This sample Tobacco Abuse in Correctional Settings Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of criminal justice research paper topics, and browse research paper examples.
The United States incarcerates the largest percentage of its population of any country in the world, with over eight million adults and 650,000 youth under some form of local, state, or federal supervision, including prisons, probation, or parole (Taxman et al. 2007). The number of individuals under criminal justice supervision in the community has quadrupled over the past 25 years from 1.12 million in 1980 to 4.9 million in 2010 and comprises the largest segment of the criminal justice population (Glaze and Bonczar 2011). The increase in the criminal justice population has been attributed in part to the war on drugs and a political climate that favors increasingly punitive sentencing. Although a common misconception is that incarcerated people are removed from the community indefinitely, as many as nine million individuals are released from prisons and jails and return to their communities each year (Beck 2006). Consequently, policies surrounding the availability and use of tobacco products and the availability of resources for tobacco cessation in correctional settings have a profound impact on efforts to reduce the morbidity and mortality associated with tobacco use in the United States.
This research paper discusses the prevalence of smoking and trends in tobacco use in correctional settings, common comorbidities such as substance abuse and dependence and psychiatric illness associated with tobacco use among incarcerated people, the health consequences of tobacco use among people in the criminal justice system, policies surrounding tobacco use in correctional settings, interventions for smoking cessations with criminal justice populations, and implications for the public health impact of tobacco use in the United States.
Fundamentals
Prevalence And Trends In Smoking
Despite over 40 years of public health messaging as well as populationand individual-based interventions, smoking remains the leading cause of death and disability in the United States. While smoking rates have declined to about 19 % among the general population, smoking remains disproportionately high for individuals in the criminal justice system (Cropsey et al. 2010). Figure 1 illustrates the prevalence of smoking from 1990 to 2011 for the general population and correctional populations. While individuals under criminal justice supervision represent approximately 3.6 % of the general population, they represent over 12 % of current smokers (Centers for Disease Control 2011). The high rates of continued smoking among individuals in the criminal justice system suggest that public health messages and interventions have been largely ineffective or have not penetrated to this population.
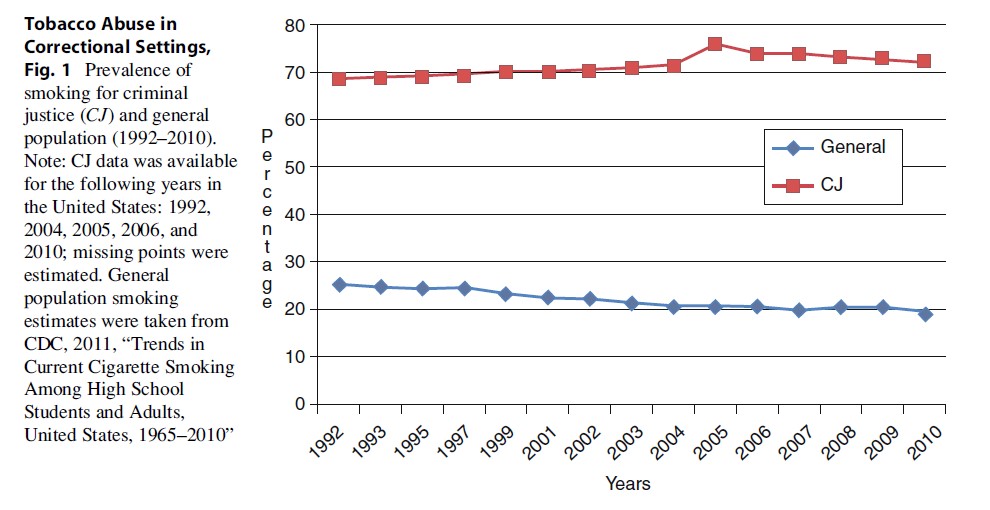
Smoking prevalence among adults in the general population is about 19.3 % (Centers for Disease Control 2011). Among incarcerated men, smoking prevalence is 70–80 % and has remained steady over the past 20 years (Cropsey et al. 2010). Similarly, a recent survey of individuals under community corrections supervision indicated that 72.3 % were current smokers (Cropsey et al. 2010). Smoking rates among female arrestees range from 42 % to 91 % – two to four times greater than among women in the general population (Nijhawan et al. 2010). Finally, approximately 70 % of adolescents in the juvenile justice system have tried smoking and half are daily smokers (Cropsey et al. 2008b). This compares to about 44.7 % of adolescents not in the juvenile justice system who have tried smoking and 6.4 % who reported smoking on 20 or more days of the month (Centers for Disease Control 2012).
