor. The most severely ill neonates are treated in neonatal intensive care units (NICUs). Ethical issues frequently arise in the delivery room and in the NICU. These ethical issues include decisions concerning starting resuscitation and advanced life support, withholding and withdrawing treatment, neonatal euthanasia in the few jurisdictions where this is legally tolerated, disagreement within the health-care team and between the health-care team and parents, decision-making problems in relation to surrogacy, and specific issues relating to neonatal research. These ethical issues are described and analyzed in this entry.
Introduction
Neonatology is the branch of medicine that deals with the medical conditions of the newborn baby. It is in many countries a subspecialty of pediatrics and was only differentiated formally from pediatrics in the 1970s or 1980s. Prior to the specialization of neonatology, obstetricians and midwifes were also involved in treating sick newborn babies.
In resource-rich countries, neonatal services are often provided within the context of highly specialized neonatal intensive care units (NICUs) where babies are treated by a multidisciplinary team of neonatologists, neonatal nurse practitioners, nurses, physiotherapists, and other health-care professionals. In 2008, 7 % of all US newborns were admitted to a NICU (Osterman et al. 2011). Babies that are less ill but still need treatment are treated in special care baby units (SCBUs), but the focus in this entry will be on the high-intensity environment of the NICU. Some neonates need highly specialized surgery, but the specific ethical issues raised by neonatal surgery are outside the scope of this entry.
Babies that need treatment in a NICU fall into three main categories:
- Preterm babies born before 37 completed weeks of gestation
- Babies with problems acquired during pregnancy or the birth process
- Babies with congenital malformations or genetic conditions
There are many problems that face preterm infants. Multiple organs can be affected adversely by being born prematurely as well as difficulties during labor or resuscitation. Lung problems include acute failure to inflate due to lack of surfactant, as well as chronic lung disease and bronchopulmonary dysplasia, and conditions caused by the process of mechanical ventilation. The bowel can also be affected, and babies can develop necrotizing enterocolitis leading to sepsis and/or the need to remove large sections of the bowel. The brain is not exempt, and intraventricular hemorrhage, posthemorrhagic ventricular dilatation, and periventricular leukomalacia are all major problems that can affect the preterm infant. These problems can lead to long-term consequences or chronic conditions that will affect the quality of life of the child and later adult throughout life.
Term babies are also not without risk if they are subjected to stress in utero. Traumatic brain injury during labor or during delivery and the resulting hypoxic-ischemic encephalopathy can result in poor quality of life, and meconium aspiration can lead to breathing problems.
The mix between the different categories of admissions varies between NICUs depending partly on the local context and disease prevalence, e.g., the proportion of substance abusing mothers, partly on whether the hospital in which the NICU is situated performs neonatal surgery.
Many ethical issues can arise in the treatment of neonates and the following are discussed below:
- Starting resuscitation and advanced life support
- Withholding and withdrawing treatment
- Neonatal euthanasia
- Decision-making and disagreement within the health-care team and between the health-care team and parents
- Specific decision-making problems
- Specific issues relating to neonatal research
Starting Resuscitation And Advanced Life Support
Babies may need resuscitation and neonatal advanced life support (NALS) immediately after they are born. That a baby will need NALS is often known or predicted in advance, for instance, if the birth is very preterm or a congenital malformation has been detected in utero. But the need for NALS may also occur in cases where it was not predicted.
In many cases, the indication for NALS will be clear, and there will be no uncertainty concerning whether NALS should be initiated or not. But there are also cases where a decision has to be made as to whether or not to initiate NALS where there is uncertainty. This occurs mainly in two scenarios:
- If the birth is very preterm and the neonate is born at the limit of viability
- If the severity of a specific congenital malformation cannot be determined with certainty in utero and there is a possibility that it may be severe and incompatible with life
A decision concerning whether or not to initiate NALS in the delivery room or operating theater is taken under very severe time constraint. It is literally the case that every second matters and that the clock on the Resuscitaire (resuscitation table) is ticking. It is therefore important that the decision is made by highly skilled staff and that the NICU and obstetrics department have agreed policies in place that describe the criteria for making the decision.
