This sample Epilepsy Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Introduction
Epilepsy is a common and often debilitating neurological disorder among persons of all ages and socioeconomic backgrounds. Epilepsy is unique inasmuch as its full impact on the affected individual extends beyond seizures, the primary symptom of epilepsy, to include associated cognitive, behavioral, affect, interpersonal, cultural, and societal aspects. While current medical therapies successfully eliminate seizures in up to two-thirds of patients, a substantial proportion of persons with epilepsy have inadequate seizure control and a disproportionate psychosocial burden. This research paper provides an overview of the epidemiology of epilepsy, how it is diagnosed and treated, the psychosocial aspects associated with epilepsy, and challenges for improving the health and well-being of persons with epilepsy in developing countries.
Epidemiology Of Epilepsy
Epilepsy is one of the most common neurological disorders and has been recognized since antiquity. An estimated 2 to 4 million people in the United States have epilepsy, including 1 of 50 children, 1 of 100 adults, and 1 million women of childbearing age (Hauser and Hesdorffer, 1990; Devinsky and Yerby, 1994). In addition, 200 000 new cases are diagnosed every year. In 2000, the annual cost of epilepsy in the United States was reported as $12.5 billion (Begley et al., 2000). Worldwide, approximately 50 million persons have epilepsy, the majority of whom cannot afford or do not have access to appropriate medical therapy.
Epilepsy can develop at any age, though a disproportionate number of cases begin in the young and elderly. Because the prevalence of epilepsy among the elderly is steadily increasing in many countries as their population ages, it has been predicted that within a few decades more than half of the patients in developed countries who develop epilepsy will be over the age of 65. Contributing factors to the onset of epilepsy in this age group are Alzheimer’s disease and other degenerative conditions of the central nervous system, cerebrovascular disease, brain tumors, head injuries, and alcohol or drug abuse.
Epilepsy is not benign and is associated with an increased risk of mortality. Causes of death among persons with epilepsy include accidental deaths (for example, drowning), sudden and unexplained death in epilepsy, status epilepticus (a condition of repeated seizures without recovery), underlying brain disease (such as brain tumors), and suicide. People with uncontrolled seizures are also at increased risk for injuries, such as bone fractures and burns.
Diagnosis And Medical Management
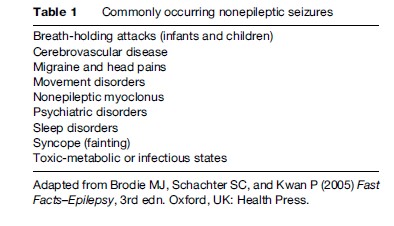
A seizure is a sudden change in behavior that may or may not be apparent to others. Not all sudden changes in behavior are seizures, and not all seizures are epileptic seizures. Whereas epileptic seizures result when the electrical activities of neuronal networks in the brain suddenly become hypersynchronized, non-epileptic seizures resemble epileptic seizures but actually reflect the response of an otherwise normal brain to a systemic physiological change, the behavioral manifestations of a psychiatric disorder, or other neurological conditions besides epilepsy. Consequently, while all patients with epilepsy have seizures, the converse may not be true. The most common causes of non-epileptic seizures are syncope (fainting); transient global amnesia (a condition characterized by prolonged loss of recent memory); metabolic disorders, including hyponatremia, hypoglycemia, and hypocalcemia; movement disorders, generally referred to as paroxysmal dyskinesias; sleep disorders; panic attacks; and psychogenic seizures, which are usually attributed to stressful psychological conflicts or major emotional trauma, such as sexual or physical abuse in childhood, a death, or divorce (Table 1). Of these conditions, non-epileptic seizures resulting from syncope and psychogenic causes are perhaps the most difficult to differentiate from epileptic seizures.
The purpose of the initial medical evaluation of a patient who has had his or her first seizure is to exclude other conditions that cause non-epileptic seizures and to determine if there is an underlying brain lesion, as assessed by computed tomography (CT) or magnetic resonance imaging (MRI). Initial laboratory studies include glucose, calcium, and magnesium levels, hematology, renal function tests, and toxicology screens. Electroencephalograms (EEGs) are helpful to support a diagnosis of epilepsy and to help classify a patient’s epileptic seizure type as generalized or partial, as discussed below. However, initial EEGs may be normal in over half of patients with epilepsy.
