This sample Lymphomas Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Introduction
The lymphomas encompass a group of distinct hematologic malignancies which arise from T and B lymphocytes. These lymphatic neoplasms are typically categorized as Hodgkin or non-Hodgkin lymphomas. Hodgkin lymphomas (HL) are derived from B cells or their progeny and are distinguished by the presence of multinucleated Reed-Sternberg cells. Non-Hodgkin lymphomas (NHL) are classified by the World Health Organization (Jaffe and Harris, 2001) into 21 subtypes of B-cell and 15 subtypes of T-cell malignancies; NHL account for about 80–90% of all lymphomas. Lymphomas vary in their clinical presentation, course, treatment strategies, and long-term prognosis. The diversity of lymphoma subtypes suggests that etiologic factors may also differ, which contributes to the complexities of disease investigation. While some factors associated with an increased risk of these cancers have been identified, the elucidation of clear etiologic determinants and their mechanistic role in pathogenesis has been challenging.
Epidemiology
Worldwide, there are approximately 363 000 new cases of lymphoma annually, accounting for 3.3% of all cancers. Lymphoma claims about 195 000 lives each year. In the United States, lymphoma is the fifth most commonly occurring malignancy, with an incidence rate of 21.8 per 100 000. These cancers are slightly more common in males (26.0/100 000) than in females (18.4/100 000). Regarding race, Whites are at greater risk than Blacks. Hispanic ethnicity is associated with a decreased risk of lymphoma. Age-related patterns of disease differ between
HL and NHL. The incidence of NHL increases dramatically with aging. The median age of diagnosis is about 64 years, with only 3% of cases diagnosed under 20 years of age. In contrast, in developing countries, HL occur predominantly during childhood and incidence decreases with age. Among industrialized nations, the distribution of HL is bimodal with peaks in the third and fifth decades of life. There is significant disparity in lymphoma incidence related to economic development, with the highest rates observed in the most developed countries. Improved diagnostics, more complete reporting, greater exposures to potential environmental carcinogens, decreased childhood exposure to disease-related pathogens resulting in decreased immunity, and differences in racial distributions may account for these differences in disease incidence. The rates of different lymphoma subtypes are also subject to significant regional and international variation, likely due to differences in prevalence of etiologic factors.
Trends In NHL Incidence
In most Western countries, unprecedented increases of about 3–4% each year in lymphoma incidence rates were observed from the 1970s to early in the 1990s, regardless of age, gender, or race (Figure 1).
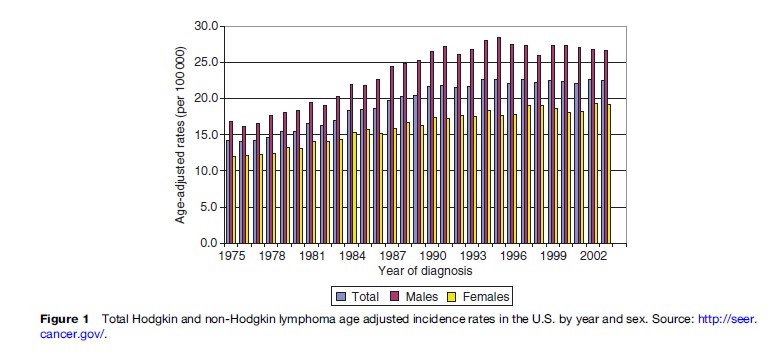
In particular, incidence in males, ages 25–54, underwent dramatic escalation, mostly related to the HIV epidemic. A sharp rise in the incidence of extranodal primary lymphomas, particularly those of the brain, has also been documented. Factors that may account in part for this startling escalation in disease incidence include: improved cancer reporting, more sensitive diagnostic techniques particularly for borderline lesions, changes in classification of lymphoproliferative diseases, and, in particular, the increasing occurrence of AIDS-associated lymphomas.
Since 1995, lymphoma incidence among males in many countries has decreased, reflecting the improved immune status of those with HIV/AIDS resulting from the introduction of highly active anti-retroviral therapy (HAART). However, available data suggest that the nonAIDS-related lymphoma incidence rates have continued to increase at a rate of approximately 1% per year, specifically among females, older males, and Blacks in the United States.
Clinical Aspects Of Lymphoma
The presentation of both HL and NHL depends on the specific lymphocytic tissue involved in the malignancy. Typically, disease is localized at onset and subsequently spreads by contiguity within the lymphatic system. Localized symptoms may be limited to a painless enlargement of a single lymph node. As the cancer disseminates, however, systemic symptoms develop which often mimic an infectious process. Fever, night sweats, fatigue, weight loss, shortness of breath, and itching skin are common. Diagnosis is made by histologic examination of biopsy tissue. Morphologic, immunophenotypic, genetic, and clinical characteristics also contribute to determination of the diagnostic classification and to the disease prognosis.