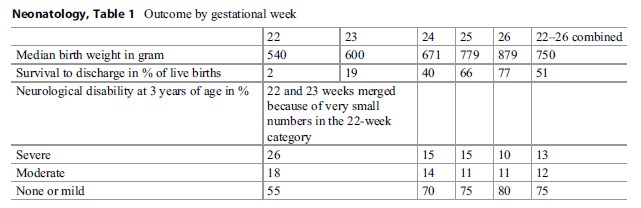 Table 1. Outcome by gestational week
Table 1. Outcome by gestational week
Decisions concerning initiation of NALS for neonates born at the limit of viability are especially complex. Over the years, the gestational age limit of viability has slowly decreased, but the prognosis for the children born at the limit has remained relatively constant. The current best outcome estimates come from the EPICure2 study which is based on all children born in the UK in 2006. The results are summarized in Table 1 (data from Costeloe et al. 2012; Moore et al. 2012).
The table shows that at the very limit of viability, 22–24 weeks, many neonates do not survive to discharge and that of those who survive many are left with neurological disabilities. It also indicates that knowing the precise gestational age is very important for predicting the outcome.
But, at the time of birth, it is not possible to establish the prognosis for the individual child with any great certainty, although there may be clinical signs that point toward a good or a bad prognosis. Spontaneous movement and respiratory effort are positive signs, whereas bradycardia and signs of infection are negative signs. It therefore makes sense to have a policy where (1) resuscitation is not attempted for neonates below the threshold of viability (in many NICUs, this is set at <23 weeks of gestation), (2) a clinical decision about initiation of NALS is made by an experienced clinician in relation to neonates just above the threshold (23 weeks), and (3) resuscitation is initiated for all healthy neonates older than a certain gestational age (usually 24 weeks or older).
If possible, parents of very preterm babies should be informed about prognosis and survival rates before delivery and also be informed about the fact that the resuscitation process and transfer to the NICU entail that they will only be able to touch their child once it is in the NICU.
Withdrawing And Withholding Treatment
Many neonates who die in the NICU die because treatment has been withdrawn or withheld; in some NICUs this figure is as high as 75 % (Wilkinson et al. 2006), whereas others report somewhat lower figures at 38 % (Hagen et al. 2004). That is, they die because of decisions made concerning their treatment and care. Decisions concerning treatment withdrawal or withholding (WoW) in the NICU are not in principle different from WoW decisions in other contexts, and the justifications for WoW are similar to the justifications for WoW in adults. The decision-making context is, however, complicated by the fact that neonates are by definition incompetent and decisions have to be made for them. It is impossible to ask them what they want, and their wishes cannot be deduced from their values or from decisions they have made during their life.
WoW can be justified if:
- The treatment is futile.
- The treatment is not likely to lead to a life with an acceptable quality of life after discharge from the hospital.
There is agreement that if a treatment is absolutely futile, i.e., there is a 0 % chance that it can produce the therapeutic goal, then it can be withheld/not offered and withdrawn if it has been initiated. There is no benefit in offering it, but potential harm, burden, and suffering.
A limiting case of futility in adults would be the brainor brainstem-dead patient, but brain and brainstem death cannot be established with certainty clinically or by EEG (electroencephalography) in the preterm infant because of a lack of development of the brainstem reflexes.
The concept of futility is, however, of less help in decision-making in two much more common situations: first, when a treatment is not absolutely futile, but only relatively futile, i.e., if there is a small chance that it will work, or if it is likely that it will partially work, and, second, when there is disagreement about whether the therapeutic goal that can (possibly) be obtained is worthwhile.