Epilepsy is operationally defined as the tendency for a person to have recurrent epileptic seizures. The causes of epilepsy vary according to the age at onset of epilepsy, and include congenital brain malformations, inborn errors of metabolism, brain trauma, brain tumors, stroke, intracranial infection, vascular malformations, and cerebral degeneration. However, up to half of patients with epilepsy do not have an identifiable underlying cause when evaluated with currently available diagnostic tests.
Epilepsy is usually diagnosed after a patient has had two or more epileptic seizures. The goals of therapy are to treat the underlying cause, if known and if remediable to treatment, and to completely suppress further seizures from occurring without causing troublesome side effects from the therapy. Antiepileptic drugs (AEDs) are the primary form of seizure-suppression therapy, and must be taken on a daily basis. Initial treatment achieves seizure freedom in up to 70% of patients, but prognosis for seizure control in the other 30% of patients is less favorable. These patients usually require numerous trials of AEDs, either as monotherapy or combination therapy, often require higher AED dosages, and typically must endure daily side effects. Such patients are said to have medically intractable epilepsy and may be candidates for adjunctive nonpharmacological treatments, including vagus nerve stimulation, brain surgery, special diets, stress reduction techniques, or investigational drugs or brain stimulation devices. Patients with medically intractable seizures require frequent visits to health-care professionals and periodic reassessment with EEGs and MRI scans, particularly if there is progressive worsening of the patient’s neurological examination or cognitive function, or an increase in seizure frequency or severity. For all these reasons, the human and financial costs associated with medically intractable epilepsy are much greater than when epilepsy readily comes under control with initial therapy or goes into remission.
Physicians usually select an AED according to the patient’s seizure type, which in turn is based on the description of the seizure as obtained from the patient and/or eyewitnesses. Other considerations for selecting an AED are the pharmacokinetic profile of the drug, the patient’s age and comorbid medical and psychiatric conditions, whether the patient is a woman of childbearing potential, the potential for adverse effects and drug–drug interactions, and cost. With the exception of medical emergencies, therapy is usually initiated with a low dose and increased slowly until seizures are completely controlled, or until bothersome side effects occur that persist, at which time the dose is lowered to minimize side effects.
The two main seizure types are generalized and partial seizures, as shown in Table 2. Generalized seizures affect both sides of the brain simultaneously when the seizure begins and are usually not associated with identifiable brain pathology. Absence seizures, myoclonic seizures, and generalized tonic-clonic seizures are among the subtypes of generalized seizures.
- Absence seizures cause the sudden onset of staring with impaired consciousness. They typically begin in childhood, last between 5 to 10 s, and may occur dozens if not hundreds of times a day, particularly in association with boredom and hyperventilation. Up to 90% of patients undergo a spontaneous remission of their epilepsy before reaching adulthood.
- Myoclonic seizures consist of sudden, brief, shock-like contractions affecting the arms, legs, face, or trunk, often occurring in the early morning.
- Generalized tonic-clonic seizures (also called grand mal seizures or convulsions) may begin with a loud noise or scream. The arms and legs then stiffen (tonic phase), the patient falls to the ground, and the patient’s lips and skin appears dusky (cyanotic). After 60 to 90 s, the arms and legs start to jerk (convulse), eventually in unison, for an additional 1 to 2 min (clonic phase). Bloody, frothy sputum may be seen coming from the mouth. After the clonic phase ends, the patient appears to be in a deep sleep, and then wakes up gradually over minutes to hours, often sleepy, confused and complaining of a severe, throbbing headache.