Confirmation of a diagnosis of HL requires the presence of multinucleated, polypoid Reed-Sternberg cells in the malignant tissue. HL presents in two forms: nodular lymphocyte predominant and the more classic form that includes nodular sclerosis, mixed cellular, lymphocyterich, and lymphocyte-depleted subtypes. A complete diagnostic work up is key to proper disease staging. Treatment is usually radiation therapy and/or combination chemotherapy. Outcomes of HL are particularly good with 5-year survival rates exceeding 90% for stages I and II and 80–90% for stages III and IV disease.
NHL vary from indolent to aggressive types. While slowly progressive and relatively responsive to chemotherapy, indolent tumors tend to wax and wane, repetitively relapse, and usually lead to eventual death. Aggressive lymphomas are highly proliferative and can be rapidly fatal, however, with new therapies, an increasing proportion of these malignancies are curable. Classification of NHL depends upon cluster differentiation antigen expression on the tumor cell surface; cytogenetic findings also add diagnostic and prognostic information. The International Prognostic Index provides distinct clinical and prognostic categories based on five demographic and clinical characteristics (age, performance status, serum lactate dehydrogenase, number of extranodal sites, and Ann Arbor stage). Therapeutic approaches for this disease are based on the specific lymphoma subtype, the stage of disease, the physiologic status of the patient, and the prognosis. While chemotherapy and/or radiotherapy are curative in some patients, many with primary or relapsed disease remain refractory to conventional treatments. For some subtypes, extended remissions have been achieved using either newly developed monoclonal antibodies directed against lymphoma cells (rituximab) or high-dose chemotherapy regimens paired with stem cell transplantation. Survival varies considerably by specific subtype; however, the overall 5-year survival rate for this malignancy now approaches 66%.
Lymphoma Pathogenesis
Lymphocytes arise from hematopoietic stem cells and undergo differentiation to a specific phenotype. These cells along with secondary lymphoid organs (lymph nodes, spleen, gastrointestinal and respiratory lymphoid tissues) are responsible for the immunologic response that protects against invasion by infectious and other foreign antigens. Immune regulation depends on a continuum of lymphoid cell growth, cell signaling, programmed cell death, and/or immune eradication. An imbalance in this complex system may initiate molecular processes that drive the malignant transformation of lymphocytes and promote proliferation of neoplastic cells; however, these processes are not well-understood. Normal T and B cell differentiation requires intricate B cell immunoglobulin and T cell receptor gene rearrangements, which are subject to spontaneous error. Chromosomal translocations are detected in up to 90% of lymphoid malignancies. Oncogenic viruses and environmental carcinogens may also independently generate genetic lesions. At a molecular level, these chromosomal translocations, deletions, and/or mutations may alter cell recognition, precipitate oncogene activation, and suppress repair mechanisms, thereby allowing clonal expansion of malignant T or B cells.
An emerging paradigm related to lymphomagenesis is that chronic antigenic stimulation, that is, a persistent inflammatory process, leads to increased B cell proliferation, thereby increasing the probability of random genetic errors. This theory is supported by the fact that increased risk of lymphoma has been clearly established in immunocompromised populations vulnerable to infection and, more recently, in those with specific chronic infections and autoimmune conditions. Common to such individuals is a persistent state of foreign or autoantigenic stimulation leading to a chronic inflammatory response involving a cascade of cellular and cytokine reactions that may provoke tissue injury, compensatory immunosuppression, and eventual tumor initiation. If the responsible antigen is infectious in nature, the pathogen itself may have the potential to infect a normal cell, integrate viral DNA into the host genome, and transform the cell into one that is malignant and self-replicating. Other environmental factors that independently lead to immunosuppression may act as cofactors in lymphomagenesis by further inhibiting the recognition and eradication of a malignant cell.
Etiology Of Lymphoma
Familial And Hereditary
Oncogenes, tumor suppressor genes, and DNA repair genes have been shown to play an important role in carcinogenesis. While most genetic lesions that have been linked to cancers represent somatic mutations, inherited (germ line) genetic susceptibility to lymphoma is conceivable. Aggregation of lymphoma in families, while unusual, has been observed, suggesting a role of either heredity or shared environmental exposures in the etiology of lymphoma. Up to sevenfold increases in risk of lymphoma among individuals having a close relative with lymphoma or other lymphoproliferative diseases have been observed. Of note, Mack and colleagues (1995) reported a 99-fold increase in risk of HL among those having a monozygotic twin with HL. These associations, however, may merely reflect early identification of new cases in families with an increased awareness of lymphoma symptoms or may suggest shared environmental exposures among family members. While the role of polymorphisms in genes specifically responsible for immune regulation and function, such as apoptosis, DNA repair, and tumor necrosis factor, have been investigated, no clear association between any of these genetic mutations and lymphoma risk has been identified. In general, familial lymphomas account for less than 5% of all cases; thus, the risk of lymphoma attributable to hereditary factors is likely to be low.
