This sample Sleep Disorders Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Introduction
Sleep is a function of the brain. As such, sleep develops, matures, and declines in consonance with other functions of the brain. Sleep is a universal phenomenon exhibited by most vertebrates. The ultimate physiological function of sleep remains enigmatic and unknown despite extensive research of this ubiquitous brain activity. Sleep intervenes in functions of growth, regeneration, and memory. In the new classification of sleep disorders, more than 80 clinical sleep disorders are codified.
Experiments have shown that sleep deprivation causes an increasing constellation of brain alterations leading to death in lower mammals if prolonged sufficiently. Severely sleep-deprived individuals have a strong tendency to fall asleep and appear slow when performing mental or motor tasks. Their motor responses are delayed, with increasing apathy, reduced motivation, decreased concentration, and poor memory as unavoidable microsleeps break the continuity of consciousness. Most individuals require between 6 and 8 h of sleep at night. In Mediterranean countries, the daytime siesta allows subtraction of an equivalent amount of time from nocturnal asleep.
Sleep is a preprogrammed function of the brain modulated by the circadian rhythm. In the adult individual, nocturnal sleep progresses in stages and cycles. In the first half of the night the four stages of non REM sleep predominate, whereas in the second half, REM (rapid eye movement) sleep or dream sleep is more prevalent. The fetus spends much of its time in REM sleep and the infant shows a great abundance of REM sleep. By 2 years of age, sleep has become consolidated to the nocturnal period with approximately 25% of the total time asleep in REM sleep. In old age, total sleep requirements continue to be 6–8 h every 24 hours, but deep stages of non-REM sleep decline while REM sleep remains at 20–25% of total sleep.
The nocturnal evolution of sleep stages can be recorded with polysomnography, a technique central to the sleep laboratory that combines recording of brain waves, eye movements, electrocardiography, electromyography, respiratory motions, and saturation of oxygen. Videotaping of the individual asleep is an integral part of polysomnography.
Sleep is important in medicine because it influences quality of life, while its disorders provoke family pathology, disturb work routines, alter social activities, reduce quality of life, and affect the health of the individual. Sleep disorders are prevalent and pervasive. Excessive daytime somnolence may lead to motor vehicle accidents, poor academic performance, reduced work productivity, and social decline. Sleep disorders medicine counts with diagnostic tools centered in the sleep laboratory to diagnose sleep disorders, and sleep specialists can procure comprehensive management of most sleep afflictions.
Sleep research focuses in brain mechanisms and the consequences of sleep-related alterations. Over the years, landmarks in sleep research have included the discovery of changes in brain waves during sleep, the discovery of the sleep cycles and of REM sleep, the localization of REM mechanisms to the brainstem, and the discovery of hypocretin (also called orexin), a neurotransmitter necessary for alertness produced by the hypothalamus.
History
Sleep was often assumed to be a passive response to reduced cerebral stimulation during mental and cerebral inactivity. Berger’s demonstration of changes in the electroencephalogram (EEG) during sleep provided the first definite evidence that the brain is not passive during sleep. In the twentieth century, studies of encephalitis lethargica, hypothalamic and thalamic stimulation, and the reticular activating system of the brain provided major advances in the understanding of the neuroanatomical substrate of sleep and wakefulness. The discoveries of rapid eye movement (REM) sleep, the association of dreaming with REM sleep, and the periodic cycles of REM and non-REM sleep throughout the night led to a new view of sleep as an active process with distinctive neurophysiological substrates underlying the two major sleep states, non-REM and REM sleep.
