This sample Respiratory Diseases Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Introduction
The lungs are one of the organs essential to life, for we depend on them to extract oxygen from the air we breathe. Despite this, and the fact that respiratory diseases are common, the general public is often poorly educated as to the true extent of pulmonary morbidity and mortality.
In developed countries, in spite of all our advanced modalities of care, respiratory diseases make up one of the four major causes of mortality and morbidity and their consequent economic costs. In the developing world, respiratory infectious diseases, compounded by the arrival of HIV, are still major killers of young and old alike.
The care of patients with respiratory problems frequently occurs in the primary care setting, where it may constitute up to 25% of the caseload. Within hospitals, generalist physicians treat many patients with pneumonias and other acute infections. Increasingly, specialist ‘respiratory physicians’ are taking on more of this care in developed countries, given the trend toward specialization. Practice varies from country to country, for example, in regard to respiratory intensive care, which may be undertaken by respiratory physicians, intensive care specialists, or anesthesiologists.
The origin of respiratory medicine as a clinical discipline derives from the care of patients with tuberculosis (TB), a scourge that continues to afflict the human race. Another strong influence arose from the understanding of pulmonary gas exchange and mechanics developed in physiology laboratories. Epidemiology has contributed knowledge of the respiratory effects of air pollution, from both tobacco smoke and atmospheric pollution. From these beginnings, and with the enormous explosion of medical knowledge in the last 30 years, respiratory medicine has expanded and now includes care for a range of diseases with multiple causes from allergies to zoonoses.
The Burden Of Lung Disease
A number of important national and international publications in recent years have brought together information on lung disease to focus attention on the consequent morbidity, mortality, and economic costs, and to highlight areas in need of research and health-care investment (British Thoracic Society, 2001; European Respiratory Society/European Lung Foundation, 2003).
The authors of the European Lung White Book (2003) highlight the forecast that in 2020, of 68.3 million deaths worldwide, 11.9 million will be caused by lung diseases. This contrasts with WHO data for 1990, in which 9.4 million deaths occurred due to lung diseases. The increase in respiratory deaths will be largely accounted for by chronic obstructive pulmonary disease (COPD), TB, and lung cancer, disorders that should be preventable with active public health interventions.
In Europe, respiratory diseases rank second to cardiovascular diseases in terms of incidence, prevalence, mortality, and economic costs. Pneumonia, COPD, and lung cancer are the big three respiratory killers in Western and Eastern Europe. Across the individual countries, there is considerable variation in age-standardized death rates from respiratory diseases, from a high in Kyrgyzstan (165 per 100 000) to a low in Austria (30 per 100 000), with a European average of 65 per 100 000 population. Of the European Union countries, Ireland (120 per 100 000) and the UK (105 per 100 000) have death rates considerably in excess of the EU average (57 per 100 000) and of figures in many Eastern European countries. Why these discrepancies exist is not yet clearly understood.
The annual economic burden of respiratory diseases in Europe is estimated to be €102 billion at year 2000 prices. This includes lost working days (€48.3b); mortality, rehabilitation, and education (€20.0b); inpatient hospital care (€17.8b); outpatient/ambulatory care (€9.1b); and prescription drugs (€6.7b). When analyzed by diagnostic category, COPD alone was estimated to cost €38.7 billion.
Tobacco: Public Enemy Number One
Tobacco smoking is directly responsible for the morbidity and mortality resulting from two of the major killer respiratory diseases, lung cancer and COPD. However, we must not lose sight of the fact that these are only part of the total sum of damage due to tobacco.
Data accessible on the WHO website (see the section ‘Relevant websites’) reveals that total annual deaths due to tobacco worldwide will continue to rise over the next 30 years. In industrialized countries, deaths will rise from 2.1 million in 2000 to 3 million in the year 2020, but the rise in developing countries will be more dramatic, from a similar baseline of 2.1 million deaths in 2000 to a projected 7 million by 2030. This may in part reflect that tobacco continues to be promoted in the developing world just as industrialized countries are at last starting to implement vigorous antismoking legislation in many public places. Major reductions in respiratory deaths could be expected from reduction in smoking rates at all ages.
Respiratory Diseases Unrelated To Tobacco
Respiratory diseases unrelated to tobacco exhibit considerable geographical variation in national prevalence rates even within Europe, which is taken as an illustrative example, using the European Lung White Book data. Worldwide, the variations and disease mix may be even more widely divergent. Of necessity, each will be discussed here briefly.