In both situations, a WoW decision will then come down to a weighing of the likely therapeutic benefit against the likely burden and suffering caused by the treatment. This way of describing the decision-making situation is, however, potentially misleading since it can give the impression of a cost/benefit equation with precision and certainty on both sides of the equation. In reality there will often be great uncertainty on both sides of the equation. It may, for instance, be clear from the clinical picture that the chance of a positive outcome is small, but not at all clear whether it is 5 %, 10 %, or 15 %. And, as in many other clinical contexts, knowing from the literature or audits that 10 % of children with the clinical presentation survive without disability cannot be transposed to the judgment that this particular child has a 10 % chance.
Nevertheless, decisions about WoW have to be made, preferably in a way so that both the neonatal team and the parents accept the decision.
A practical approach is required when it comes to WoW decisions. Accurate diagnosis of all relevant conditions and detailed assessment of the prognosis are essential. There has to be professional assessment, joint medical and nursing. The medical staff can offer their expertise as can the nursing staff who spend more time caring for the neonate (in the case of very sick neonates, there is often one to one nursing care). There has to be a joint presentation to the parents. The parents need to hear from both the medical and nursing staff. They have differing needs from both and this is essential. A decision about discontinuation of care is not one to be taken lightly, and both medical and nursing staff should be involved in this discussion with the parents. The actual process of withdrawal of care, when it has been duly considered and agreed by the parents, is also very important and has to be done with sensitivity and dignity. Electronic monitoring, investigations, medications, and therapeutic procedures should be stopped, but basic nursing care, comfort, and pain relief will continue. The parents and the child should be given a quiet place with privacy, and the support of the family through the withdrawal process and after the death of the child is essential.
Neonatal Euthanasia
In countries where voluntary euthanasia of adults is legal, it is possible to discuss whether neonatal euthanasia should also be allowed. Are there situations where doctors should be allowed to directly kill a severely disabled and suffering neonate? It is clear that a neonate can never express a wish for euthanasia, so the ethical question becomes whether the non-voluntary euthanasia of neonates should be legally allowed.
There are two main lines of argument that can be pursued to justify neonatal euthanasia. The first line of argument builds on the idea developed by a number of prominent consequentialist and pragmatic bioethicists that what gives an entity a right not to be killed is not species membership (e.g., that it is a human being) or inherent dignity, but that it is a person. On this line of argument, only persons have a right not to be killed. The criteria for personhood vary between personhood theorists, but they commonly are developed from the idea that in order to have a right to life, an entity has to know cognitively that it has a life of which it can be deprived. This means that neonates and infants are not persons, since they do not fulfill the criteria for personhood, and it is therefore not intrinsically wrong to kill them. This line of argument justifies not only neonatal euthanasia of severely disabled and suffering children but infanticide in general.
The second line of argument focuses on suffering and especially on the cases where there is agreement that the child’s life has a quality that is so bad that both health-care team and parents agree that it is justified to withhold or withdraw treatments with the intention of ending the child’s life/suffering. In those cases, a question can be raised: “If it is justified to let the child die slowly with the suffering this entails, why is it not justified to make it die quickly and without suffering through euthanasia?”
The main arguments against legalizing neonatal euthanasia, apart from more general arguments against all forms of euthanasia, point out that it is likely to be used in ways that are discriminatory against children with particular disabilities. Medical history shows that there has been reluctance to perform standard, simple, life-saving surgery on infants with Down’s syndrome, although such children are neither severely disabled nor suffering.
In the Netherlands, neonatal euthanasia of severely disabled neonates is legally tolerated, although not formally legalized.
Disagreement Within The Neonatal Team Or Between Staff And Parents
Decision-making concerning severely ill neonates is not always easy, and situations may arise in which there is disagreement within the neonatal team, or between staff and parents. Given that decisions have to be made, such disagreements must be resolved. In this context, it is important for staff to remember that for many parents, this may be the first time in their life when they are involved in life-and-death decision-making and that what is “routine” for staff is highly unusual and emotional for parents. In the case of first-time parents, they may, in addition, not yet have become fully accustomed to being parents and filling the role of proxy decision-maker.