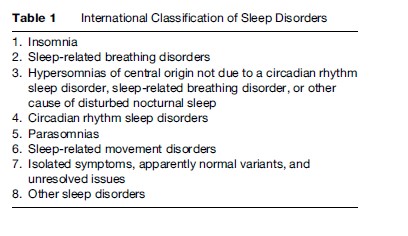
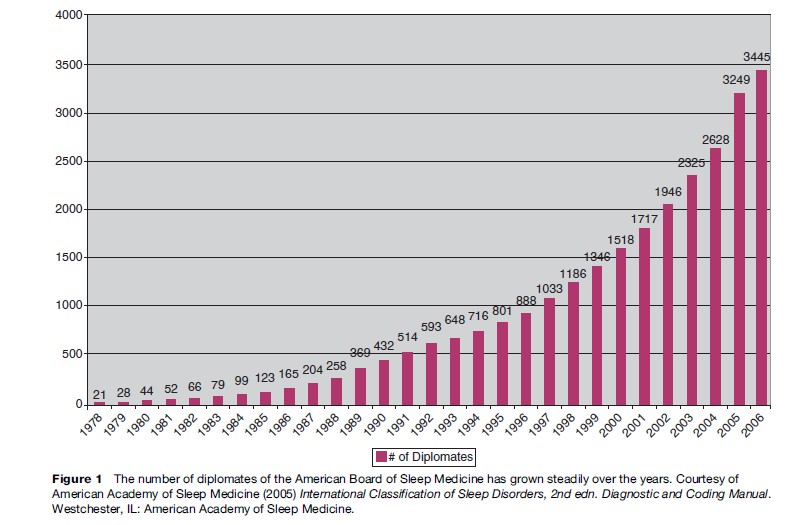
Physicians have known for centuries that sleep disturbance is often a sign of disease, but the recognition that primary sleep disorders are common, serious, and often treatable occurred mainly in the second half of the twentieth century. The first sleep clinics devoted specifically to diagnosis and treatment of a broad range of sleep disorders appeared in the 1970s. Also, in the United States, the Association of Sleep Disorders Centers, organized in 1975, provided a focus for development of the field of sleep disorders medicine. Subsequent major events included the publication of specialized journals. As the breadth of the field expanded, it became apparent that a nosology devoted to sleep disorders was required. The Association of Sleep Disorders Centers published the first classification of sleep disorders in 1979. A more comprehensive classification published by the American Sleep Disorders Association in 1990 as the International Classification of Sleep Disorders was revised in 2000, and updated in 2005 by the American Academy of Sleep Medicine (Table 1). By the end of 2006, 3445 professionals were diplomates of the American Board of Sleep Medicine (Figure 1). The first board exam on sleep given by the American Board of Medical Specialties took place in November 2007.
The Sleep Center
Patients with sleep disorders are evaluated by sleep specialists in sleep centers and tested in the sleep laboratory with polysomnography, a technique that records sleep parameters such as brain waves, eye movements, muscle tone, and breathing patterns. Sleep laboratory testing with nocturnal and daytime polysomnography is an indispensable procedure for the evaluation of patients with sleepdisordered breathing, pathological excessive daytime sleepiness, and complex motor disorders. Titration of positive airway pressure apparatuses can only be done in conjunction with polysomnography. Polysomnography involves at a minimum a full night stay in the sleep laboratory attended by properly trained technicians.
Laboratories accredited by the American Academy of Sleep Medicine use digital equipment and computer-assisted scoring techniques. Some night tests will be followed by daytime nap tests, also known as multiple sleep latency test (MSLT), or maintenance of wakefulness test (MWT). Patients report to the laboratory at 8.00 or 9.00 p.m. and are discharged the following morning at 8.00 a.m. or at 3.00–5.00 p.m. if a daytime test has been recorded. Scoring is usually done by a trained technician and the interpretation is carried out by the physician.
Actigraphy is a technique used to record body motion. Periods of quiescence during the 24-h period are associated with sleep, whereas periods of motion are associated with wakefulness.
Major Sleep Disorders
Sleep Apnea
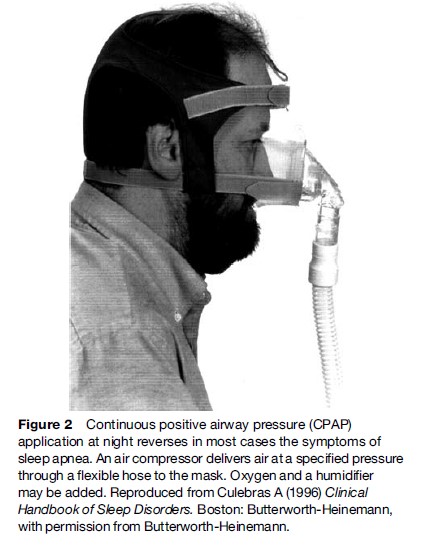
Sleep apnea, also known as sleep-disordered breathing, is a very common disorder and the major sleep-related risk factor for cerebrovascular disease. Sleep apnea syndrome affects 2% of women and 4% of men (Young et al., 1993). It appears more frequently past the age of 45 years and is more common in obese individuals. Loud disruptive snoring is a marker of sleep apnea and in itself a source of disease (Partinen et al., 1985). Frequent symptoms are lapses in respiration, restless sleep, excessive daytime somnolence, and depression. In addition, sleep apnea can increase the risk of stroke and myocardial infarction (Yaggi et al., 2005). Epidemiological studies have shown a dose–response relationship between the severity of sleep apnea and the odds ratio for development of systemic hypertension (Nieto et al., 2000). Sleep apnea is diagnosed with polysomnography in the sleep laboratory. Treatment with noninvasive positive airway ventilation is generally successful (Figure 2). For mild forms of sleep apnea, the application of mandibular advancement devices can be beneficial. Surgery removing excessive tissues in the oropharynx may be considered for individuals who cannot tolerate noninvasive equipment or who have obvious obstruction to airflow in the oropharynx by redundant tissue growth. There is proof that successful correction of sleep apnea with noninvasive positive airway pressure ventilation lowers mean blood pressure (Becker et al., 2003). Excessive daytime somnolence generally improves with successful treatment of sleep apnea.