Smoking is entrenched in the culture of prisons and jails and has a place in prison life that differs from that in the “free world.” With smoking rates three to four times higher among criminal justice populations than among individuals in the general population, smoking is normative in correctional settings and lacks the stigma attached to smoking in the “free world” (Cropsey et al. 2008a). In correctional settings, smoking connotes peer acceptance and creates a shared social and emotional connection. In addition, tobacco products are an important part of the informal economy in correctional settings and are traded and bartered for other commodities or services.
Smoking Comorbidities
Mental Illness
In the general population, individuals with histories of psychiatric disorders have higher rates of lifetime and current smoking and are less likely to quit smoking. Rates of smoking are substantially higher among individuals diagnosed with depression, schizophrenia, and anxiety disorders. Active psychiatric disorders are risk factors for onset of daily smoking and progression to nicotine dependence. Nicotine-dependent individuals with comorbid psychiatric disorders make up less than 10 % of the US population but consume over a third of cigarettes smoked in the United States (Grant et al. 2004). In addition, the burden of smoking-related disease is significant in smokers with chronic mental illness. For example, among individuals with chronic mental illness, the prevalence of chronic obstructive pulmonary disease (COPD) is over four times greater than the estimated COPD prevalence for individuals of a similar age in the general population.
Psychiatric disorders are prevalent in correctional populations, which may contribute to the high prevalence of smoking in criminal justice population. The prevalence of psychiatric disorders in correctional populations ranges from 7.6 % to 36.5 %, with 14.7 % of incarcerated individuals diagnosed with a psychiatric disorder in the past year (Glaze and James 2006). Additionally, one in four incarcerated people reports a learning impairment, which may compound the morbidity from other psychiatric diagnoses. The high prevalence of psychiatric disorders in correctional populations has been linked to the deinstitutionalization of mentally ill persons in the United States and the lack of access to mental health services in the community. Suicide was once the leading cause of death among jail inmates. Over the past 20 years, suicide has decreased drastically in the incarcerated population; however, the suicide rate in jails remains at 47 per 100,000 (Mumola 2005) compared to 12 per 100,000 in the general population (Heron 2012). Outside the correctional setting, incarcerated individuals are exposed to factors that contribute to the development of, and relapse to, mental illness, including sexual assault, childhood abuse and neglect, and abusive relationships. In addition, incarceration may exacerbate mental health problems, with violence, isolation from family and friends, and overcrowding being likely contributors to the high rates of mental illness in correctional populations. Thus, the rates of smoking and the high prevalence of psychiatric disorders in correctional populations suggest that a large proportion of incarcerated individuals may have difficulty quitting smoking without intensive interventions and may suffer long-term and serious health consequences from smoking.
Substance Abuse
In the general population as well as the incarcerated population, smoking is closely linked to the use of alcohol and other substances. In the general population, individuals with histories of dependence on alcohol and other substances smoke more heavily, are more nicotine dependent, and are less likely to quit successfully without intensive interventions. For example, 70–90 % of individuals who abuse alcohol and other drugs are cigarette smokers (Bowman and Walsh 2003), and tobacco use is associated with initiation and increasing levels of consumption of alcohol and other drugs.