Asthma
This common lifelong airways disease affects both adults and children worldwide. There are major variations in prevalence, and in Europe, figures for adult prevalence vary from 0.28% in Georgia to 10–13% in the UK. A further concern is that asthma prevalence has doubled in Western Europe in the last 10 years. The prevalence in teenage children is particularly high, up to 21%, which bodes ill for the future. Mortality rates due to asthma range from 0.54 per 100 000 in the Netherlands to 8.7 per 100 000 in Portugal, suggesting variations in standards of care. Strategies are needed to deal with both causes and best management of asthma, especially since it affects many young people.
Cystic Fibrosis
This disorder is important, as it is the most common, lethal inherited disease of Caucasian races. National disease registries exist in North America and a number of European countries. Lung disease is one of the major causes of morbidity and mortality in patients with cystic fibrosis. The cost of care for those with advanced disease is considerable and in Europe exceeds €29 000 per annum. Care is often centered in tertiary centers because of the sophisticated level of care needed for relatively small numbers of mainly children and young adults.
Interstitial Lung Diseases
Idiopathic pulmonary fibrosis and connective tissue-related lung disease are probably the most important in this group of disorders, based on their prevalence and significant morbidity and mortality. The category as a whole covers approximately 200 disorders, many extremely rare, that have been classed as orphan diseases. (A useful contact for the latter is the register and study group centered in France– Group d’Etudes et de Recherche sur les Maladies ‘Orphelines’ Pulmonaires; see the section ‘Relevant websites.’)
Idiopathic pulmonary fibrosis data relating to incidence and prevalence are difficult to obtain, partly because of problems of nomenclature. The European Lung White Book quotes prevalence figures from a low of 3–6 per 100 000 in the UK to a high of 16–18 per 100 000 in Finland.
While corticosteroids were used for many years as the treatment of first choice for idiopathic pulmonary fibrosis, results were often unsatisfactory. Bouros and Antoniou (2005) have recently reviewed current and future prospects for treatment.
A significant subgroup of interstitial lung disease may relate to organic or inorganic dust exposure, so a careful occupational history is essential when assessing such cases. Another important subgroup is made up of iatrogenic pulmonary disorders, especially those related to the use of chemotherapeutic agents and radiation therapy in cancer treatment.
Occupational Lung Diseases
There is a major information deficit regarding the true incidence and prevalence of occupational lung diseases. This is because the occupational component may go unnoticed and due to the poorly developed state of official reporting systems in many countries. The range of manifestation is wide and includes acute inhalation injuries, occupational infections, asthma, chronic obstructive pulmonary disease (COPD), interstitial lung diseases, lung cancer, and pleural disease, including mesothelioma.
Mesothelioma is of particular concern in industrialized countries in which asbestos was widely used from World War II until the 1970s. Given the approximately 30-year latency between exposure and mesothelioma development, it is expected that mesothelioma deaths will continue to rise until 2020. In Europe alone, it is estimated that mesothelioma will kill about 250 000 people between 1995 and 2029.
Asthma is now considered to be the most common occupational respiratory disease in modern societies and accounts for 5–15% of asthma in young adults. A careful and complete occupational history should be included in the assessment of all adult asthmatic patients.
In the absence of publication of national statistics for occupational lung diseases, it is difficult to make international comparisons. Some voluntary reporting registries exist and can provide useful insights, for example, the SWORD project coordinated by the Health and Occupational Network (THOR) in the UK.
Pneumonia
The respiratory tract is the most common site for bacterial infections, of which the pneumonias are of the most clinical importance. The incidence of pneumonia is highest at the extremes of age, and most deaths occur in the elderly. Although common worldwide, the prevalence of pneumonia is higher in nonindustrialized and less-developed countries.
Perhaps one of the most worrying facts is the growing prevalence of bacterial antibiotic resistance, in particular, penicillin-resistant Streptococcus pneumoniae. Physicians need to be aware of local bacterial resistance information when choosing antibiotics to treat pneumonia. Vaccination of at-risk populations, such as the elderly, against S. pneumoniae should be part of public health strategy.
Nosocomial pneumonias constitute an important problem for hospital inpatients, especially the immune compromised or patients post major surgery. The control of MRSA (methicillin-resistant Staph. aureus) and multidrug-resistant enterococci requires not only careful choice of antibiotic for the individual patient but a combined strategy of general hygiene measures, monitoring of patients and staff for carriage of organisms, adequate information systems to track all data, clear prescribing policies, and active measures to prevent cross-infection.
Viral pneumonias are uncommon outside of epidemic situations. At the time of writing, there is much concern about the risk of a pandemic due to emergent strains of influenza virus, and much discussion of the measures that may be undertaken to minimize mortality. Based on previous experience, if a pandemic occurs, it will carry significant mortality worldwide.