The UN Convention on the Rights of the Child which has been ratified by all UN member states, except the USA, states in article 3.1 that:
In all actions concerning children, whether undertaken by public or private social welfare institutions, courts of law, administrative authorities or legislative bodies, the best interests of the child shall be a primary consideration.
This principle also applies in the NICU, but deciding what is “the best interests of the child” is not always easy.
As discussed above, decision-making does not only rely on “objective medical facts” but also on considerations of how this particular neonate compares to other neonates with the same gestational age or condition and of how this particular neonate responds to treatment. There is room for legitimate disagreement concerning these issues. There is also room for legitimate disagreement about whether or not a particular therapeutic outcome is worthwhile, and parents may be both more and less willing than health-care professionals to accept an outcome involving severe disability as acceptable. If the child survives with a severe disability, a significant burden will fall to the parents as the main caregivers. Some parents feel that they can shoulder this burden and some do not.
It is common for NICUs to offer at least one of the parents of severely ill children the opportunity to stay with the child and sleep in the hospital. This is important for the bonding between children and parents, and it means that the parents will often have followed the ups and downs of the child’s condition very closely. They will therefore often have firm views concerning what is in the best interest of their child.
In some circumstances where the disagreement is primarily about the prognosis, the best option is to let the disagreement remain unsolved and wait to see if the clinical picture becomes clearer. However, when this does not work and the disagreement persists and where the neonatal team is of the strong view that the best interest of the child is served by a particular decision, then they have a duty to implement that decision, even against the objection of the parents. This may in some jurisdictions have to involve a court decision.
The situation is more complicated if the disagreement is not about prognosis, but about values, i.e., about whether a certain outcome is valuable and worthwhile. Here it is less obvious that health-care professionals are in a better position to judge than the parents.
Specific Decision-Making Problems
In certain circumstances, decisions about neonates have to be made immediately after birth in a situation where the mother lacks decision-making capacity, for instance, if the child has been delivered by cesarean section under general anesthesia and where there is no other legitimate proxy decision-maker present. In such cases, health-care professionals will have to act based on what they judge as the best interests of the child and get the decisions ratified by the mother/parents later. Some decisions produce irreversible states, e.g., if resuscitation is not initiated, the child dies, or if surfactant (a one-dose drug) is administered, it cannot later be unadministered. In such situations, it is important for health-care professionals to realize that what parents do later can never amount to proper informed consent, but only to acceptance.
The rise in the use of commercial and noncommercial surrogacy has also created tricky decision-making situations in neonatology. Who should make decisions for a child that has been born as the result of a surrogacy arrangement? This will in many jurisdictions have a specific legal answer, but that is an answer that varies from jurisdiction to jurisdiction, and that legal answer may not always coincide with what seems to be the ethically most appropriate allocation of decision-making responsibility. In many jurisdictions, the surrogate birth mother will be the only one who has legal decision-making power, but if she and the contracting parents agree that the child is and will continue to be theirs, then it seems as if they should be the ones making decisions for the child.
Specific Issues In Neonatal Research
The treatment of neonates can only improve if research takes place. Research in neonatology covers a wide range of interventions and approaches, and much of it is no more controversial than other types of research involving proxy consent for incompetent research participants.
There are, however, two types of neonatal research that requires specific analysis:
- Research on standard “traditional” treatments
- Research that requires consent during labor or immediately after birth
A number of treatments and procedures in neonatology are standard and commonly used, but have never been the subject of systematic scientific investigation of their effectiveness and efficiency. It is known from other areas of medicine as well as from neonatology itself that when such “traditional” treatments are rigorously investigated, some of them are shown not to work and some to be positively harmful. It is nevertheless difficult to research such treatments, since the best research design for showing effectiveness, i.e., the randomized controlled trial, requires that some neonates are randomized to not receiving the standard traditional treatment. This may look as if they are deprived of an effective treatment. But this is a false impression if there is equipoise in the relevant clinical community, e.g., if the community is no longer certain that the treatment is effective, or if the community is divided in its view on effectiveness. In that case, both researching the treatment and continuing using it without research are options that involve risk: on the one hand, the risk of depriving some research participants of an effective treatment and, on the other, the risk of continuing to use an ineffective and potentially harmful treatment. And choosing to do the research is the only way forward that will provide the evidence that is necessary for a decision to either continue using the treatment as standard or stopping because it is ineffective.