Population studies show a clear, bidirectional relationship between nicotine dependence and dependence on alcohol and other drugs. Nicotine dependence is most prevalent among individuals with a current substance use disorder. Alcohol-dependent smokers are more physically dependent on nicotine, and heavy drinkers smoke more cigarettes, smoke sooner after awakening (an indicator of nicotine dependence), and inhale more smoke from each cigarette. In addition, individuals who are dependent on other substances smoke higher nicotine content cigarettes. Smokers with comorbid abuse of other substances are less likely to maintain long-term tobacco cessation and require more intensive behavioral and pharmacological interventions. Finally, alcohol and tobacco have a synergistic impact on health; health risks for individuals who abuse alcohol and smoke are greater than health risks for individuals who abuse either substance alone. In fact, among treated alcoholics, more deaths are attributable to smoking than to alcohol.
The “war on drugs” has been credited with the sharp increase in drug-related offenses among individuals in the correctional population. Most incarcerated people enter prison or jail with a history of abuse and dependence on alcohol and other substances. For example, about 56 % of inmates reported using drugs in the month prior to their offense, while about a third reported using drugs during the time of their crime (Karberg and Mumola 2006). Overall, about half of individuals in prison meet DSM-IV criteria for a substance use disorder. Given the overwhelming use of criminal sanctions for drug use behavior in the United States, as well as the association between drug use and smoking, it is not surprising that so many prisoners have high rates of smoking.
Medical Problems
The increase in incarceration over the past 30 years has resulted in increased correctional costs, from $20 billion in 1982 to over $74 billion in 2007, more than a threefold increase in annual expenditures (Bureau of Justice Statistics 2012). Healthcare costs have contributed substantially to this increase and are expected to double over the next 10 years, adding further financial burden to correctional systems already facing economic hardships (Lamb-Mechanik and Nelson 2000). Smoking-related diseases contribute substantially to this increase in correctional medical costs. Even though 88 % of individuals in the correctional system are younger than 50, 43 % of incarcerated males and 57 % of incarcerated females report at least one medical problem (Maruschak 2008). The most common medical problems are directly related to or exacerbated by smoking, including diabetes and heart, circulatory, respiratory, kidney, and liver problems.
Correctional populations are especially vulnerable to the negative health consequences of smoking. Many smokers increase smoking during incarceration, and many incarcerated people report a greater need to smoke due to the stress, boredom, and deprivation of prison life. Because of restricted availability and the expense of purchasing tobacco products from prison or jail commissaries or on the black market, many smokers switch to unfiltered hand-rolled cigarettes, which are higher in tar and nicotine. Recent studies have demonstrated that smoking roll-your-own cigarettes was associated with greater smoke exposure compared to factory-manufactured cigarettes. Thus, smoking in prison may present a greater health risk than smoking outside prison.
Racial Disparities
Over the past decade, smoking prevalence rates for African-Americans have come to equal those of Caucasians (21.3 % vs. 22.1 %; Centers for Disease Control 2011). This increase in smoking for African-Americans is further complicated by the fact that they tend to have higher rates of smoking-related diseases and mortality from smoking and more difficulty with smoking cessation. The differences in cessation rates have been documented even when controlling for potential moderators in both incarcerated (Cropsey et al. 2009) and nonincarcerated populations. This increase in smoking-related consequences and difficulties with cessation may be due to African-American’s preference for smoking mentholated cigarettes which results in higher CO concentrations. African-Americans are overrepresented in the criminal justice system such that while they comprise only about 30 % of the general population, approximately 60 % of African-American men are incarcerated for at least 1 year before age 35 (Pettit and Western 2004). The overrepresentation of African-Americans in the criminal justice system in conjunction with their increased difficulty with cessation and greater health risks highlights both the importance and difficulty of cessation in this population.
Prison Policies
Tobacco policies have changed profoundly in US correctional facilities in the past several decades, with a consistent trend toward increasingly restrictive policies toward tobacco availability and use (Kauffman et al. 2008). Historically, tobacco use was an accepted part of life in US penal institutions, and state and federal correctional institutions routinely provided free tobacco. Although some correctional systems provided tobacco products to make incarceration more humane, cigarettes also played a role in maintaining order within facilities.