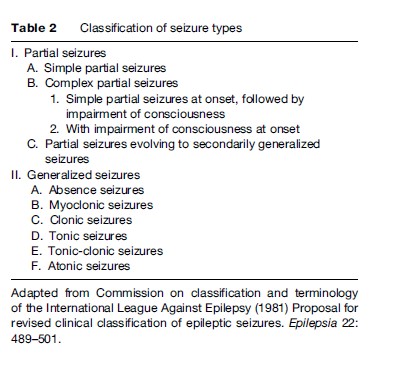
At their onset, partial seizures affect a restricted area of cortex (the outer layer of the brain) and usually suggest the presence of an underlying brain lesion, whether or not apparent on CT or MRI scans. Symptoms that patients with partial seizures experience when the seizure begins may not be apparent to others and are called simple partial seizures – ‘simple’ meaning that consciousness is not impaired. Patients may refer to these symptoms as auras or warnings, and they may include nausea, fear, jerking of one side of the body, or a metallic taste. Many other symptoms may occur with simple partial seizures as well. Other patients do not have a conscious warning at the start of their partial seizures and abruptly lose consciousness. This type of partial seizure is called a complex partial seizure – ‘complex’ meaning that consciousness is impaired. Complex partial seizures (known in the past as temporal lobe seizures and psychomotor seizures) are the most common type of seizure experienced by adults with epilepsy. During complex partial seizures, patients typically appear awake but do not meaningfully interact with people or objects around them and do not respond normally to instructions or questions. They appear to stare and either remain still or demonstrate repetitive nonpurposeful behaviors (called automatisms), such as chewing, lip smacking, repeating words or phrases, aimless walking or running, or undressing. If patients are forcibly restrained or redirected during complex partial seizures, they may become aggressive. Complex partial seizures typically last less than 3 min and may be immediately preceded by a simple partial seizure or followed by a tonic-clonic seizure. After complex partial seizures, patients may appear confused or somnolent, and may complain of a headache. Because their consciousness is impaired, patients have no memory of what happened during complex partial seizures.
Besides identifying the type(s) of seizure a patient has, clinicians determine whether a patient has an identifiable epilepsy syndrome, which is defined by specific seizure types, age of epilepsy onset, family history, response to particular AEDs, and prognosis.
The number and availability of pharmacological (AED) and nonpharmacological treatment options for patients with epilepsy have steadily increased over the past 10 to 20 years, as briefly described below. Successful use of AEDs requires detailed knowledge of their pharmacodynamic and pharmacokinetic properties, an understanding of the pertinent published safety and efficacy studies, and individualized therapy to a particular patient. Recently published guidelines from the American Academy of Neurology and the American Epilepsy Society for the use of the newer AEDs in the treatment of new-onset and medically refractory seizures are based on published studies of efficacy, tolerability, and safety in adults and children (French et al., 2004a, 2004b). However, there are numerous clinical situations requiring an AED treatment decision for which there are few if any relevant clinical studies. In such circumstances, expert opinion can provide some direction to the clinician. The most recent compilation of expert opinion was based on data obtained in 2004 from 48 American epilepsy specialists covering all of the newer AEDs except for pregabalin (Karceski et al., 2005).
To be effective, AEDs must enter the brain; consequently, AEDs often cause dose-related side effects that are due to brain dysfunction, such as sleepiness, trouble with balance, or double vision. Side effects are a major cause of medication intolerance and noncompliance, particularly within the first 6 months of therapy.
If a trial of the first AED is unsuccessful either because seizures are not controlled or side effects are bothersome, then a second AED, also appropriate for the patient’s seizure type(s), is prescribed. The second AED is usually titrated to a tolerable and effective dosage before the first AED is tapered and stopped, unless the first AED caused a side effect requiring immediate discontinuation. While it is preferable to maintain a patient on a single AED rather than AED combinations because of enhanced compliance, lower medications costs, and generally fewer complications, some patients have better seizure control on combinations of AEDs than on individual drugs.
The selection of AEDs for women of childbearing potential is particularly important because all AEDs can potentially cause birth defects, especially when taken in combination. The overall risk of birth defects in the offspring of women with epilepsy who take an AED is approximately twice the expected rate, and risks are higher with combination therapy. The most frequently occurring birth defects are neural tube defects, cleft lip and palate, heart defects, and reduced brain size. Physicians often recommend that women on AEDs take between 0.4 and 4 mg/day of folic acid for a prolonged period before conceiving to reduce the risk of birth defects, but the health benefits of this practice to the fetus have not been proven in this population.
Currently available AEDs suppress the occurrence of seizures, but there is no evidence that they cure epilepsy or prevent the onset of seizures in patients at high risk, such as those who suffer a serious brain injury. Therefore, patient adherence to the AED dosing schedule on a daily basis is crucial for maintaining seizure control. Failure to take medications as prescribed can lead to an increase in seizures and/or medication side effects. Causes of noncompliance include memory lapses, complicated AED regimens, denial of illness, and fixed incomes. Patients must be educated about the importance of regularly taking seizure medication.
