This sample Treating Mentally Ill Offenders Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of criminal justice research paper topics, and browse research paper examples.
Prisons and jails now include a substantial number of individuals who are mentally ill or substance abusers. This research paper reviews how offenders with mental health and substance abuse disorders are handled for their behavioral health disorders. More importantly, the overrepresentation of minorities in the correctional system presents challenges to diagnoses and treatments offered, given the disparities in health care in the community. The importance of medications, and the continuation after release from prison or jail, is emphasized as a necessary tool to safely manage and assist individuals with behavioral health disorders. The failure to provide adequate diagnoses and treatment in confinement facilities, as well as in the community, has implications for efforts to reduce the demand for incarceration.
Introduction
The United States has shown a substantial increase in its correctional population, with much of it due to the “war on drugs” increasing the incarceration of the mentally ill and substance abusers. This special population often requires unavailable treatment. Moreover, minority and poverty-stricken populations make up the majority of the correctional population and face the same disparities in access to care as these individuals see in the noncorrectional population. Diagnostic concerns, lack of access to psychotherapy, and pharmacotherapy are quite prevalent. Nevertheless, treatment availability can improve the correctional environment and has positive consequences for recidivism and the larger society. Moreover, substance abuse treatment can reduce the spread of diseases such as AIDS. Approaches such as drug courts and integrated programs have helped to improve access to treatment and maintain adherence to care in the community.
Prisons and jails now include a substantial number of individuals who are mentally ill or substance abusers. Estimates of the inmate population that is severely mentally ill range from 15 % to 30 % (Fazel and Seewald 2012). Fifty percent to 65 % of state and federal prisoners and jail inmates have a diagnosis of mental illness (James and Glaze 2006). Jails and prisons are now the largest provider of mental health services in the country, serving more mentally ill than any public mental health hospital or clinic. Half of the correctional population meets standard diagnostic criteria for drug dependence or abuse (Mumola and Karberg 2006).
Unfortunately, individuals in the correctional system are often underdiagnosed and undertreated. Once incarcerated, inmates have little chance of accessing mental health services with fewer than 17 % actually receiving services. Moreover, individuals are under-referred for mental health services and correctional systems lack the professional staff to address mental disorders, such as providing evidence-based psychotherapy (Foulks 2004). The culture of corrections further complicates the problem since the need for security and control supersedes the need for treatment. Nevertheless, the need for treatment services is well documented. Consequently, many correctional settings offer treatments of various types or at least make an attempt to manage those mentally ill individuals or substance abusers who are clearly behaviorally disturbed or suffering from intoxication or withdrawal.
Barriers To Treatment And Services
The correctional system as an institution has a different perspective on the role of treatment, as shown in Table 1.
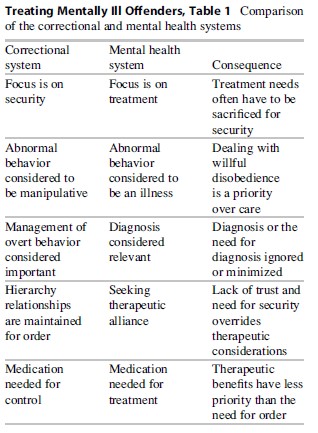
The correctional system is a punitive system with a focus on security. In such a setting, a therapeutic alliance, while possible, is sacrificed to the need for order; trust is secondary. Interventions necessarily are focused on control rather than therapeutic improvement and treatment needs are sacrificed for security.
There are also key staffing issues. Jails and prisons face multiple challenges in providing inmates with adequate care because of several reasons. One such challenge is the lack of knowledge of treatment histories or medications. Second, jail and prison officials do not have access to medical records. Finally, there is an inability to communicate with providers because of confidentiality restrictions.
Demographics are also important. The incarcerated are disproportionately poor and minority. African-Americans are disproportionately represented in the criminal justice system-10 % of African-American men between ages 18 and 34 were in prison in 2005 (three times the rate of Hispanic men and seven times that of White men). African-Americans and Latinos make up over half the prison population, which is a far greater representation than in the larger society. For example, African-American juveniles with conduct problems are sent to youth detention while their White counterparts receive treatment. In addition, African-Americans arrested for possession are more likely to be incarcerated than their White counterparts (Iguchi et al. 2005).