Some neonatal research has to begin immediately after the child has been born. As the history of neonatal research shows, this may be a very dramatic research, e.g., on the use of extracorporeal membrane oxygenation (ECMO) for respiratory distress, and very mundane research, e.g., on how best to maintain the body temperature of the neonate during initial treatment in the labor suite and during transfer to the NICU. But irrespective of whether the research is dramatic or mundane, it requires parents to make decisions about research participation in a highly time-pressured and stressful context. It is difficult to think of a situation more unsuitable than being in active labor for understanding complex information about the research and reflecting carefully on it. This means that it is important to think very carefully about how informed consent is being sought. Is it, for instance, possible to identify potential participants during pregnancy and inform them and get their initial consent then, so that they only have to confirm their consent during or immediately after labor? Or, is a two-step process necessary, with simple information in the first place and an initial consent that is then later ratified when full information can be given at a less stressful time? If it is not possible to identify potential participants during pregnancy with reasonable certainty, advance information and consent given antenatally is unlikely to work effectively, because the parents are likely to perceive the choice as hypothetical and not real if they do not think that the situation will really arise in their case.
Conclusion
Health-care professionals working in neonatology encounter ethically charged clinical situations every day. Many of the patients in the NICU, the neonates, are very ill, and their condition may improve or deteriorate very quickly. Decisions have to be made in the best interest of the neonate, but those decisions cannot be made unilaterally by a single doctor; they necessarily involve the whole health-care team and the parents as the proxy decision-makers for the child. Constant reflection on ethical practice is thus necessary in this setting, as well as constant attention to open and honest communication within the health-care team and with parents.
Bibliography :
- Costeloe, K. L., Hennessy, E. M., Haider, S., Stacey, F., Marlow, N., & Draper, E. S. (2012). Short term outcomes after extreme preterm birth in England: Comparison of two birth cohorts in 1995 and 2006 (the EPICure studies). BMJ British Medical Journal, 345, e7976.
- Hagen, C. M., & Ruud Hansen, T. W. (2004). Deaths in a neonatal intensive care unit: A 10-year perspective. Pediatric Critical Care Medicine, 5(5), 463–468.
- Moore, T., Hennessy, E. M., Myles, J., Johnson, S. J., Draper, E. S., Costeloe, K. L., & Marlow, N. (2012). Neurological and developmental outcome in extremely preterm children born in England in 1995 and 2006: The EPICure studies. BMJ British Medical Journal, 345, e7961.
- Osterman, M. J. K., Martin, J. A., Mathews, T. J., & Hamilton, B. E. (2011). Expanded data from the new birth certificate, 2008. National Vital Statistics Reports, 59(7), 1–28.
- Wilkinson, D. J., Fitzsimons, J. J., Dargaville, P. A., Campbell, N. T., Loughnan, P. M., McDougall, P. N., & Mills, J. F. (2006). Death in the neonatal intensive care unit: Changing patterns of end of life care over two decades. Archives of Disease in Childhood-Fetal and Neonatal Edition, 91(4), F268–F271.
- Nuffield Council on Bioethics. (2006). Critical care decisions in fetal and neonatal medicine: Ethical issues. London: Nuffield council on bioethics. Available at http://nuffieldbioethics.org/wp-content/uploads/2014/07/CCD-web-version-22-June-07-updated.pdf
- Royal College of Paediatrics and Child Health. (2014). Practical guidance for the management of palliative care on neonatal units. London: RCPCH. Available at http://www.bapm.org/publications/documents/guide lines/NICU-Palliative-Care-Feb-2014.pdf
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.