Primary care physicians or emergency room physicians often make the initial diagnosis of epilepsy and begin therapy. Patients are often referred to neurologists for further diagnostic evaluation and additional therapeutic trials if seizures do not respond to initial therapy, or to assess the feasibility of withdrawing AEDs if they have been seizure-free for 2 or more years. Epileptologists are neurologists who specialize in epilepsy, and are usually located at centers that have access to investigational treatments and sophisticated surgical procedures for the evaluation and treatment of medically intractable epilepsy. The psychosocial consequences of epilepsy, described later, may require the involvement of other specialists, such as psychiatrists, psychologists, neuropsychologists, social workers, and vocational counselors.
Antiepileptic Drugs
Antiepileptic drugs vary based on their mechanisms of action on brain neurons, the seizure type(s) they effectively control, pharmacokinetic properties, side effect profile, teratogenicity, and propensity for drug–drug interactions.
Carbamazepine (CBZ) blocks voltage-dependent sodium channels on neuronal membranes, thereby preventing neurons from firing as rapidly as needed to sustain a seizure. CBZ is used for partial seizures and generalized tonic-clonic seizures, and should be initiated at 100 to 200 mg daily and increased by 100 to 200 mg every 3 to 14 days as needed for seizure control, typically over a period of 1 to 2 months. Common side effects are double vision, headache, dizziness, and nausea and vomiting, which can be lessened by use of a controlled-release formulation. Other possible side effects include mild or serious rashes and reversible decreases in white blood cells. Potentially fatal effects on bone marrow or liver are fortunately very rare. CBZ can cause birth defects, including spina bifida. One of the difficulties in administering CBZ arises from its effects on increasing the metabolism of other drugs; hence, drug–drug interactions are common.
Ethosuximide (ESM) works by reducing calcium currents in neurons of the thalamus, a deep nuclear structure in the brain. ESM is a first-line treatment for patients with absence seizures. The usual starting dose is 250 to 500 mg daily, with 250-mg dose increments over 2 to 3 weeks as needed for seizure control. Side effects are infrequent and include hiccups, nausea and vomiting, abdominal pain, lack of appetite, headache, dizziness, drowsiness, and unsteadiness. Allergic rashes occur infrequently.
Felbamate (FBM) has several mechanisms of action and is effective against partial seizures as well as generalized seizures that occur with a particularly severe epilepsy syndrome in children called the Lennox-Gastaut syndrome. As with other AEDs, dosing is advanced slowly to minimize side effects, which include insomnia, headache, nausea and vomiting, loss of appetite, sleepiness, weight loss, and dizziness. FBM is associated with an elevated risk of potentially fatal bone marrow suppression and hepatitis. While routine monitoring of liver and blood counts is recommended, the results do not predict potentially fatal toxicity. Consequently, FBM is now primarily used in patients with Lennox-Gastaut syndrome, and only when the benefits of treatment are judged to outweigh the risks. FBM can affect other drugs by increasing their metabolism in the liver.
Gabapentin (GBP) binds to voltage-gated calcium channels on neurons, inhibiting the flow of calcium ions, and is effective against partial seizures. The usual starting dose is 300 mg daily, which is increased by 300 mg every 3 days as needed for seizure control to the maximum tolerated dose. Typical side effects are drowsiness, dizziness, weight gain, fluid retention, and trouble with balance. GBP has no known effects on other drugs. Because GBP is excreted by the kidneys, dosage requirements for patients with kidney dysfunction are less.
Lamotrigine (LTG), like CBZ, blocks voltage-dependent sodium channels on neuronal membranes and is effective against partial seizures and generalized tonic-clonic seizures. Dosing is initiated at 25 to 50 mg daily, and increased slowly to reduce the likelihood of rash, especially in patients who also are taking valproate. Common side effects are rash, headache, nausea and vomiting, insomnia, dizziness, double vision, trouble with balance, and tremor. Severe, potentially life-threatening, skin reactions occur in up to 1 in 1000 adults and 1 in 100 children. Recent data from a pregnancy registry suggest an increased risk to babies of isolated cleft lip or palate when LTG is taken during the first trimester of pregnancy.