Immune Dysregulation
An important role of the immune system in the occurrence of lymphoma has been well-established. Risk of lymphoma is clearly increased in conditions of immune dysregulation, be it primary immunodeficiency, iatrogenic immunosuppression, autoimmune disease, or acquired immunodeficiency. Persistent immunologic stimulation and cytokine production, reactivation of Epstein-Barr virus (EBV) infection, and gene rearrangements appear to be sequelae that most often herald lymphomagenesis.
Primary Immunodeficiency
Among individuals with primary immunodeficiency, the risk of lymphoma ranges from 10–25%. These conditions are characterized by genetic defects that interfere with DNA repair and cell-mediated immunity. Specifically, hereditary immunodeficiencies such as Wiskott-Aldrich syndrome and ataxia telangiectasia are accompanied by a 10–15% absolute risk of diffuse large B-cell lymphoma. Since the T cell response is so important in controlling EBV infection, it is not surprising that many of these tumors are EBV-associated. These neoplasms are aggressive, primarily extranodal, and frequently involve the central nervous system.
Iatrogenic Immunosuppression
Individuals with secondary immunosuppression, most often drug-induced to prevent organ rejection in transplant recipients, experience dramatic increases in lymphoma risk. Posttransplant lymphoproliferative disease (PTLD) is characterized by polyclonal and monoclonal lesions derived from mutated B cells. The magnitude of risk of PTLD varies depending on the degree, duration, and type of immunosuppression. Opelz and Dohler (2004) conducted a large international study of 195 938 patients who received a solid organ transplant. These investigators found that the relative risk of lymphoma among organ transplant recipients at 5 years compared to the normal population was 239.5 for heart–lung recipients, 58.6 for lung recipients, 34.9 for pancreas, 29.9 for liver, 27.6 for heart, and 12.6 for cadaveric kidney. Chronic antigenic stimulation from the allograft on a backdrop of drug induced immunosuppression is the likely mechanism for these lymphoid malignancies. As with primary immunodeficiency, the hallmark of these lymphomas is high-grade, often EBV-positive tumors with a proclivity for extranodal sites, especially the brain. While this condition often develops within the first year after an allograft, when immunosuppression is usually severe, time to lymphoma development had no impact on patient survival. Historically, outcomes with PTLD have been poor, with 1-year mortality approaching 50%. Recent efforts to reduce immunosuppressive drugs and treat with rituximab have led to a 64% response rate in PTLD.
Autoimmune Conditions
It has been difficult to delineate the deleterious effects of immunosuppression alone from the impact of persistent inflammation in the development of lymphoma among individuals having autoimmune conditions that often require treatment with immunosuppressive agents. For example, rheumatoid arthritis, systemic lupus erythematosis, Sjogren’s syndrome, and celiac disease all carry an increased risk of both HL and NHL. Patients with the latter two diseases are generally not treated with immunosuppressants, so their risk of lymphoma can be attributed to the underlying autoimmune disease. On the other hand, patients with rheumatoid arthritis and systemic lupus erythematosis frequently receive immunosuppressive therapy for extended periods of time. The increased risk of lymphoma seen in this population may therefore be partly incurred from the disease itself and partly from its treatment. Askling and colleagues (2005) designed a study to assess the risk of steroid immunosuppression and specifically address this problem of etiologic differentiation by including a population of individuals with either giant cell arteritis or polymyalgia rheumatica. Both conditions are treated with corticosteroids early in their courses rather than after a protracted pattern of chronic inflammation. The investigators found that with one to three years of moderate to high-dose steroids, there was no increased risk of lymphoma in this population. Instead, they found a statistically significant reduction in the rate of lymphomas. While these findings cannot be extrapolated to other immunosuppressive agents whose mechanism of action is different from that of corticosteroids, this study suggests that inflammation may have a greater role in lymphomagenesis than treatment with some immunosuppressive agents.