Sleep Disordered Breathing
Mortality due to obstructive sleep apnea syndrome (OSAS) and other sleep-related disorders is not recorded in routine statistics. Given the known association with fatal road traffic accidents and that OSAS is a risk factor for hypertension, cardiovascular disease, and stroke, this information deficit is significant.
Prevalence figures have been estimated at up to about 5–7% of adult males and rather less in women. The management of OSAS is now a basic component of respiratory specialist services, and with the rise in obesity in affluent countries, the prevalence figures and resource requirements are likely to increase.
Tuberculosis
The recent WHO Report (2005) shows a stable or falling TB incidence in five of the six WHO regions, the exception being the African region and particularly countries with higher HIV prevalence rates. In 2003, the TB incidence rate was estimated to be rising by 1.0% per year globally. In the same year, there were 8.8 million new cases of TB and 1.7 million people died from the disease, of whom 229 000 were coinfected with HIV.
The WHO is strongly promoting the directly observed treatment strategy (DOTS) to improve outcomes and reduce the risk of acquired drug resistance. Tuberculosis remains a major public health issue worldwide.
Important Advances
The last decade has seen the development and/or the clinical application of several important advances in the investigation and treatment of respiratory diseases.
Molecular Biology And Genetics
Molecular genetics has already given us the ability to identify a range of genetic mutations that can lead to lung diseases, of which a good example is cystic fibrosis. Suspected cases can now be screened for a range of specific mutations. Molecular techniques are also applied for the identification of extrinsic causes of disease, such as the use of polymerase chain reaction (PCR) to identify the presence of M. tuberculosis, Pneumocystis carinii, and other microorganisms.
Similarly, identification of various mediators of inflammation has been followed by the development of monoclonal antibodies directed against specific molecules. These have applications in a range of chronic inflammatory diseases and tumors. In the respiratory field, these have proved to be a mixed blessing, and whereas monoclonal anti-immunoglobulin E (anti-IgE) treatment is beneficial in asthma, the use of anti-tumor necrosis factor (anti-TNF) alpha agents for rheumatoid arthritis has been associated with increased risk of tuberculosis and the need for particular vigilance. Molecular biology has also been applied to the production of surfactant and antiprotease to be used as replacement treatments. Unfortunately, these are expensive and only have application for relatively rare conditions, which makes it difficult to foresee their widespread clinical use.
Imaging Techniques And Treatment Innovations
Imaging techniques have been fundamental to the assessment of lung disease for nearly a century. Plain radiographs have been followed by the use of computed tomography (CT) scanning, and more recently, magnetic resonance imaging (MRI) and positron emission tomography (PET) scans. These modalities can be used for various lung diseases but play a critical role in the staging of lung cancer and selection of patients suitable for surgery. Currently, the use of combined PET/CT is being evaluated and may offer important advantages for this purpose.
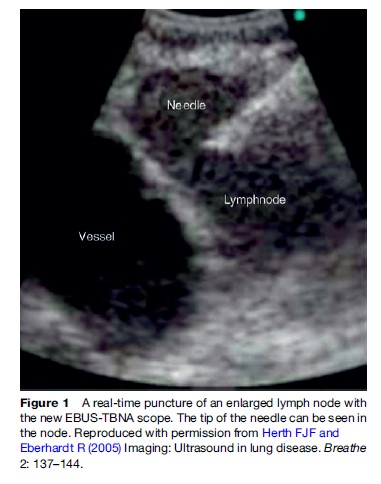
Another new technique is the use of endoscopic ultra- sound (EUS) or endobronchial ultrasound (EBUS) to guide needle biopsy of mediastinal lymph nodes for staging purposes. As Plat et al. (2006) have shown, this technique can be regarded as complementary to PET. Although conventional transbronchial node aspiration (TBNA) has been used for many years, its application was not widespread. Gasparini points out (2005) that only about 25% of bronchoscopists actually use the technique (Figure 1). Ultrasound-guided biopsy offers much promise but will require resources for training and equipment as well as collaboration between chest physicians and gastroenterologists.
Other interventional techniques for palliation of lung cancer, including stent insertion and cryotherapy, electrocautery, and laser ablation of tumors, have been developed, although use is mostly confined to pulmonary oncology centers. Spiro (2002) has reviewed these advances as well as recent developments in chemotherapy for both small cell and nonsmall cell lung cancer.
Turning from lung cancer to the other large and important area of COPD and respiratory failure, there has been increasing use of noninvasive positive pressure ventilation (NIPPV) for management of acute respiratory failure, considerably reducing the need for tracheal intubation and intensive care unit (ICU) care. The use of NIPPV has led to the development of respiratory high dependency units (RHDU), and guidelines for the organization of such developments are summarized in the European Lung White Book. If NIPPV use is expanded for patients with chronic stable respiratory failure, it will add to the complex infrastructural requirements for respiratory home care recently described by the American Thoracic Society (2005).