Levetiracetam (LEV) affects the currents of two inhibitory neurotransmitters in the brain – GABA and glycine – although whether these actions account for the mechanism of action of LEV is unclear. It is effective against partial and generalized seizures, including myoclonic and absence seizures. The starting dosage is 500 to 1000 mg daily, which is increased by 1000 mg every 2 weeks as tolerated and needed for seizure control. Patients with kidney dysfunction require lower dosages. Side effects include somnolence, headache, lack of appetite, nervousness, and, less frequently, agitation, aggression, anxiety, or depression. LEV has no effects on other drugs.
Oxcarbazepine (OXC) works similarly to CBZ and LTG on neuronal membranes. It is quickly metabolized in the body to an active metabolite. OXC is used to treat partial seizures and generalized tonic-clonic seizures. Dosage is started at 150 to 600 mg daily in adults and increased every 1 to 2 weeks as tolerated and as needed to control seizures. Side effects include drowsiness, dizziness, headache, double vision, nausea and vomiting, trouble with balance, and rash.
Phenobarbital (PB) amplifies the inhibitory effect of GABA on brain neurons and is used for partial seizures, generalized tonic-clonic seizures, and myoclonic seizures. PB is the least expensive AED, but is generally viewed as a second-line drug because many patients experience side effects, such as sleepiness, depression, and agitation. An intravenous form of PB is useful for seizure emergencies. Adult dosages range from 60 to 240 mg/day. PB has been associated with birth defects and drug–drug interactions.
Phenytoin (PHT) blocks voltage-dependent neuronal sodium channels and is used for partial seizures and generalized tonic-clonic seizures. An intravenous formulation is useful for seizure emergencies. Typical dose-related side effects are rash, trouble with balance, slurred speech, and sleepiness. Long-term use may cause swelling of the gums (gingival hyperplasia), hair growth, acne, thinning of the bones, and peripheral nerve dysfunction. Very serious side effects, such as hepatitis, bone marrow suppression, swelling of the lymph nodes, and a potentially fatal rash, are very rare. On the other hand, drug–drug interactions are common. Phenytoin has been associated with birth defects.
Pregabalin (PGB) works in a similar manner as GBP, and is effective for the treatment of partial seizures. The starting dose is 150 mg/day, with subsequent titration every week to an effective and tolerable maintenance dose. Common side effects are dizziness, sleepiness, headache, trouble with balance, weight gain, and peripheral fluid retention. PGB has no known effects on other drugs. Because PGB is excreted by the kidneys, target dosages for patients with kidney dysfunction are lower than in patients with normal kidney function.
Primidone (PRM) is converted by the liver to PB and another active compound. PRM is used for partial seizures and generalized tonic-clonic seizures, but it is considered a second-line treatment because of sedating side effects and reduced sex drive. The initial dose is usually 125 mg at bedtime, with 125 mg increments every 3 to 5 days as needed for seizure control and as tolerated. PRM causes drug–drug interactions.
Sodium valproate (VPA) has several mechanisms of action, and is effective for all seizure types. The initial dosage is 500 to 1000 mg/day, with subsequent titration as needed and tolerated. Tremor is a dose-related side effect; weight gain and hair thinning may also occur. Rarely, serious effects on platelet counts, the pancreas, and the liver may be seen. VPA has been associated with birth defects, especially neural tube defects. VPA inhibits the metabolism of a number of drugs, including PHT, PB, the primary metabolite of CBZ, and LTG; therefore, drug–drug interactions are common.
Tiagabine (TGB) augments the effects of the inhibitory neurotransmitter GABA and is used to treat partial seizures. Treatment commences with 4 to 8 mg daily, and the dosage is increased weekly or more slowly by 4 to 8 mg as needed for control of seizures and as tolerated. Side effects are related to daily dose and rate of titration, and include dizziness, fatigue, muscle weakness, nervousness, tremor, impaired concentration, lethargy, and depression. Drug–drug interactions may occur, and required doses are reduced in patients with significant liver dysfunction.
Topiramate (TPM) has several mechanisms of action and is used for partial seizures, generalized tonic-clonic seizures, and myoclonic seizures. Treatment is initiated at 25 to 50 mg/day and increased by 25 to 50 mg every 1 to 2 weeks as needed for seizure control and as tolerated. Side effects include a language disorder characterized by word-finding difficulty, slowing of cognition, trouble with balance, dizziness, fatigue, numbness and tingling, reduced appetite, and weight loss. Rare side effects include kidney stones, decreased sweating, and acute angle closure glaucoma. Drug interactions may occur, especially with hormonal contraceptives, PHT, and CBZ.