Acquired Immunodeficiency
NHL is one of the most common malignancies associated with human immunodeficiency virus (HIV) infection, and rates of HL are also elevated among those infected with HIV. As early as 1985, NHL was recognized as an AIDS-defining illness when approximately 4% of all AIDS cases first presented with lymphoma. Although HIV is not considered to be an oncogenic virus, it contributes to lymphomagenesis by impairment of cell-mediated immunity and increased opportunity for virally induced cell proliferation, leading to an accumulation of genetic lesions. About 50% of HIV-associated lymphomas are EBV-positive. Burkitt lymphoma and centroblastic lymphoma are associated with EBV in 30% and 40% of HIV-positive cases, respectively, unrelated to the severity of immunodeficiency. In contrast, immunoblastic lymphoma, primary central nervous system lymphoma, and primary effusion lymphoma are almost always EBV-associated and usually occur only in strongly immunosuppressed AIDS patients. This variability suggests other factors must also be involved in the etiology of AIDS-related lymphomas. Although incidence of NHL in HIV-positive individuals has decreased since the mid-1990s, NHL still accounts for about 20% of all AIDS-related deaths in countries having broad access to HAART. The findings by Biggar and colleagues (2006) that show an increasing excess of HL among persons with AIDS are perplexing. These investigators speculate that in severely immunosuppressed individuals with AIDS, Reed-Sternberg cells are incapable of producing the cytokines required to perpetuate survival; however, in the presence of the immune-modulating effects of antiretroviral therapy, these malignant cells are able to establish a microenvironment that facilitates their own proliferation and expansion, with the ultimate development of HL.
Infectious Agents
The number of viruses and bacteria that have been associated with lymphoma is steadily increasing (Table 1).
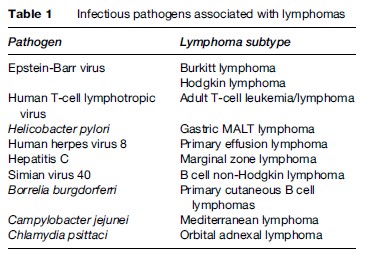
These infections increase the risk of lymphoma through numerous mechanisms, including immunosuppression, direct oncogenic mutation of cellular DNA, and chronic antigenic stimulation. Each infectious agent is briefly discussed below.
Epstein-Barr Virus
Epstein-Barr virus is a ubiquitous virus that persistently infects more than 90% of adults in developed countries and essentially all individuals living in developing countries. Although primary infection is usually subclinical in nature, the virus remains latent in memory B cells. EBV is associated with infectious mononucleosis, and viral DNA and proteins are found in lymphoma cells. EBV has been shown to be capable of B-cell activation, which could lead to a genetic mutation occurring in a virally infected B lymphocyte. Many lymphomas arising in the setting of immunosuppression are EBV-associated, including those found in recipients of organ transplantation and those associated with HIV. These most likely represent reactivation of latent EBV infection. EBV is also associated with approximately 30–40% of Hodgkin lymphomas, most aggressive natural killer (NK) cell lymphomas and leukemias, a subset of peripheral T cell lymphomas, and virtually all Burkitt lymphomas arising in malarial areas.
In developed countries, approximately 40% of HL are EBV-positive. The role of delayed EBV infection, characterized by development of infectious mononucleosis in adolescence, has been examined but not confirmed as a risk factor for HD. Risk has been estimated to be 2.5 and lasts up to 20 years after initial infection, suggesting a link with EBV or confounding due to socioeconomic class and late exposure to infections or to hyperreactivity resulting from antigenic stimuli.
The onset of endemic Burkitt lymphoma is characterized by high EBV antibody titers. The relative restriction of endemic Burkitt lymphoma to the wet, temperate lowlands of Africa and New Guinea suggests an etiologic significance of the convergence of two pathogens: Plasmodium falciparum in endemic malarial infestation regions, and EBV reactivation among malarial-infected children. Only about 15–25% of Burkitt lymphoma cases in nonendemic areas are associated with EBV.
Although EBV is endemic throughout the world, only a small percentage of carriers will develop lymphoma. Clearly EBV-associated lymphomagenesis is a multifactorial process, which is only partially understood. The role of the virus in the pathogenesis of a diverse subset of lymphomas is indicative of its potential to behave differently under circumstances of immunosuppression, coinfection, and other host and environmental factors.
Human T-Cell Lymphotropic Virus 1
In 1978, human T-cell lymphotropic virus 1 (HTLV-1) was identified as the etiologic agent of adult T-cell leukemia/lymphoma (ATLL). This retrovirus produces slow, progressive infection, is transmitted through blood and breast milk, and is known to precipitate immunosuppression. HTLV-1 is endemic in Japan, the Caribbean, and parts of central Africa; carriers have a cumulative lifetime risk of ATLL of 1–5%. In endemic regions, ATLL accounts for 50% of all lymphoid malignancies. Exposure usually occurs during infancy, but due to its long latency period the median age of development of ATLL is 55 years. The leukemogenic potential of the virus is thought to arise from the infected cells’ expression of viral oncoproteins, which promotes genetic mutation and clonal proliferation. Public health strategies such as blood donor screening, protective sexual practices, and accessibility of nutritious alternatives to breast-feeding are primary prevention measures that may limit HTLV-1 transmission in countries of high viral prevalence.