Disparities in services for the poor and minorities in the general population are well documented (Kessler et al. 2005; Primm and Lawson 2010). African-Americans with depression are only half as likely to get treatment services even when they are appropriately diagnosed. Incarceration can contribute to these disparities as inmates are less likely to get treatment, or have difficulty linking to services after release due to structural issues related to incarceration (Springer et al. 2012). Outside of the correctional system, less than a quarter of African-Americans receive evidence-based treatment for most mental disorders in any setting.
Consequences Of Lack Of Treatment
The need for treatment is also related to the fact that most incarcerated individuals are ultimately released. The failure to treat mental illness and substance abuse contributes to recidivism, trapping individuals in an endless cycle of mental illness and incarceration. This cycle appears particularly prominent among African-Americans (Primm and Lawson 2010). African-Americans are more likely to be underserved in correctional settings (Hartwell 2001) and due to their overrepresentation, their release greatly affects the African-American community that often is one with limited resources and high rates of poverty.
Moreover, prisons have become vectors for chronic diseases such as AIDS, Hepatitis C, and treatment-resistant TB (Springer et al. 2012). Recently released inmates have been found to be infected with HIV and continue to be involved in risky behavior such as high-risk sex or drug abuse. These disorders can be spread to the general population through high-risk behavior if the individuals are not treated for both the underlying mental illness or substance abuse and the chronic illness.
Mental disorders can be associated with violence when untreated. Yet when treated, individuals with mental disorders are no more violent than the general population. Substance abuse can also be associated with continued criminal behavior. Treatment of substance abuse reduces the risk of such behavior in the community and reduces crimes rates. Lack of access to treatment therefore affects both the incarcerated and general community.
The First Step: Accurate Diagnosis
Misdiagnosis and underdiagnosis is common in correctional settings. Moreover, the poor and ethnic minorities are probably more likely to be underdiagnosed or misdiagnosed, given the findings from the non-correctional community.
Outside of the correctional system, clinicians tend to grossly overdiagnose ethnic minorities with relatively uncommon disorders such as schizophrenia at the expense of much more familiar ones, such as mood and anxiety disorders (Strakowski et al. 2003). This underrecognition of some mental disorders and excessive misdiagnosis of others contributes to treatment disparities among African-Americans and Latinos. Such disparities also contribute to the failure of recognizing these disorders in the prison system. Mentally ill, underrepresented minorities are often not recognized as having a disorder and are instead arrested, which further contributes to the increase in mental illness within the prison population (Foulks 2004).
Anxiety Disorders
Anxiety disorders are less likely to be observed in the community for African-Americans diagnosed by clinicians without the use of assessment instruments, which are related to misdiagnosis and underrecognition of symptoms. However, anxiety disorders such as generalized anxiety disorder or posttraumatic stress disorder (PTSD) are among the most common mental disorders and may show a higher prevalence among those in the correctional system because of the correctional setting itself. Prisoners can and do exploit each other, and the problem of violence and victimization within the correctional system is well documented. Mentally ill prisoners are far more likely to be victimized and exploited (Crisanti and Frueh 2011).
Many individuals enter the correctional setting with preexisting lifestyle factors that are similar in the inner city. Individuals are often exposed to violence if not victimized themselves, and PTSD is widespread in inner cities where minorities and the poor are over-represented (Alim et al. 2006). PTSD is both underdiagnosed or misdiagnosed, as those with the disorder tend to be hyper-vigilant, and show autonomic hyperactivity and emotional numbness, which could be interpreted as psychotic or antisocial (Lawson 2009). African-Americans are generally at risk of being perceived as guilty or troublemakers, and those with suspicious behavior, such as the hyper-vigilance and emotional numbness associated with PTSD, are often perceived as being criminals (Hicks 2004). The result is delayed or no treatment.
Depression
Depression is among the most common disorders in the correctional system (Baillargeon et al. 2000). Although depression is often treated in the correctional system, there is a large unmet need as suicide rates are higher in the prison system than in the community (Rabe 2012). Failure to recognize depression may arise from a lack of awareness of African-American and Latino culture (Primm and Lawson 2010). Moreover, low income individuals and many ethnic minorities, especially males, do not report sadness and often will focus on the vegetative or physical signs of depression, including sleep or eating disturbance, and somatic complaints. The problem is further enhanced by the failure of many inmates to recognize depression. Gang members may show their depression by “acting out” and commit antisocial or violent acts.