Zonisamide (ZNS) has several mechanisms of action and is used for partial seizures and generalized seizures. The starting dose is 100 mg daily for adult patients, which is usually increased every 2 weeks as needed and tolerated. Typical side effects are lack of appetite, dizziness, trouble with balance, fatigue, sleepiness, and confusion. Rare side effects include kidney stones and decreased sweating. Drug interactions may occur.
Nonpharmacological Therapies
Several nonpharmacological therapies are available for selected patients whose seizures do not satisfactorily respond to AEDs. These include brain surgery, vagus nerve stimulation, dietary approaches, such as the ketogenic diet and the modified Atkins diet, and a variety of stress-reduction techniques. Ongoing treatment with AEDs is generally maintained. Among the nonpharmacological therapies, brain surgery offers the greatest potential for complete seizure control, especially when seizure onset can be localized with sophisticated EEG testing to the inner part of the temporal lobe and when the underlying pathology is determined by brain imaging studies to be a condition known as mesial temporal sclerosis. With the exception of stress-reduction techniques, nonpharmacological therapies generally require extensive and expensive evaluations and are primarily offered at comprehensive epilepsy centers.
Psychosocial Aspects Of Epilepsy
Patients with epilepsy often experience an unsatisfactory quality of life because of a variety of epilepsy-related psychosocial factors, such as stigma and psychiatric comorbidity.
Stigma adversely affects patients with epilepsy, especially those with difficult-to-control seizures, and particularly in developing, resource-poor countries. Perceived and enacted stigma impact on nearly all everyday activities of persons with epilepsy, such as attending school, driving, working, enjoying recreational activities, establishing social relationships, and obtaining insurance. Even patients who are seizure-free and well informed about their disorder may experience unemployment and underemployment, driving restrictions, difficulty obtaining life and health insurance, and social stigmatization.
Psychiatric comorbidity is common in patients with epilepsy. The most frequent associated psychiatric condition is depression, occurring in 10–20% of patients with controlled seizures and up to 60% of patients with medically intractable epilepsy. Depression is underdiagnosed and undertreated in patients with epilepsy, in part because of the largely unjustified concern that all antidepressant drugs could exacerbate seizures. Undertreatment is a major problem, because suicide is a frequent cause of death in patients with epilepsy, occurring up to 10 times more frequently than in the general population.
Up to 25% of patients with epilepsy have anxiety, most commonly in the form of a generalized anxiety disorder. The severity of anxiety may not correlate with seizure frequency. Ironically, severe anxiety may develop after a patient with epilepsy becomes seizure-free. Apart from having an anxiety disorder, living with fear is common among people with epilepsy and is often reported as ‘the worst thing about having epilepsy’ (Fisher et al., 2000a, 2000b). Specific fears include dying from a seizure, public embarrassment, losing employment, and being involved in an automobile accident.
Reducing The Global Burden Of Epilepsy
The recognition that epilepsy is a multifaceted disorder consisting of seizures, underlying brain dysfunction, and numerous psychosocial complications has prompted major efforts around the world to identify and overcome the barriers to optimum quality of life for persons with epilepsy.
Public health initiatives have sought to improve education about epilepsy among health-care practitioners, ministers, teachers, rescue personnel, and the general public. For example, epilepsy-related initiatives of the United States Centers for Disease Control and Prevention have focused on improving care; enhancing communication and combating stigma; self-management, disease surveillance and prevention research; increasing public awareness and knowledge; and strengthening partnerships with other organizations such as the Epilepsy Foundation (Schachter, 2001). Reducing stigma is the primary objective of Out of the Shadows, a global campaign of the International League Against Epilepsy, the World Health Organization, and the International Bureau for Epilepsy, but this effort can be particularly challenging among cultures that continue to view epilepsy as the result of supernatural forces, as was more pervasive centuries ago.
In addition to education, public health agencies are attempting to improve access to appropriate medical care for the millions of patients with epilepsy worldwide who currently have no access to treatment or cannot afford appropriate medications.
Bibliography:
- Begley CE, Famulari M, Annegers JF, et al. (2000) The cost of epilepsy in the United States: As estimate from population-based clinical and survey data. Epilepsia 41: 342–351.