Helicobacter Pylori
Helicobacter pylori (HP), a gastric pathogen, has been shown to play a pivotal role in extranodal gastric lymphoma, particularly mucous-associated lymphoid tissue (MALT) types, of which the majority are HP-positive. This association is now well-established based upon the presence of HP infection in primary gastric lymphoma, confirmation of the importance of HP in the pathogenesis of gastric lymphoma by in vitro studies, and demonstration of complete remission of the lymphoma following antibiotic eradication of HP. Chronic antigenic stimulation and inflammation due to the pathogen may represent the mechanism of lymphomagenesis in these tumors.
Human Herpes Virus 8
Some rare infectious pathogens have been linked to the development of lymphoma. Human herpes virus 8 (HHV8), primarily associated with Kaposi sarcoma, has been detected in most subjects with primary effusion lymphoma, a body-cavity-based lymphoma seen almost exclusively in HIV-positive patients. Cases often present with dual EBV and HHV8 infection; therefore, delineation of the etiologic role of each virus is difficult. These neoplasms have been demonstrated to be monoclonal expansions of a single infected cell, suggesting that the viral infection precedes tumor growth.
Hepatitis C
Approximately 180 million people, or 3% of the world population, are infected with hepatitis C virus (HCV). Although not known to be oncogenic, HCV is lymphotropic and replicates in peripheral blood mononuclear cells. In Italy, reports have suggested that up to 32% of NHL cases are HCV-positive, compared to only 1.3% of normal controls. Japanese studies have reported similar findings. In the United States, however, where HCV prevalence is less than 2%, a population-based study demonstrated a relative risk of NHL of only 2.0 with HCV positivity. Studies from Canada and several other countries have been negative. While there may be a role of HCV in NHL, this virus may only be relevant in geographic areas with the highest prevalence of infection. While the exact mechanism of lymphomagenesis is unclear, the increased risk may be due to chronic antigenic stimulation.
Simian Virus 40
In the past decade there has been considerable controversy regarding the potential role of simian virus 40 (SV40), a polyomavirus indigenous to African green monkeys, in lymphomagenesis. Confirmed as a viable contaminant of the Salk polio vaccine, SV40 has demonstrated oncogenic potential in animals and may be transmissible from person to person and from mother to infant during childbirth. In 2002, reports by two investigative teams, Vilchez et al. and Shivapurkar et al., that demonstrated detection of SV40 in 40% of NHL specimens drew significant attention to this virus as an etiologic factor in lymphoma. While additional studies have provided evidence of an association between SV40 and lymphoma, other investigations from Spain, Australia, and Germany have failed to detect SV40 DNA in any lymphoma specimen. Dissemination of the virus via contaminated vaccine in these countries has not been confirmed. Given the high prevalence of SV40 detected in lymphoma specimens in early reports, further research in this area is warranted.
Other Pathogens
A plethora of data has recently emerged linking lymphoma risk to various other infections. Recent studies suggest that Chlamydia psittaci (CP) may be associated with ocular lymphomas of the orbital adnexal type. CP is an obligate intracellular bacterium that causes psittacosis, a human lung infection associated with exposure to infected birds, cats, and other pets. Ferreri and colleagues (2004) demonstrated CP DNA in 80% of tumor biopsies from 40 Italian patients with ocular lymphomas. Of those positive, 66% were marginal zone lymphomas. Other studies have not consistently supported this finding. Genetic and phenotypic variations in CP strains present in Europe and southeastern United States may account for some of these differences.
Recently, infection with Borrelia burgdorferri has been linked to primary cutaneous B cell lymphoma. The majority of these observations have come from European countries, with little evidence of such an association in North America.
Mediterranean lymphoma is an unusual form of lymphoma that arises in small-intestinal-mucosa-associated lymphoid tissue. Early-stage disease regresses with antibiotic treatment, suggesting a bacterial etiology. The bacteria Campylobacter jejunei has been identified in these tumors. Although research has been quite limited due to the unusual nature of these lymphomas, these observations raise the possibility of a role for other, yet to be recognized, pathogens in lymphomagenesis.
Other Environmental Exposures
Numerous other environmental exposures have been studied related to lymphoma; however, results have been somewhat inconsistent and at times contradictory. Many of these studies have been limited by inadequate sample size, poor methodologic designs, and difficulties in measuring exposure.