Suicide is an important consequence of depression. Suicide and suicide attempts have been recognized as a worldwide problem in correctional systems. It is clearly more common than in the general community, perhaps due to the high rates of victimization as well as unrecognized psychopathology (Crisanti and Frueh 2011). Early recognition and treatment of depression is one essential approach to reducing the suicide risk.
In the past, suicide was thought to be rare among ethnic minorities. However, recent studies have shown young African-American males do not differ in rates from their White counterparts, while Native Americans have among the highest rates in young men (Joe et al. 2006).
Bipolar Disorder
Misdiagnosis of bipolar disorder is common, and these individuals may instead be diagnosed for years with schizophrenia and/or depression (Lawson 2005). African-Americans are much more likely to be under-or misdiagnosed and often receive a diagnosis of schizophrenia instead of bipolar disorder. It is also under-recognized in the correctional system with a third of inmates having unrecognized bipolar disorder (Kemp et al. 2008).
Recognizing and treating bipolar disorder is extremely important in the correctional system. The symptoms of the disorder involve impulsivity, pleasurable high-risk behavior, and irritability. Impulsive violent behavior, drug use, overspending, sexual assault, gambling, and disregard for the rights of others are all common in a manic episode and make these individuals especially vulnerable to arrest (Lawson 2005). The increased underdiagnosis among African-Americans makes the risk for arrest far greater than the likelihood for treatment. Secondly, bipolar disorder has been found to be the most single important factor in recidivism in jails (Quanbeck et al. 2005).
Schizophrenia
Individuals too impaired to make it in society may result to criminal activity to survive, resulting in the severely mentally ill ending up incarcerated. Many are regarded as criminals or psychopaths, and often the first time, a mental illness is diagnosed in jail or prison. Symptoms, such as impulsivity, poor judgment, callousness, a blunted affect, command hallucinations, and delusions, may be interpreted as antisocial or criminal especially for minorities. Once in the correctional system, individuals with schizophrenia are at great risk for being victimized. Upon release, transition to the outside world is especially difficult, leading to readmissions and recidivism especially when the diagnosis is not made. In addition, African-Americans are at increased risk of being perceived as hostile, further reducing the likelihood of treatment (Lawson 2007).
Preventing Misdiagnosis
Prison officials must be made aware of the risks associated with a misdiagnosis. A missed diagnosis increases the inmates’ risk of exploitation and suicide, and the correctional staff’s ability to prevent risks to themselves and other prisoners. Secondly, cultural awareness is important. Stereotypes about the rates of illness based on race must be discarded. An appreciation of cultural issues can increase diagnostic accuracy (Lawson 2005, 2007).
Language issues must be addressed as well. Many Latinos speak English as a second language. Outside of the prison setting, patients who speak English as a second language are more likely to be misdiagnosed as having schizophrenia when they have depression and may report different symptoms in their primary language. Limited English proficient individuals may be misdiagnosed, ignored, victimized, lack adherence to treatment, or may not receive appropriate and necessary treatment in the correctional system (Foulks 2004).
The use of screening tools can also be effective. Screening tools used with clinical judgment can lead to a greater likelihood of a valid diagnosis. Screening has been found to be effective in primary care settings which have successfully used various instruments to identify mental health illness (Gilbod et al. 2002). These instruments can be very brief and self-administered and often have good validity and reliability, although not all have been standardized in ethnic minority populations.
Non-Pharmacological Management
Psychotherapy can be effective in the correctional setting. Some contend that the practice of psychotherapy in prison is an unethical endeavor due to a lack of trust or confidentiality between the therapist and client and the possible threat of coercion. However, if these issues are addressed directly, a therapeutic relationship can be established. In fact, when therapy was provided, mental health providers offered a full range of services with goals that include mental illness recovery, emotions management, institutional functioning, reentry, risk-need, and personal growth, with the main focus being mental health recovery (Bewley and Morgan 2011). Moreover, many systems offer special areas of treatment that are key in the correctional system including: (1) management of self-mutilation, posttraumatic reactions (e.g., prison rape survivors), terminal illness, and crisis intervention, (2) maintenance of psychotic and major affective disorders, (3) outpatient therapy on adjustment issues and elective psychotherapy, and (4) treatment Programs for sex offender therapy and chemical dependency.
Moreover, various therapeutic approaches have been found to be effective. Meditation-based programs including Transcendental Meditation, mindfulness-based stress reduction, and 10-day Vipassana retreats have been found to enhance psychological well-being, decrease substance use, and decrease recidivism (Himelstein 2011).