Lung transplantation programs continue to expand slowly. The survival of lung transplant recipients lags behind that of other organ recipients. Improving our understanding of post-transplant obliterative bronchiolitis is the focus for efforts to improve survival.
Keeping Up To Date
Continuing medical education (CME) and continuing professional development (CPD) are now an essential part of practice internationally. Specialist reaccreditation programs may be introduced by national regulatory agencies in the coming years. Respiratory medicine, through its major scientific societies, is actively pursuing this quality agenda. Close cooperation between the American Thoracic Society and the European Respiratory Society has led to the publication of joint position statements on various topics, providing Internet-accessible information for the individual physician. For more general medical information, the up-to-date website offers a very useful starting point.
Bibliography:
- American Thoracic Society (2005) Statement on home care for patients with respiratory disorders. American Journal of Respiratory and Critical Care Medicine 171: 1443–1464.
- Bouros D and Antoniou KM (2005) Current and future therapeutic approaches in idiopathic pulmonary fibrosis. European Respiratory Journal 26: 693–702.
- British Thoracic Society (2001) The Burden of Lung Disease. London: Munroe and Forster Communications.
- Egan JJ (2004) Obliterative bronchiolitis after lung transplantation – a repetitive multiple injury airway disease. American Journal of Respiratory and Critical Care Medicine 170: 931–932.
- European Respiratory Society/European Lung Foundation (ERS/ELF) (2003) European Lung White Book. European Respiratory Society/ European Lung Foundation.
- Gasparini S and Silvestri GA (2005) Usefulness of transbronchial needle aspiration in evaluating patients with lung cancer. Thorax 60: 890–891.
- Herth FJF and Eberhardt R (2005) Imaging: Ultrasound in lung disease. Breathe 2: 137–144.
- Plat G, Pierard P, Haller A, et al. (2006) Endobronchial ultrasound and positron emission tomography positive mediastinal lymph nodes. European Respiratory Journal 27: 276–281.
- Spiro SG and Porter JC (2002) Lung cancer – where are we today? Current advances in staging and nonsurgical treatment (state of the art). American Journal of Respiratory and Critical Care Medicine 166: 1166–1196.
- World Health Organization (2005) Global Tuberculosis Control: Surveillance, Planning, Financing. WHO Report 2005. Geneva, Switzerland: WHO.
- Brennan NJ and O’Connor T (2004) Ireland needs healthier airways and lungs – the evidence (INHALE). Supplement to Irish Medical Journal 97: No. 1.
- British Thoracic Society (2005) BTS recommendations for assessing risk and for managing Mycobacterium tuberculosis infection and disease in patients due to start anti-TNF-Alpha treatment. Thorax 60: 800–805.
- King TE (2005) Clinical advances in the diagnosis and therapy of the interstitial lung diseases. American Journal of Respiratory and Critical Care Medicine 172: 268–279.
- Mapp CE, Boschetto P, Maestrelli P, and Fabbri LM (2005) Occupational asthma (state of the art). American Journal of Respiratory and Critical Care Medicine 172: 280–305.
- McNicholas WT (2005) Sleep apnoea syndrome. Breathe 1: 218–227.
- Murray CJL and Lopez A (1996) The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries and Risk Factors in 1990 and Projected to 2020. Boston, MA: Harvard School of Public Health.
- Pack AI (2006) Advances in sleep-disordered breathing (centennial review). American Journal of Respiratory and Critical Care Medicine 173: 7–15.
- Spiro SG and Silvestri GA (2005) One hundred years of lung cancer (centennial review). American Journal of Respiratory and Critical Care Medicine 172: 523–529.
- Stark P (2006) Use of imaging studies in the staging of non-small cell lung cancer. http://www.uptodate.com (accessed November 2007).
- Studer SM, Levy RD, McNeil K, and Orens JB (2004) Lung transplant outcomes: A review of survival, graft function, physiology, health related quality of life and cost-effectiveness. European Respiratory Journal 24: 674–685.
- Troosters T, Casaburi R, Gosselink R, and Decramer M (2005) Pulmonary rehabilitation in chronic obstructive pulmonary disease (state of the art). American Journal of Respiratory and Critical Care Medicine 172: 19–38.
- Vilmann P and Larsen SS (2005) Endoscopic ultrasound – guided biopsy in the chest: Little to lose, much to gain. European Respiratory Journal 25: 400–401.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