In the mid-1980s, about half of state correctional facilities provided free tobacco. By the early 1990s, tobacco products were sold in about 88 % of prison commissaries, 26 % of prison systems provided tobacco at no cost for indigent inmates, and 8 % of prison systems provided no cost tobacco products to all inmates (Vaughn and del Carmen 1993). Some correctional systems phased out distribution of free tobacco as incarcerated people gained the opportunity for paid employment and had money to purchase tobacco products from prison commissaries.
The initial impetus for changing tobacco policies was cost containment, including the cost of providing tobacco products, maintaining buildings and facilities, and treating smoking-related medical conditions. The trend toward restricting tobacco gained momentum because of concerns about exposure to environmental tobacco smoke (ETS). ETS is a particular health risk in correctional facilities because of the high prevalence of smoking, overcrowding and poor ventilation, inadequate facilities, and unrestricted indoor smoking or poor enforcement of indoor smoking policies. Smoke concentrations in correctional facilities are greater than in the homes of smokers. Finally, the desire to limit amenities for incarcerated people provided additional impetus for changes in tobacco policies. In 1986, only 5 % of US prisons had smoke-free living areas; by 2007, 96 % had smoke-free living areas, 27 % banned indoor smoking, and 60 % banned smoking completely (Kauffman et al. 2008).
Tobacco policies in correctional settings range from policies restricting smoking to policies prohibiting possession of tobacco products or tobacco use anywhere on facility grounds. A complicating factor in correctional tobacco policies is that the correctional facility is the incarcerated individual’s home and there is some debate whether incarcerated people have the right to smoke as long as nonsmokers, other inmates, and staff members are protected from exposure to ETS. Complete tobacco bans force incarcerated people to quit tobacco use involuntarily or continue to use tobacco products illicitly (Eldridge and Cropsey 2009).
Although there is relatively little research on the impact of tobacco bans and restrictions in correctional settings, the research that is available indicates that the majority of people continue to smoke after the imposition of tobacco restrictions. Partial tobacco bans (i.e., incarcerated individuals are allowed to possess tobacco products but smoking is restricted in indoor areas) may be more difficult to enforce than complete tobacco bans. Organizational and environmental factors in correctional settings often mitigate against consistent enforcement of tobacco bans and the imposition of disciplinary sanctions for tobacco possession or use. Although administrators and others are often concerned about the possibility of violence and disciplinary infractions during the transition to smoking restrictions, there is little evidence that this occurs.
Despite the fact that tobacco use tends to persist after the imposition of smoking bans and restrictions, there is evidence of a reduction in the amount of tobacco consumed, which has implications for health and air quality in correctional settings. There is evidence of an improvement in air quality and a reduction in ETS and suspended particulates after the imposition of tobacco restrictions.
Despite these positive changes as a consequence of tobacco bans and restrictions, one negative change is a gradual reduction in the availability of tobacco cessation programs and materials. For example, tobacco cessation programs were offered in 86 % of correctional facilities with indoor tobacco restrictions compared to 39 % of facilities with total tobacco bans. Similarly, tobacco cessation aids (e.g., nicotine replacement) were available in 65 % of facilities with tobacco restrictions but only 35 % of facilities with total bans. This raises the question about whether the goal of tobacco restrictions in correctional settings is to suppress tobacco use during incarceration or to accomplish lifelong tobacco cessation. The trend toward restricting tobacco use while decreasing availability of tobacco cessation programs and materials is likely to result in temporary suppression of tobacco use during incarceration rather than long-term tobacco cessation during incarceration and after release (Kauffman et al. 2008). Although data are sparse, almost all individuals released from smoke-free correctional facilities resume smoking within 6 months of release (>98 %), with only 37.3 % remaining abstinent from smoking at the end of the first day post-release (Lincoln et al. 2009).