Dialectical behavioral therapy has been used effectively as well. Various cognitive behavioral therapy approaches and interpersonal therapy have been shown to be effective in depression and anxiety disorders. Psychosocial interventions such as cognitive behavioral therapy (CBT), family interventions, and education programs have been found to be effective in maximum security settings (Walker 2004). Modified therapeutic communities modified for the correctional setting have been shown to be effective.
Pharmacotherapy
Despite the strong evidence for the effectiveness of psychosocial interventions, medication treatment is the primary mode of treatment within the correctional system (Thornburg 1995). Part of the reason may be the absence of personnel trained in psychosocial interventions. Another reason may be due to ethnic minorities who outside of the correctional system are thought to be poor psychotherapy candidates (Primm and Lawson 2010), leading to a decrease in the utilization of different types of psychotherapy.
Pharmacotherapy
One of the most prescribed medication groups are benzodiazepines which are safe, effective, and have less abuse potential than their older counterparts for anxiety and sedation. In the correctional system, benzodiazepines are used to address behavioral problems and a wide range of psychiatric disorders (Lerat et al. 2010). However, their overuse could lead to problems in the correctional system. The medications tend to contribute to disinhibition and tolerance is quickly acquired, making their use for many behavioral and psychiatric problematic. In an older study, violent or aggressive incidents occurred significantly more frequently in inmates on psychotropic medication than inmates who were not on psychotropic drugs. Of these, antianxiety agents (diazepam in 81 % of the cases) appeared to be the most implicated, with 3.6 times as many acts of aggression occurring when inmates were on these drugs (Workman and Cunningham 1975). Apparently the benefits were outweighed by the disinhibiting effects on behavior.
While these agents are less likely to be abused than most street drugs and older sedative/hypnotics, overuse and dependence often occur. To maintain control and order, hypnotics and sedatives such as benzodiazepines are often prescribed and their use is widespread among prisoners. Both illegal and medical drug use can occur in prison. Moreover, in this population in the jail/prison setting, drug-seeking behavior is frequently encountered. Prescribers usually take into account the potential for abuse before prescribing pain medications, benzodiazepines, and other hypnotic/sedative drugs, and they will reduce their use with guidelines and education. Nevertheless while agents such as SSRI are more likely prescribed by psychiatrists in the community to treat anxiety disorders, use of these agents to treat disorders in prisons remains widespread.
Some prescribed agents may not be abused in the community, but they are frequently abused in prison. Practitioners appear less likely to consider medications such as atypical antipsychotics and antidepressants as having the potential for abuse or dependence. Quetiapine (Seroquel®), an atypical antipsychotic, and Bupropion (Wellbutrin®), an SSRI antidepressant, have been identified as possible drugs of abuse within the correctional setting (Del Paggio 2005). Abuse was indicated by: (1) clinical presentations atypical at best; (2) doses that would be considered subtherapeutic for control of the reported “psychotic” symptoms; (3) refusal to consider other treatment options for their symptoms; (4) asking specifically for Seroquel® and Wellbutrin®, and (5) clinical presentations frequently suggested malingering of symptoms. Educational programs and close monitoring is often effective to combat this abuse.
As noted above, depression is common and often treated with antidepressants (Baillargeon et al. 2000). Antidepressants are effective in the correctional setting when the diagnosis is appropriately made, as shown by their increased use relative to other agents such as antipsychotics despite their cost and relatively strong adherence (Baillargeon et al. 2000). Although African-Americans are more likely to receive antidepressants in the correctional system, they are still less likely to receive them compared to Caucasians and more likely to receive them compared to Latinos.
Depression is strongly associated with suicide which is unfortunately not uncommon in the correctional system. As such, effective treatment of depression should have a positive effect on suicide rates within the correctional system. In fact, a marked decrease of suicide rates occurred after the introduction of SSRIs, and a significant association was seen between SSRIs, other new-generation antidepressants, and lower suicide rates, while TCAs are associated with higher suicide rates (Gibbons et al. 2005).
Antipsychotics have been widely used because of the incarceration of the severely ill and the need to treat aggressive behavior. The comparatively high acquisition costs of the newer antipsychotic medications have caused the mental health community to look closely at their potential benefits. Initiation of the atypical olanzapine therapy was associated with favorable clinical outcomes with the incarcerated mentally ill, particularly in patients with a formal diagnosis of thought disorder. The decline in total resource utilization was not statistically significant, although it may be of practical importance (Del Paggio et al. 2002).