Narcolepsy
Narcolepsy is characterized by excessive sleepiness. Associated manifestations are cataplexy, sleep paralysis, and hallucinatory dreams at sleep onset (hypnagogic hallucinations). Men and women are equally affected. Onset is typically in the second or third decade of life, although childhood onset may occur and some patients are not diagnosed until middle age. Changes in sleep schedule, psychological stress, head trauma, or infections sometimes appear to precipitate symptoms.
Excessive sleepiness in narcolepsy is associated with repeated naps or lapses into sleep. Sleep tends to occur in boring or monotonous situations and may be temporarily forestalled by physical activity and mental stimulation. Patients often report episodes of amnesia with automatic behavior during which they may carry out complex nonsensical activities such as mixing inappropriate foods, writing incomprehensible sentences, or driving to the wrong destination. Accidents due to sleepiness and automatic behavior may occur while driving or operating dangerous equipment.
Cataplexy, a unique feature of narcolepsy, is characterized by sudden loss of muscle tone usually provoked by strong emotion, particularly laughter lasting a few minutes. Consciousness is preserved and memory is intact. Respiratory and oculomotor muscles are not affected. In some patients, episodes of cataplexy may occur almost continuously, a condition referred to as status cataplecticus. Cataplexy rarely precedes the onset of excessive sleepiness but may develop simultaneously with sleepiness or with a delay of 1–30 years.
Hypnagogic hallucinations are vivid perceptual experiences that occur at sleep onset, often associated with fear or dread. Sleep paralysis is a transient, generalized inability to move or to speak during the transition between sleep and wakefulness. The experiences are often frightening. Disrupted nocturnal sleep with frequent awakenings is common in patients with narcolepsy. Many patients report that narcolepsy seriously affects interpersonal, marital, work, and social relationships.
A large segment of patients with otherwise typical features of narcolepsy do not have cataplexy, a condition referred to as monosymptomatic narcolepsy. In rare cases, narcolepsy is the consequence of brain tumors, stroke, multiple sclerosis, and other neurological disorders that damage the hypothalamus.
Patients with narcolepsy have excessive REM sleep both during the night and day, along with vivid dreaming. Discovery of the involvement of the hypothalamic hypocretin-releasing system in narcolepsy has improved the understanding of the ultimate etiology of the disorder. Hypocretin is a brain neurotransmitter that enhances alertness (Baumann et al., 2005). Various injuries to the hypothalamic hypocretin-secreting cell group, from surgical injury to head trauma to immunologic aggression would explain narcolepsy and its gradations of severity (Mignot et al., 2002). The diagnosis of narcolepsy is made clinically and confirmed with sleep laboratory tests that show excessive presence of REM sleep in daytime recordings. Treatment is symptomatic with a variety of agents that enhance daytime alertness, reduce REM sleep, or improve the continuity of sleep at night.
Insomnia
Insomnia is characterized by repeated difficulty with sleep initiation, duration, consolidation or quality despite adequate time and opportunity to sleep. Insomnia should incorporate daytime impairment as a result of faulty sleep. Primary insomnia includes psychophysiological insomnia, idiopathic insomnia, and paradoxical insomnia or sleep state misperception. Psychophysiological insomnia is one of the most common forms of insomnia. It develops as a result of chronic, somatized tension anxiety and negative conditioning to sleep. The individual with psychophysiological insomnia has focused attention on the inability to sleep, which is perceived to be the only source of distress. Other emotional or mental concerns are minimized. The search for contributing factors such as stress, caffeine ingestion, and poor sleep hygiene is generally fruitful. Not uncommonly there is a triggering factor such as divorce or the death of a relative followed by perpetuating factors at the core of which is the negative conditioning to sleep.