Interventions
Very few smoking cessation studies have been conducted with correctional populations, and none have been conducted with individuals in community corrections. Initially, two pilot studies examined smoking interventions with prisoners, and both used small samples and focused exclusively on male inmates. More recently, a large randomized controlled trial of smoking cessation with female prisoners who were provided NRT and 10 weeks of group smoking cessation counseling showed cessation rates comparable to community smoking cessation interventions. The literature suggests that spontaneous quit attempts among female prisoners are rare. However, this study demonstrates that female prisoners are interested in smoking cessation that it is feasible to provide smoking cessation in correctional environments, and that incarcerated smokers quit smoking successfully when provided with community standard smoking cessation interventions. However, no studies have examined providing integrated smoking cessation treatment to community corrections populations, despite the high need for such interventions and the public health relevance of reaching this low-income population. Given that smoking is now concentrated in individuals with low incomes who may have substance use and mental illness problems, smoking cessation interventions must be able to reach these individuals who are at risk and who do not have access to standard smoking cessation interventions in the community. Individuals in community corrections represent such a population of high-risk smokers who are poor and do not have access to community-level smoking cessation interventions.
Recommendations For The Field
Correctional settings house individuals with high rates of smoking, smoking-related medical conditions, histories of drug and alcohol abuse and dependence, and psychiatric illnesses that present challenges to long-term smoking cessation. Incarceration (and criminal justice supervision in the community) provides an opportunity to address tobacco use in a population that may otherwise have less access to tobacco cessation programs and materials. In 2002, the National Commission on Correctional Health Care in its report on the health status of soon-to-be-released inmates recommended that incarcerated people have access to smoke-free environments and smoking cessation materials and programs. However, smoking among criminal justice populations, particularly individuals under community corrections supervision, is virtually ignored in the research literature, despite the enormous human, health, and economic costs to correctional settings and to the community after release (Cropsey et al. 2004).
The current state of tobacco policies (i.e., tobacco bans and restrictions and availability of tobacco cessation programs and materials) in correctional settings highlights the gap between temporary suppression of smoking during incarceration and long-term smoking cessation. Although data are sparse, most individuals released from correctional facilities relapse to smoking soon after release. Prisons and jails provide an opportunity for achieving lifelong smoking cessation for disadvantaged men and women, with the potential for an enduring positive impact on health and economic security. However, as correctional settings impose tobacco bans and restrictions while diverting resources away from smoking cessation programs and materials, that opportunity is being lost.
Bibliography:
- Bailey BA, Daugherty RA (2007) Intimate partner violence during pregnancy: Incidence and associated health behaviors in a rural population. Matern Child Health J 11:495–503
- Beck AJ (2006) The importance of successful reentry to jail population growth. Presented at the Urban Institute’s jail reentry roundtable, 27 June 2006. www.urban.org/projects/reentry-roundtable/upload/ beck.PPT
- Bowman J, Walsh R (2003) Smoking intervention within alcohol and other drug treatment services: a selective review with suggestions for practical management. Drug Alcohol Rev 22:73–82. doi:10.1080/0959523021000059857
- Bureau of Justice Statistics (2012) Direct expenditures by justice function, 1982–2007. Extracted on 24 July 2012. http://bjs.ojp.usdoj.gov/content/glance/tables/exptyptab.cfm