Mood stabilizers have been useful as well because they are effective in treating both bipolar disorder, which disproportionately affects recidivism and aggression. Medication adherence is important in preventing re-incarceration and homelessness for those patients incarcerated with bipolar disorder and treated with mood stabilizers (Copeland et al. 2009). Lithium has been found to reduce aggression in a variety of settings including corrections (Muller-Oerlinghausen and Lewitzka 2010). Divalproex is effective in reducing impulsivity and mood liability in bipolar and non-bipolar patients. However, the impulsive/ aggressive subgroup was the only non-bipolar subgroup in which DVX yielded clinical benefit (Kamath et al. 2008). The author found that divalproex was effective in reducing disruptive behavior in both groups (Lawson and Nanos 2008).
Ethnopsychopharmacology
Ethnic differences have been reported for the metabolism of many psychotropic medications. Given the large ethnic minority populations in the correctional system, such findings are extremely relevant. African-Americans may require less medication than Caucasians due to differential pharmacological response (Bradford 2002). For instance, African-Americans may require lower doses of antipsychotic and antidepressant medications than Whites. Cytochrome P 450 enzymes metabolize over 90 % of drugs in clinical use including antipsychotic and antidepressant medications, and individuals with relatively inactive CYP2D6 alleles (which account for 25 % of metabolism of commonly used drugs) tend to have higher plasma levels of antipsychotics and antidepressants (Bradford 2002). However, 50 % of people of African ancestry have reduced functioning or nonfunctioning alleles, which lead to slower metabolism of older antipsychotics or tricyclic antidepressants and higher plasma levels. Chronically higher plasma levels may be associated with an increased risk of side effects, such as intolerance of the medication, which in turn can lead to poorer adherence to treatment. African-Americans are also more likely to develop tardive dyskinesia when receiving first-generation antipsychotics (Lawson 2007). A noted disparity in the provision of treatment is that African-Americans are more likely to be prescribed antipsychotics and are less likely to be prescribed newer antipsychotics or antidepressants (Lawson 2007). As mentioned above, African-Americans are also less likely to be offered different types of psychotherapy.
Many clinicians are unaware of potential racial/ethnic differences in pharmacological responses. For example, many anticipate that African-Americans will respond to medication similarly as other racial/ethnic groups do since considerable genetic similarities exist across such groups. Many also feel that African-Americans require more medication based on the misconception that African-American males are more hostile (Lawson 2002). However, the evidence suggests otherwise. Since the older medications are more likely to be metabolized by the CYP2D6 enzymes, African-Americans may be at greater risk of experiencing side effects when given the same dose as Whites because the drugs are metabolized more slowly. Moreover, since African Americans are more likely to be perceived of as being hostile or having schizophrenia, they may end up in receiving even higher doses and ultimately less likely to adhere to treatment after release.
Substance Abuse Pharmacotherapy
Substance abuse treatment has become an important intervention for reducing recidivism among inmates, especially since substance abuse is a major factor in the growth of US prison populations. However, pharmacotherapy has become an effective treatment in addressing drug abuse. An estimated 12–15 % of inmates have histories of heroin addiction (Mumola and Karberg 2006) and not surprisingly much of the research has involved opiate pharmacotherapy. The full agonist methadone and related agents have been found to be effective in addressing drug use problems in the correctional setting and post-release. Methadone treatment begun in prison and continued in the community upon release extended the time parolees remained in treatment, reduced further drug use, and produced a threefold reduction in criminal activity (Kimlock et al. 2009). A review of current studies showed that prerelease opiate maintenance therapy (OMT) was significantly associated with increased treatment entry and retention after release if arrangements existed to continue treatment. For other outcomes, associations with prerelease OMT were weaker but included post-release reductions in heroin use. Evidence regarding crime and re-incarceration was equivocal, but as noted above, some studies found positive results.