Patients respond initially to hypnotic medications but long-term results are more favorable with cognitive behavioral modification and similar techniques imparted by psychologists. These methods include sleep restriction consolidation, sleep hygiene education, relaxation therapy, stimulus control therapy, and correction of distorted perception of sleep. Sleep laboratory tests are only exceptionally of value in the diagnosis of insomnia.
Restless Legs
The diagnosis of restless legs syndrome (RLS) is based on the clinical history. Essential criteria are an urge to move the legs usually accompanied or caused by uncomfortable or unpleasant sensations in the legs, onset or exacerbation with rest, relief with movement, and evening or night presentation. Supportive clinical features of the diagnosis of RLS are family history, favorable response to dopaminergic therapy, and periodic limb movements (PLMs). These are repetitive limb movements that occur mostly in sleep in up to 80% of the patients. PLMs can appear in other disorders, particularly in the normal elderly population. The diagnosis of RLS can be supported by the sleep laboratory evaluation when periodic limb movements appear, as it does in most nocturnal tracings of patients with RLS. The diagnosis is confirmed with the favorable response to dopaminergic drugs.
Parasomnias
Parasomnias are undesirable physical events or experiences occurring at sleep onset, within sleep or during arousal from sleep. Common parasomnias are somnambulism or sleepwalking (SW) and sleep terrors. Patients exhibiting these disorders tend to have more than one parasomnia because of a shared pathogenic substrate, a strong familial predisposition and precipitating factors in common that include sleep deprivation, insufficient sleep syndrome, and sleep apnea. Parasomnias generally appear in the developmental age, although some start also later in life, posing problems of differential diagnosis with organic neurological or psychiatric disorders.
Sleep walking consists of a series of complex behaviors initiated during an arousal from slow-wave sleep that may culminate in walking behavior, coupled with an altered state of consciousness and impaired judgment. Episodes tend to occur during the first third of the night and may occur several times per night. Additional infrequent behaviors are eating, performing sexual intercourse, urinating, or most dramatically climbing out a window and injuring oneself or others (homicidal behavior). Sleep walking is frequent in childhood (17%), peaking by age 12 with no gender difference. Adult sleep walkers (4% prevalence) are most often men. Co-occurrence of enuresis and sleep terrors is high in relatives of patients with sleep walking.
Sleep terrors consist of abrupt arousals from deep sleep accompanied by a cry or scream with autonomic nervous system activation and behavioral manifestations of intense fear. Characteristics are confusion, retrograde amnesia, occurrence during the first part of the night, and precipitation by spontaneous or other disorder-related sleep deprivation.
Nightmares or anxiety dreams are frightening events with dream content that awaken the individual from REM sleep. Following awakening, the subject is oriented to the environment with clear sensorium. Dream content usually involves an experience of immediate and credible threat to survival, security, or self-esteem. Dream anxiety attacks occur in REM sleep. There is good recall for the disturbing dream and no displacement from the bed; injuries are quite rare.
REM sleep behavior disorder is a REM sleep parasomnia characterized by violent behaviors driven by a dream (Scheck et al., 1987). Patients are most often men who punch, kick, thrash about, get out of bed, move furniture, and perform other complex movements while in REM sleep. Not uncommonly, injuries are inflicted to the bed mate or patient. REM sleep behavior disorder has been associated with Parkinson disease (Comella et al., 1998) and other neurodegenerative disorders. Treatment with medications is generally satisfactory.
Circadian Dysrhythmias
Sleep is optimal in both quality and quantity only when it occurs during a proper time-frame in a 24-h day cycle governed by the circadian rhythm. Similarly, wakefulness is optimal at certain hours during the 24-h period. The timing of sleep and wake is a complex function of both circadian and homeostatic processes. Attempts at falling asleep or staying awake at physiologically inappropriate times will result in sleep–wake disturbance. This is the consequence of misalignment of the intrinsic sleep–wake propensity of a person and the 24-h physical and social environment. The intrinsic rhythm may be abnormally shifted relative to the environmental time-cues (delayed or advanced sleep phase disorder), become disrupted (irregular sleep–wake disorder), or have different periodicity (free-running type). The physical environment may change faster than the adaptation ability of the intrinsic sleep–wake rhythm (jet lag), or an individual may choose to disregard the intrinsic rhythm and voluntarily choose to stay awake at an inappropriate time (shift-work disorder). All these disturbances fall within the category of the circadian dysrhythmias, a group of intrinsic or acquired disorders of sleep and wakefulness.