- Centers for Disease Control and Prevention (2011) Vital signs: current cigarette smoking among adults aged 18 years – United States, 2005–2010. Morb
- Mortal Wkly Rep 60(33):1207–1212. Accessed 24 Jan 24 2012
- Centers for Disease Control and Prevention (2012) Trends in the prevalence of tobacco use national YRBS: 1991–2011. Extracted on 19 July 2012. http://www.cdc. gov/healthyyouth/yrbs/pdf/us_tobacco_trend_yrbs.pdf
- Cropsey KL, Eldridge GD, Ladner TL (2004) Smoking among female prisoners: an ignored public health epidemic. Addict Behav 29:425–431
- Cropsey KL, Eldridge GD, Weaver MF, Villalobos GC, Stitzer ML, Best AM (2008a) Smoking cessation intervention for female prisoners: addressing an urgent public health need. Am J Public Health 98:1894–1901
- Cropsey KL, Jones-Whaley S, Jackson DO, Hale GJ (2010) Smoking characteristics of community corrections clients. Nicotine Tob Res 12:53–58
- Cropsey KL, Linker JA, Waite DE (2008b) An analysis of racial and sex differences for smoking among adolescents in a juvenile correctional center. Drug Alcohol Depend 92:156–163. doi:org/10.1016/j.drugalcdep. 2007.07.018
- Cropsey KL, Weaver MF, Eldridge GD, Villalobos GC, Best AM, Stitzer ML (2009) Differential success rates in racial groups: results of a clinical trial of smoking cessation among female prisoners. Nicotine Tob Res 11:690–697
- Eldridge GD, Cropsey KL (2009) Smoking bans and restrictions in U.S. prisons and jails: consequences for incarcerated women. Am J Prev Med 37(2s): S179–S180
- Glaze LE, Bonczar TP (2011) Probation and parole in the United States, 2010. U.S. Department of Justice, Bureau of Justice Statistics, NCJ 236019
- Glaze LE, James DJ (2006) Mental health problems of prison and jail inmates. Bureau of Justice Statistics, NCH 213600
- Grant BF, Hasin DS, Chou P, Stinson FS, Dawson DA (2004) Nicotine dependence and psychiatric disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry 61:1107–1115. doi:10.1001/ archpsyc.61.11.1107
- Hammett TM, Harmon MP, Rhodes W (1997/2002) The burden of infectious disease among inmates of and releases from US correctional facilities. Am J Public Health 92:1789–1794
- Harrison PM, Beck AJ (2003) Prisoners in 2002. U.S. Department of Justice, Bureau of Justice Statistics, NCJ 200248
- Heron M (2012) Deaths: leading causes for 2008. Natl Vital Stat Rep 60:9–10. http://www.cdc.gov/nchs/data/ nvsr/nvsr60/nvsr60_06.pdf. Accessed 25 Feb 2013
- Himelhoch S, Lehman A, Kreyenbuhl J, Daumit G, Brown C, Dixon L (2004) Prevalence of chronic obstructive pulmonary disease among those with serious mental illness. Am J Psychiatry 161:2317–2319
- Karberg JC, Mumola C (2006) Drug use and dependence, state and federal prisoners, 2004. Bureau of Justice Statistics, NCJ213530
- Kauffman RM, Ferketich AK, Wewers ME (2008) Tobacco policy in American prisons, 2007. Tob Control 17:357–360
- Lamb-Mechanik D, Nelson J (2000) Prison health care survey: an analysis of factors influencing per capita costs. National Institute of Corrections. http://nicic. org/pub/2000/0159.99.pdf. Accessed 9 Sep 2003
- Lincoln T, Tuthill RW, Roberts CA, Kennedy S, Hammett TM, Langmore-Avila E, Conklin TJ (2009) Resumption of smoking after release from a tobacco-free correctional facility. J Correct Health Care 15:190–196
- Maruschak LM (2008) Medical problems of prisoners. U.S. Department of Justice, Bureau of Justice Statistics, NCJ 221740
- Mumola CJ (2005) Suicide and homicide in state prisons and local jails. U.S. Department of Justice, Bureau of Justice Statistics, NCJ 210036
- Nijhawan AE, Salloway R, Nunn AS, Poshkus M, Clarke JG (2010) Preventive healthcare for underserved women: results of a prison survey. J Womens Health 19:17–22
- Pettit B, Western B (2004) Mass imprisonment and the life course: race and class inequality in U.S. Incarceration. Am Sociol Rev 69:151–169
- Taxman FS, Young DW, Wiersema B, Rhodes A, Mitchell S (2007) The national criminal justice treatment practices survey: multilevel survey methods and procedures. J Subst Abuse Treat 32:225–238. doi:10.1016/ j.jsat.2007.01.002
- Vaughn MS, del Carmen RV (1993) Smoking in prisons: a national survey of correctional administrators in the United States. Crime Delinq 39:225–230
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.