Buprenorphine is a long-acting partial agonist that acts on the same receptors as heroin and morphine, relieving drug cravings without producing the same intense “high” or dangerous side effects. Congress passed the Drug Addiction Treatment Act, permitting qualified physicians to prescribe Schedule III–V narcotic medications for the treatment of opioid addiction. This legislation created a major paradigm shift by allowing access to opiate treatment in a medical setting rather than limiting it to federally approved opioid treatment programs. Buprenorphine has advantages over methadone including less associated stigma; fewer regulations, which permit its use outside opioid treatment programs; and lower risk of overdose. Its combination with naloxone reduces the likelihood of intravenous abuse of the medication. It can be a valuable tool in addressing the problem of adherence since in 85–90 % of such persons relapsing to opioid use within 1 year after release, regardless of duration of incarceration (Kinlock et al. 2002). Overall, Buprenorphine has been found to be effective during incarceration and for post-release (Sullivan et al. 2006).
Corrections And Public Health
Since the first reports of HIV/AIDS occurring in US prison populations were published more than 25 years ago, epidemiologic studies have consistently documented a high prevalence of HIV infection and AIDS among prison inmates. The most recent estimates show that the prevalence of HIV infection in the US prison population is more than three times higher than that of the general population (Spaulding et al. 2009). Moreover, one-sixth of all infected individuals in the USA pass through the criminal justice system annually (Spaulding et al. 2009). Consequently, interventions are urgently needed for individuals with HIV disease who are transitioning back to the community. Moreover, 20 % of HIV-infected inmates released from prison were re-incarcerated within 3 years of their release date, creating a cycle of reinfection (Balergeon et al. 2010). Buprenorphine was associated with reduced relapse to opioid use and sustained viral suppression among released HIV-infected prisoners meeting criteria for opioid dependence (Springer et al. 2012) which helps combat this cycle of reinfection.
The impact of HIV infection and the cycle of reinfection on the African-American community is especially important. African-Americans have both higher HIV infection rates and have a greater representation in the correction system (El-Sadr et al. 2010). African-Americans have less access to services upon release (Primm and Lawson 2010).
Mental disorders also contribute to the spread of AIDS. Depression has been linked to disease progression in HIV, risky behaviors, and medication non-adherence. Moreover, treatment of depression leads to better adherence of HAART medications (Walkup et al. 2008). Unfortunately it is well documented that ethnic minorities have limited access to treatments for affective disorders which may further exacerbate the risk of the spread of AIDS in the African-American community (Primm and Lawson 2010).
Need For Integrated Treatment
Treatment in the correctional system must address the complex problem of substance use comorbidity. Because drugs of abuse affect similar brain circuits or receptor mechanisms proposed for mental disorders, they can cause drug abusers to experience one or more symptoms of mental illness (Lawson et al. 2011). When substance abusers present with similar symptoms of mental disorders, an underlying mental disorder may be missed and a drug abuser may be incarcerated rather than provided treatment. The result could be misdiagnosis and inappropriate treatment. Additionally, individuals with overt, mild, or even subclinical mental disorders may abuse drugs as a form of self-medication (Lawson et al. 2011). As a result, the mental disorder is considered yet another symptom of substance abuse, resulting in a delay in or absence of treatment for the mental disorder, especially in the correctional settings. Substance abuse adds to the burden by exacerbating mental illness and leading to a poorer outcome. In correctional systems, co-occurring disorders greatly exacerbate the rate of recidivism (Baillargeon et al. 2010). And, those with co-occurring substance abuse disorders are more likely to be held in jail longer than other inmates charged with similar crimes (McNiel et al. 2005). The combination of mental illness and drug abuse contributes to a revolving door of incarceration.
HIV means that many of these inmates may have three disorders, a triple whammy. It has already been noted that drug abuse worsens the outcome of HIV. Untreated mental illness is also associated with poor outcome for HIV. Treatment for comorbidity is inherently more difficult and often requires specialized services. Yet, such treatment is important and perhaps necessary to improve outcome and protect the community.
Ensuring Treatment
Mental health and drug courts are a valuable and effective source for early detection, referral, and navigation of services (Gallagher et al. 2011). They offer fresh insight into the potentially beneficial and detrimental effects of legal decisions and view one of the roles of law as that of a healing agent. At present, several states have instituted mental health courts based on these concepts; incorporating previous drug court experiences (Gallagher et al. 2011) in their development. Their goal is to avoid the criminalization of the mentally ill and their recidivism through the creation of special programs.