Social Implications
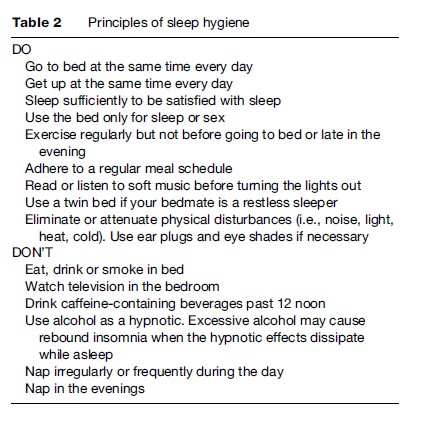
Sleep–wake disorders decrease the quality of life and disrupt social activities. In addition there is a risk of medicolegal troubles (Mahowald et al., 2005). Academic decline is a distinct risk in sleepy subjects. Many individuals have no respect for sleep compliance or ignore the basic rules of sleepy hygiene. Sleep deprivation results when sleep hygiene is violated. The basic principles of sleep hygiene are listed in Table 2.
Individuals with excessive daytime somnolence and a tendency to fall asleep driving should not drive until the problem has been solved or brought under control. Situations that increase drowsiness and risk of accidents are driving at night, driving alone, or along monotonous stretches of road. If sleepy, the driver should stop the car and take a brief nap. All other measures are of no useful relief.
Past the age of 45 years, individuals tolerate poorly circadian rhythm violations and work shift schedules. Consideration should be given to eliminate shift work past this age. Jet lag is best alleviated by adopting immediately the sleep–wake schedule of the destination with the aid of a short-duration hypnotic, if necessary.
Bibliography:
- Baumann CR and Bassetti CL (2005) Hypocretins (orexins) and sleep-wake disorders. Lancet Neurology 4: 673–682.
- Becker H, Jerrentrup A, Ploch T, et al. (2003) Effect of nasal continuous positive airway pressure treatment on blood pressure in patients with obstructive sleep apnea. Circulation 107: 68–73.
- Comella CL, Nardine TM, Diederich NJ, and Stebbins GT (1998) Sleep-related violence, injury, and REM sleep behavior disorder in Parkinson’s disease. Neurology 51(2): 526–529.
- Mahowald MW and Schenck CH (2005) Violent parasomnias: Forensic medicine issues. In: Kryger MH, Roth T and Dement WC (eds.) Principles and Practice of Sleep Medicine, 4th edn., pp. 960–968. Philadelphia, PA: Elsevier/Saunders
- Mignot E, Lammers GJ, Ripley B, et al. (2002) The role of cerebrospinal fluid hypocretin measurement in the diagnosis of narcolepsy and other hypersomnias. Archives of Neurology 59: 1553–1562.
- Nieto FJ, Young TB, Lind BK, et al. (2000) Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Journal of the American Medical Association 283: 1829–1836.
- Partinen M and Palomaki H (1985) Snoring and cerebral infarction. Lancet 2: 1325–1326.
- Schenck CH, Bundlie SR, Patterson AL, and Mahowald MW (1987) REM sleep behavior disorder: a treatable parasomnia affecting older adults. Journal of the American Medical Association 257: 1786–1789.
- Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, and Mohsenin V (2005) Obstructive sleep apnea as a risk factor for stroke and death. New England Journal of Medicine 353: 2034–2041.
- Young T, Palta M, Dempsey J, et al. (1993) The occurrence of sleep-disordered breathing among middle-aged adults. New England Journal of Medicine 328: 1230–1235.
- American Academy of Sleep Medicine (2005) International Classification of Sleep Disorders, 2nd edn. Diagnostic and Coding Manual. Westchester, IL: American Academy of Sleep Medicine.
- Culebras A (2006) Sleep Disorders and Neurological Disease, 2nd edn. New York: Informa Healthcare.
- Jouvet M and Delorme F (1965) Locus coeruleus et sommeil paradoxal. Comptes Rendues des Se´ances et Me´moires de la Socie´te´ de Biologie 159: 895–899.
- Kryger MH, Roth T and Dement WC (eds.) (2005) Principles and Practice of Sleep Medicine, 4th edn. Philadelphia, PA: Elsevier/ Saunders.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