Ultraviolet Radiation
The impact of exposure to ultraviolet radiation (UVR) on the risk of developing lymphoma remains controversial. Increasing recreational time, changing fashions leading to more skin exposure, and the cosmetic desirability of tanning have contributed to increasing UVR exposure in recent years, and the increasing incidence of NHL parallels the escalating incidence of skin cancer. NHL and skin cancer occur more frequently than expected in the same individuals, and some studies suggest that sun sensitivity is related to an increased risk of NHL. Such disease pairing may provide etiologic clues to disease causation. In humans, sunlight exposure in susceptible individuals produces acute UV injury, resulting in both inflammatory and immunomodulatory responses. Evidence suggests that it is the absorption of UVR by these cells and the resulting DNA damage that trigger the biochemical cascade of immunosuppression, and may alter the balance of the host–disease relationship in favor of pathogens. Some studies have implicated UVR in risk of lymphoma, but data remain inconclusive. A moderate international geographic correlation of UVR levels and NHL incidence among Caucasians has been reported. Similarly, findings of a higher risk of NHL among farmers may be attributed to the increased UVR exposure that accompanies their outdoor activities. On the other hand, Smedby and colleagues (2005) conducted a large, population-based study of 3740 patients and 3187 controls in Sweden and Denmark that yielded opposing results. The study found that higher amounts of UVR exposure were associated with decreased lymphoma risk, contrary to what was previously indicated. Protective effects of vitamin D are a possible explanation that would support an inverse association between UVR and lymphoma risk. Given the ubiquitous nature of UVR, this exposure warrants careful consideration as an etiologic factor in lymphoma. The conflicting results of published studies suggest that further investigation is, indeed, indicated.
Chemical/Agricultural Exposure
Given the excess mortality from cancer observed in rural areas, particularly those in which farming is common, and the concurrent rise in the use of pesticides, agriculture related environmental exposures have been ambitiously investigated. These studies are challenging to conduct because of the difficulty in developing high-quality assessments of exposure. While many studies have demonstrated a high rate of lymphoma among agricultural workers, few provide information on the specific agricultural exposures that might be involved, such as individual pesticides, animal pathogens, or even UVR exposure.
Some specific herbicides and pesticides have been linked to an increased risk of lymphoma. Phenoxy herbicides, which are widely utilized both in agriculture and by the general population, have most frequently been associated with higher risk of lymphoma. One of particular interest has been Agent Orange, a phenoxy herbicide formulation used as a defoliant by U.S. forces in Vietnam. Some but not all studies have reported an increased incidence of lymphoma among veterans exposed to this agent. The herbicide 2,4-dichlorophenoxyacetic acid (2,4-D) has been associated with excess risk of lymphoma; risk estimates of 3–8 times normal have been associated with the heaviest exposure levels. Additional studies have suggested some increased risk of lymphoma among persons exposed to organochlorine chemicals such as polychlorinated biphenyls, or PCBs. Although the data for occupational exposures are not entirely consistent, there is evidence that some links may exist between the development of lymphoproliferative diseases and environmental or work-related toxins. Chemical exposures have been shown to increase genetic mutations and alter cellmediated immunity. Occupations that include tobacco, leather, construction, automotive, and health-care workers have been studied, but results are inconsistent. Additional large, population-based studies are needed in order to improve our current understanding of this problem.
Hair Dyes
Hair dyes contain compounds, such as aromatic amines, that are known to be mutagenic and carcinogenic in animals. Excess hematologic malignancies have been reported in both hairdressers and men and women whose hair is dyed. It appears that darker permanent dyes pose the highest risk, but there is some evidence that this risk has greatly diminished or been eliminated since 1982, when oxidative dye products were reformulated in the United States and Europe. A recent international European study of 2302 lymphoma patients and 2417 controls examined patterns of hair dye use among men and women. This study found that 38% of study subjects reported previous use of a hair dye product, and a history of having ever used hair dye was associated with a 19% increased risk of lymphoma. The odds ratio in this study was markedly higher for those using hair dyes exclusively prior to 1980 compared with those who started dyeing their hair after that year (1.37). Although the increased risk apparently posed by hair dyes is comparatively small, the potential impact of this exposure is magnified by the prevalence of hair dye use. For this reason, the use of products currently available merits closer examination.
Tobacco And Alcohol
Tobacco has been shown to alter the immune response and contains substances known to be leukemogenic; however, minimal support for an association of HL and NHL with tobacco exists. Most studies have found no association with smoking amount or duration.
Studies regarding alcohol have been inconsistent, but several have suggested a protective effect of alcohol related to HL and NHL, implicating a cellular and humoral immune response benefit. This reduced risk appears to be independent of specific type of alcohol consumed, duration of alcohol use, and lifetime consumption.
Blood Transfusions
Several studies have demonstrated an association between history of blood transfusion and lymphoma. In patients who are diagnosed with low-grade lymphomas within months or a few years following transfusion, it is often impossible to know if the lymphoma preceded the transfusion or if the reverse is true. Potential biologic mechanisms that may have an etiologic impact include transmission of an oncogenic virus, transfusion-induced immunosuppression, and engraftment of malignant lymphoma cells from the donor. A population-based study of women in Iowa found a twofold or greater risk of lymphoma among persons receiving blood transfusions. Additional cohort studies have likewise shown a significant increase in risk of NHL in patients with a history of blood transfusion.