Mental health courts promote a nonadversarial atmosphere in which participants interact directly with the judge and in which praise and encouragement are issued far more often than sanctions. One program reported a significant drop in psychiatric hospitalization days for mentally ill participants and a decrease in positive drug and alcohol tests. Another mental health court program in Nevada reported successfully keeping mentally ill offenders out of the correctional system while concomitantly improving their mental condition. Mental health courts have been found to lower post-treatment arrest rates and days of incarceration (Steadman et al. 2010). While mental health and drug courts are not in and of themselves treatment and depend heavily on existing treatment resources, they are an important first step to providing services to improve adherence and linkage to post-release services.
Conclusion
The changing inmate population in the correctional system makes treatment essential to prevent recidivism and protect the community. We now have treatments that are effective in addressing mental disorders, substance abuse, and general medical problems such as AIDS. Most importantly, these treatments are shown to be effective in the correctional system and show strong benefits post release. Unfortunately, the issues that limit treatment in the community at large also impact the correctional community. As in the community, a large minority population, problems with disease recognition, need for integrated treatments, and barriers to treatment adherence exist in the correctional setting. Moreover, the culture of the system and financial challenges limit access to evidence-based treatment. Yet the need for ongoing and integrated treatment cannot be more urgent. For many with mental illnesses, substance abuse problems, or medical issues, the correctional system provides treatment opportunities for the first time in their lives. When they are released, it is essential that the cycle of high-risk behavior and recidivism is broken, both for the individual and the larger community. Educating the correctional system administrators and the general public on the benefits of evidence-based treatment is more important than ever. Recognition of mental disorders and substance abuse early in the process is crucial. Integrated service approaches combined with mental health/drug courts may produce the effective outcomes necessary for changing the life trajectories of former inmates. Dual diagnosis programs have now been introduced in many settings often with excellent results. However, many of those with comprehensive services in the correctional system discontinue them when released, which is why programs that promote adherence and linkage to services are essential (Foulks 2004). Providing early detection, personnel education, alternatives to incarceration, evidence-based treatment in corrections, and strong aftercare will be economically feasible and may help to reduce the disparities in health outcomes seen in ethnic minorities.
Bibliography:
- Alim TN, Graves E, Mellman TA, Aigbogun N, Gray E, Lawson W, Charney DS (2006) Trauma exposure, posttraumatic stress disorder and depression in an African-American primary care population. J Natl Med Assoc 98:1630–1636
- Baillargeon J, Contreras S, Grady JJ, Black SA, Murray O (2000) Compliance with antidepressant medication among prison inmates with depressive disorders. Psychiatr Serv 51(11):1444–1446
- Baillargeon J, Penn JV, Knight K, Harzke AJ, Baillargeon G, Becker EA (2010a) Risk of reincarceration among prisoners with co-occurring severe mental illness and substance use disorders. Adm Policy Ment Health 37:367–374
- Baillargeon J, Giordano TP, Harzke AJ, Spaulding AC, Wu ZH, Grady JJ, Baillargeon G, Paar DP (2010b) Predictors of reincarceration and disease progression among released HIV-infected inmates. AIDS Patient Care STDS 24(6):389–394
- Bewley MT, Morgan RD (2011) A national survey of mental health services available to offenders with mental illness: who is doing what? Law Hum Behav 35(5):351–363
- Bradford LD (2002) CYP2D6 allele frequency in European Caucasians, Asians, Africans and their descendants. Pharmacogenomics 3:229–243
- Copeland LA, Miller AL, Welsh DE, McCarthy JF, Zeber JE, Kilbourne AM (2009) Clinical and demographic factors associated with homelessness and incarceration among VA patients with bipolar disorder. Am J Public Health 99(5):871–877
- Crisanti AS, Frueh BC (2011) Risk of trauma exposure among persons with mental illness in jails and prisons: what do we really know? Curr Opin Psychiatry 24:431–435