- Brodie MJ, Schachter SC, and Kwan P (2005) Fast Facts–Epilepsy, 3rd edn. Oxford, UK: Health Press.
- Devinsky O and Yerby MS (1994) Women with epilepsy: Reproduction and effects of pregnancy on epilepsy. Neurologic Clinics of North America 12: 479–495.
- Fisher RS, Vickrey BG, Gibson P, et al. (2000a) The impact of epilepsy from the patient’s perspective I: Descriptions and subjective perceptions. Epilepsy Research 41: 39–51.
- Fisher RS, Vickrey BG, Gibson P, et al. (2000b) The impact of epilepsy from the patient’s perspective II: Views about therapy and health care. Epilepsy Research 41: 53–61.
- French JA, Kanner AM, Bautista J, et al. (2004a) Efficacy and tolerability of the new antiepileptic drugs I: Treatment of new onset epilepsy: Report of the Therapeutics and Technology Assessment Subcommittee and Quality Standards Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology 62: 1252–1260.
- French JA, Kanner AM, Bautista J, et al. (2004b) Efficacy and tolerability of the new antiepileptic drugs II: Treatment of refractory epilepsy: Report of the Therapeutics and Technology Assessment Subcommittee and Quality Standards Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology 62: 1261–1273.
- Hauser WA and Hesdorffer DC (1990) Epilepsy: Frequency, Causes, and Consequences. New York: Demos.
- Karceski S, Morrell MJ, and Carpenter D (2005) Treatment of epilepsy in adults: Expert opinion, 2005. Epilepsy & Behavior 7(Supplement 1): S1–S64.
- Schachter SC (2001) Ongoing epilepsy program activities at the Centers for Disease Control and Prevention. Epilepsy & Behavior 2: 381–383.
- Artama M, Auvinen A, Raudaskoski T, Isojarvi I, and Isojarvi J (2005) Antiepileptic drug: use of women with epilepsy and congenital malformations in offspring. Neurology 64: 1874–1878.
- Asconape JJ (2002) Some common issues in the use of antiepileptic drugs. Seminars in Neurology 22: 27–39.
- Barry JJ and Jones JE (2005) What is effective treatment of depression in people with epilepsy? Epilepsy & Behavior 6: 520–528.
- Beyenburg S, Mitchell AJ, Schmidt D, Elger CE, and Reuber M (2005) Anxiety in patients with epilepsy: Systematic review and suggestions for clinical management. Epilepsy & Behavior 7: 161–171.
- Boro A and Haut S (2003) Medical comorbidities in the treatment of epilepsy. Epilepsy & Behavior 4(supplement 2): 2–12.
- Brodie MJ, Schachter SC, and Kwan P (2005) Fast Facts–Epilepsy, 3rd edn. Oxford, UK: Health Press.
- Jacoby A, Snape D, and Baker GA (2005) Epilepsy and social identity: The stigma of a chronic neurological disorder. Lancet Neurology 4: 171–178.
- Kanner AM and Barry JJ (2003) The impact of mood disorders in neurological diseases: Should neurologists be concerned? Epilepsy & Behavior 4(Supplement 3): 3–13.
- Kwan P and Brodie MJ (2000) Early identification of refractory epilepsy. New England Journal of Medicine 342: 314–319.
- Levy RH, Mattson RH, Meldrum BS and Perucca E (eds.) (2002) Antiepileptic Drugs, 5th edn. Philadelphia, PA: Lippincott Williams and Wilkins.
- Loring DW, Meador KJ, and Lee GP (2004) Determinants of quality of life in epilepsy. Epilepsy & Behavior 5: 976–980.
- Meinardi H, Scott RA, Reis R, and Sander JW (2001) The treatment gap in epilepsy: The current situation and ways forward. Epilepsia 42: 136–149.
- Schachter SC (2006) Quality of life for patients with epilepsy is determined by more than seizure control: The role of psychosocial factors. Expert Review of Neurotherapeutics 6: 111–118.
- Schachter SC and Andermann L (eds.) (2003) The Brainstorms Village: Epilepsy in our World. Philadelphia, PA: Lippincott Williams and Wilkins.
- Wyllie E, Gupta A and Lachhwani DK (eds.) (2006) The Treatment of Epilepsy. Philadelphia, PA: Lippincott Williams and Wilkins.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.