Diet
The Westernized diet has changed substantially over the past decades with the inclusion of more processed and refined foods. Diet has been shown as a source of mutagenic and chemopreventive agents; therefore, dietary factors may account for some of the increase in lymphoma incidence that has occurred over the past several decades. The risk of NHL has been linked to increased consumption of animal protein and saturated and animal fats. Animal products may generate chronic antigenic stimulation and/or immune unresponsiveness, or confounding by dietary absorption of pesticides and herbicides may account for the association. The roles of specific types of fats and their effects on immune function remain poorly understood. Some studies have attributed increased lymphoma risk to consumption of dairy products and eggs as well.
Higher intake of fruits, cruciferous vegetables, green leafy vegetables, and vegetables high in carotenoids have been demonstrated to have an inverse association with NHL. The relationship between fruits and vegetables and risk of NHL may be due to the antioxidants and inhibitors of nitrosation found in some foods. Fish consumption has also been associated with a decreased risk of lymphoma.
Drugs
As early as 1966, systemic ‘pseudolymphoma’ syndromes were linked to the use of anticonvulsants. These syndromes are often clinically indistinguishable from lymphoma, and they usually regress when the offending agent is withdrawn. Other drugs, such as calcium channel blockers, ACE inhibitors, statins, H2 blockers, and SSRIs, can produce cutaneous hypersensitivity reactions, which often appear to overlap histologically with cutaneous B or T cell lymphomas and occasionally progress to NHL. Factors related to the evolution of these lymphomas remain largely unknown. No consistent associations of NHL with long-term use of non-steroidal anti-inflammatory drugs, aspirin, or COX- 2 inhibitors have been observed.
Reproductive
While hormones have immunomodulatory effects, there is no convincing evidence of any influence of hormones or reproductive factors on HL or NHL. A small increase in lymphoma risk has been reported during pregnancy, but the immune dysregulation of pregnancy has been repeatedly suggested to increase the mother’s vulnerability to cancer and other diseases.
Anthropometric Parameters
While physical activity is thought to influence immune function, there are little data to suggest that there is a relation with lymphoma. Reported risk estimates of 1.6 and 1.4 for males and females, respectively, with a body mass index of greater than or equal to 30 appear in the literature. Studies have indicated that obesity can lead to impaired immune function, which can be restored if calories are restricted and physical activity is increased. Obesity may also affect the metabolism of endogenous hormones, which may interfere with cell proliferation, differentiation, and apoptosis. Taller height, also associated with availability of food and energy and greater exposure to growth-related hormones, has also been suggested as a marker of increased HL risk.
Summary
A significant step in lymphoma research has been the gradual realization that the lymphomas comprise a diverse set of diseases, which vary not only in pathology and clinical course but most likely in etiology. The improved treatment and prevention of these hematologic malignancies depend on our understanding of the etiology and pathogenesis of these diseases. The rapid increase in the occurrence of NHL between 1975 and 1995 suggests that lymphomagenesis may be influenced by environmental factors. The identification of environmental–genetic interactions that may predispose patients to develop lymphoma is an important component to the delineation of disease causation.
Although we have seen that there is an abundance of epidemiologic data in lymphoma, many questions remain unanswered. While many of these factors have been discussed, it is not certain which factor(s) may serve as an initiator of malignancy and which promote the survival of a cancer cell, perhaps at times merely by ignoring its existence. We must build on our current knowledge regarding the etiology of NHL and the mechanisms related to its progression. As knowledge is gained in these two arenas, prevention, treatment, and eventual cure will be realized. Potential strategies that may be useful include: administration of vaccines and medications (antibiotics or antivirals) to prevent or treat viral infections that are eventually demonstrated to be associated with lymphoma; development of immunotherapeutic treatments that will treat existing tumors whose growth may be dependent on viral antigenicity, or will enhance the immune response against the tumor; development of therapies that interfere with tumor survival such as antiangiogenesis drugs and biologics that interrupt critical growth-signaling pathways in the tumor; novel approaches to enhance immune function such as vitamins and nutrients that will improve immune surveillance during episodic exposure to carcinogens or during anticipated immunosuppression such as during medical procedures or high-stress events; implementation of protective practices for hazardous and mutagenic substance use, such as protective clothing, air management systems, and so forth; and development of new agricultural, industrial, and home products that are effective while carcinogen-free.
Bibliography:
- Askling J, Klareskog L, Hjalgrim H, Baecklund E, Bjo¨ rkholm M, and Ekbom A (2005) Do steroids increase lymphoma risk? A case-control study of lymphoma risk in polymyalgia rheumatica/giant cell arteritis. Annals of the Rheumatic Diseases 64(12): 1765–1768.