- Del Paggio D, Finley PR, Cavano JM (2002) Clinical and economic outcomes associated with olanzapine for the treatment of psychotic symptoms in a county mental health population. Clin Ther 24(5):803–817
- El-Sadr WM, Mayer KH, Hodder SL (2010) AIDS in America – forgotten but not gone. N Engl J Med 362(11):967–970
- Fazel S, Seewald K (2012) Severe mental illness in 33,588 prisoners worldwide: systematic review and metaregression analysis. Br J Psychiatry 200(5):364–373
- Foulks EF (2004) Commentary: racial bias in diagnosis and medication of mentally ill minorities in prisons and communities. J Am Acad Psychiatry Law 32:34–35
- Gibbons RD, Hur K, Bhaumik DK, Mann JJ (2005) The relationship between antidepressant medication use and rate of suicide. Arch Gen Psychiatry 62:165–172
- Himelstein S (2011) Meditation research: the state of the art in correctional settings. Int J Offender Ther Comp Criminol 55(4):646–661
- Iguchi MY, Bell J, Ramchand RN, Fain T (2005) How criminal system racial disparities may translate into health disparities. J Health Care Poor Underserved 16:48–56
- James DJ, Glaze LE (2006) Mental health problems of prison and jail inmates, Bureau of Justice Statistics special report. Department of Justice, Washington, DC, NCJ Publication No. 213600
- Joe S, Baser RE, Breeden G, Neighbors HW, Jackson JS (2006) Prevalence of and risk factors for lifetime suicide attempts among blacks in the United States. J Am Med Assoc 296:2112–2123
- Kamath J, Temporini HD, Quarti S, Zhang W, Pagano KL, Demartinis N, Trestman RL (2008) Psychiatric use and utility of divalproex sodium in Connecticut prisons. Int J Offender Ther Comp Criminol 52(3):358–370
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE (2005) Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 62:593–602
- Kinlock TW, Battjes RJ, Schwartz RP (2002) A novel opioid maintenance program for prisoners: preliminary findings. J Subst Abuse Treat 22:141–147
- Lawson WB (2005) Bipolar disorder in African Americans in perspectives. In: Georgiopoulos AM, Rosenbaum JM (eds) Cross-cultural psychiatry. Lippincott Williams and Wilkins, Philadelphia, pp 135–142
- Lawson WB (2007) Schizophrenia in African Americans. In: Mueser KT, Jeste DV (eds) Clinical handbook of schizophrenia. Guilford, New York, pp 616–623
- Lawson WB (2008) Identifying interethnic variations in psychotropic response in African-
- Lewis DO, Shanok SS, Cohen RJ, Kligfeld M, Frisone G (1980) Race bias in the diagnosis and disposition of violent adolescents. Am J Psychiatry 137:1211–1216
- Muller-Oerlinghausen B, Lewitzka U (2010) Lithium reduces pathological aggression and suicidality: a mini-review. Neuropsychobiology 62(1):43–44
- Mumola C, Karberg J (2006) Drug use and dependence, state and federal prisoners. U.S. Department of Justice, Office of Justice Programs, Washington, DC
- Primm AB, Lawson WB (2010) Disparities among ethnic groups: African Americans. In: Ruiz P, Primm A (eds) Disparities in psychiatric care: clinical and cross-cultural perspectives. Wolters Kluver/Lippincott Williams & Wilkins, Baltimore, pp 19–29
- Spaulding AC, Seals RM, Page MJ, Brzozowski AK, Rhodes W et al (2009) HIV/AIDS among inmates of and releases from US correctional facilities, 2006: declining share of epidemic but persistent public health opportunity. PLoS One 4:e7558
- Springer SA, Qiu J, Saber-Tehrani AS, Altice FL (2012) Retention on buprenorphine is associated with high levels of maximal viral suppression among HIV-infected opioid dependent released prisoners. PLoS One 7(5):e38335. doi:10.1371
- Steadman HJ, Redlich A, Callahan L, Robbins PC, Vesselinov R (2010) Effect of mental health courts on arrests and jail days: a multisite study. Arch Gen Psychiatry 68:167–172
- Strakowski SM, Keck PE Jr, Arnold LM, Collins J, Wilson RM, Fleck DE, Corey KB, Amicone N, Adebimpe VR (2003) Ethnicity and diagnosis in patients with affective disorders. J Clin Psychiatry 64:747–754
- Sullivan LE, Barry D, Moore BA, Chawarski MC, Tetrault JM, Pantalon MV, O’Connor PG, Schottenfeld RS, Fiellin DA (2006) A trial of integrated buprenorphine/naloxone and HIV clinical care. Clin Infect Dis 43(4):S184–S190
- Walker H (2004) Using psychosocial interventions within a high-security hospital. Nurs Times 100(31):36–39
- Walkup W, Wei W, Sambamoorthi U, Crystal S (2008) Antidepressant treatment and adherence to combination antiretroviral therapy among patients with AIDS and diagnosed depression. Psychiatr Q 79(1):43–53
- Workman D, Cunningham D (1975) Effect of psychotropic drugs on aggression in a prison setting. Can Fam Physician 21(11):63–66
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.