- Biggar RJ, Jaffe ES, Goedert JJ, Chaturvedi A, Pfeiffer R, and Engels EA for the HIV/AIDS Cancer Match Study (2006) Hodgkin lymphoma and immunodeficiency in persons with HIV/AIDS. Blood 108: 3786–3791.
- Ferreri AJ, Guidoboni M, Ponzoni M, et al. (2004) Evidence for an association between Chlamydia psittaci and ocular adnexal lymphomas. Journal of the National Cancer Institute 96(8): 586–594.
- Jaffe ES, Harris NL, Stein H, and Vardiman JW (2001) World Health Organization Classification of Tumours: Tumours of the Haematopoietic and Lymphoid Tissues. Lyon, France: International Agency for Research on Cancer.
- Mack TM, Cozen W, Shibata DK, et al. (1995) Concordance for Hodgkin’s disease in identical twins suggesting genetic susceptibility to the young-adult form of the disease. New England Journal of Medicine 332: 413–418.
- Opelz G and Dohler B (2004) Lymphomas after solid organ transplantation: A collaborative transplant study report. American Journal of Transplantation 4(2): 222–230.
- Shivapurkar N, Harad K, Reddy J, et al. (2002) Presence of simian virus 40 DNA sequences in human lymphomas. Lancet 359(9309): 851–852.
- Smedby KE, Hjalgrim H, Melbye M, et al. (2005) Ultraviolet radiation exposure and risk of malignant lymphomas. Journal of the National Cancer Institute 97(3): 199–209.
- Vilchez RA, Madden CR, Kozinetz CA, et al. (2002) Association between simian virus 40 and non-Hodgkin lymphoma. Lancet 359(9309): 817–823.
- Carbone A and Gloghini A (2005) AIDS-related lymphomas: From pathogenesis to pathology. British Journal of Haematology 130(5): 662–670.
- Chiu BC, Cerhan JR, Folsom AR, et al. (1996) Diet and risk of nonHodgkin lymphoma in older women. Journal of the American Medical Association 275(17): 1315–1321.
- Cross AJ and Lim U (2006) The role of dietary factors in the epidemiology of non-Hodgkin’s lymphoma. Leukemia and Lymphoma 47(12): 2477–2487.
- Ekstro¨ m-Smedby K (2006) Epidemiology and etiology of non-Hodgkin lymphoma: A review. Acta Oncologica 45: 258–271.
- Engels EA, Pfeiffer RM, Goedert JJ, et al. for the HIV/AIDS Cancer Match Study (2006) Trends in cancer risk among people with AIDS in the United States 1980–2002. AIDS 20: 1645–1654.
- Fisher SG and Fisher RI (2004) The epidemiology of non-Hodgkin’s lymphoma. Oncogene 23: 6524–6534.
- Fisher SG and Fisher RI (2006) The emerging concept of antigen-driven lymphomas: Epidemiology and treatment implications. Current Opinion in Oncology 18: 417–424.
- Kripke ML (1994) Ultraviolet radiation and immunology: Something new under the sun; Presidential address. Cancer Research 54(23): 6102–6105.
- Mu¨ ller AMS, Ihorst G, Mertelsmann R, and Engelhardt M (2005) Epidemiology of non-Hodgkin’s lymphoma (NHL): Trends, geographic distribution, and etiology. American Journal of Hematology 84: 1–12.
- Sandin S, Hjalgrim H, Glimelius B, Rostgaard K, Pukkala E, and Askling J (2006) Incidence of non-Hodgkin’s lymphoma in Sweden, Denmark, and Finland from 1960 through 2003: An epidemic that was. Cancer Epidemiology Biomarkers and Prevention 15(7): 1295–1300.
- Thomas RK, Re D, Zander T, Wold J, and Diehl V (2002) Epidemiology and etiology of Hodgkin’s lymphoma. European Society for Medical Oncology 13(supplement 4): 147–152.
- http://www-dep.iarc.fr/globocan/database.htm – GLOBOCAN 2002 Database. Descriptive data regarding cancer worldwide, provided by the Descriptive Epidemiology Group of the International Agency for Research on Cancer.
- htttp://www.leukemia-lymphoma.org/ – The Leukemia & Lymphoma Society. This is the world’s largest voluntary health organization dedicated to funding blood cancer research, education, and patient services. The Society’s mission is to cure leukemia, lymphoma, Hodgkin disease, and myeloma, and improve the quality of life of patients and their families. Since its founding in 1949, the Society has invested more than $550.8 million for research specifically targeting blood cancers.
- http://www.lymphoma.org/ – Lymphoma Research Foundation. A nonprofit organization in the United States that provides lymphoma information for patients and maintains an active research funding program in lymphoma.
- http://seer.cancer.gov/ – National Cancer Institute Surveillance, Epidemiology and End Results Program. Source for cancer statistics from the United States.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.






