This sample Tuberculosis Diagnosis Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Introduction
Definitions
Tuberculosis is a disease caused by a mycobacterium from the Mycobacterium tuberculosis complex. These comprise M. tuberculosis, M. bovis, M. africanum, and M. microti. For a case of tuberculosis to be confirmed, it is necessary to isolate one of these organisms from the affected organ or organs (Migliori et al., 1999).
Definition of a case depends on the degree of certainty of diagnosis and may vary from country to country. For example, a definite case is defined in the European guidelines as ‘‘a case with culture confirmed disease caused by M. tuberculosis complex’’ or, in countries where culture confirmation is not possible, as ‘‘a patient with two consecutive sputum smear examinations positive for acid-fast bacilli or one positive sputum examination, radiological signs and a clinician’s decision to treat.’’ The guidelines go on to define ‘‘other than definite causes’’ as those meeting both of the following conditions: ‘‘(1) a clinician’s judgement that the patient’s clinical and/ or radiological signs and/or symptoms are compatible with TB, and (2) a clinician’s decision to treat a patient with a full course of chemotherapy’’ (American Thoracic Society, 2000).
The American guidelines define ‘‘tuberculosis, clinically active’’ as a person with ‘‘clinical, bacteriological, and/or radiographic evidence of current tuberculosis,’’ so-called Class 3. A separate case of ‘‘tuberculosis suspect (diagnosis pending),’’ the definition state ‘‘should be so classified when a diagnosis of tuberculosis is being considered whether or not treatment has been started, until diagnostic procedures have been completed.’’ The definition continues, ‘‘persons should not remain in this class for more than three months.’’ These patients are allocated to Class 5.
The guidelines go on to say that all positive smear, culture, susceptibility, and nucleic acid amplification results should be reported.
Patients may also be defined according to whether they have had previous treatment, as relapse or not new.
Clinical Practice
In clinical practice, a large proportion of patients are probably treated without bacteriological evidence either by smear or culture.
In a recent survey of cases of tuberculosis in England and Wales, no culture confirmation was made in 40% of notified cases (34% of those with pulmonary disease and 50% of those with nonpulmonary disease). Inevitably, the proportion with no positive culture results was much higher in children, 78%, compared with 38% in adults. A smear-positive result was only obtained in 43% of patients with pulmonary disease.
Tuberculosis can be one of the easiest diagnoses to make. A patient may present with characteristic symptoms, a chest radiograph may show a characteristic pattern of disease, and sputum is easily obtained and shows positive on smear and later culture. Tuberculosis, on the other hand, can also be one of the most difficult diagnoses to make, particularly at a nonpulmonary site. Eventually, the clinician may be forced to start treatment as a trial of therapy and hope the patient will improve. I have had a few patients in this category, who, after completion of treatment, left me unsure as to whether they had actually had active disease.
Because tuberculosis cannot always be confirmed by laboratory means, the full clinical armamentarium of symptoms and signs must be used toward the diagnosis.
Symptoms
Epidemiological Setting
Whenever a patient presents to a health-care professional in need of a diagnosis, the epidemiological pattern of disease is a factor by which the health-care professional will be helped to come to a diagnosis. Tuberculosis is very much more common in developing, resource-poor countries than in developed, richer countries. Individuals born in developing countries will therefore carry a much higher risk. For example, in the UK, only approximately one case of tuberculosis in every 20 000 white persons is found annually. The risk is ten times greater in the Chinese population, 20 times greater in the South Asian, and 50 times greater in the African population. The risks remain high in second and third-generation immigrants. The ethnic origin of the presenting patient must therefore be borne in mind when coming to a diagnosis.
Pulmonary Disease
Tuberculosis may present without symptoms, for example, when an individual who has been in contact with an infectious case is screened and found to have disease. Up to 50% of childhood tuberculosis may be detected in this way.
The characteristic symptoms of pulmonary tuberculosis in approximate decreasing order of frequency are:
- cough,
- malaise,
- fever,
- weight loss,
- night sweats,
- breathlessness,
- chest pain.
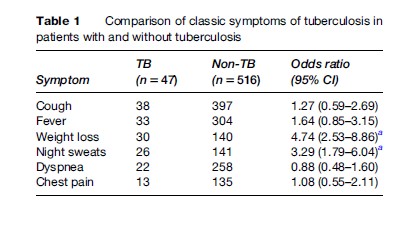
In a comparative study of patients with culture-proven pulmonary tuberculosis compared with patients with some other pulmonary infection, only weight loss and night sweats were helpful in distinguishing TB from other chest diseases (Table 1).
The cough of tuberculosis is typically constant and irritating. Initially, it may be unproductive, but as disease progresses and caseation goes on to cause cavitation within the lung parenchyma, it may become profusely productive of sputum. Rupture of a blood vessel may lead to hemoptysis, which may be dramatic and rarely life-threatening.
Malaise is of gradual onset but is likely to demotivate the patient so that after a few weeks of the disease, they want to do nothing but rest.
Fever is normally low-grade, rarely rising above 40ºC and characteristically low in the morning and peaking at night.
Weight loss is gradual, but if treatment is not started it may become dramatic over the space of a few months, the patient going on to lose 50% of body mass or more.
Night sweats may be profuse. ‘‘I thought I had wet the bed, doctor.’’ They may continue for some months after treatment has been started.
Breathlessness is a late feature occurring only when a substantial part, probably more than 20%, of the lung has been destroyed. In patients with preexisting lung disease, this symptom may occur earlier. Chest pain is a relatively common feature. It may be pleuritic in nature if disease is localized to a lung surface but can also be vague and difficult for the patient to locate precisely.
All these symptoms may occur in other chest diseases. It is of interest that the study detailed in Table 1 showed that only weight loss and night sweats were useful as distinguishing symptoms from other chest diseases. It should be emphasized that some or indeed all of these symptoms may be absent in the tuberculosis patient or present to different intensities.
Signs
Examination of the patient with pulmonary tuberculosis is usually unrewarding. The commonest sign is the patient being underweight, sometimes markedly so. Clinical anemia may be present. When the disease is chronic with long-standing lung and airway distortion, clubbing of the fingers may be present. It is remarkable how extensive radiographic changes may be without abnormal physical signs present. There may be reduced expansion of one or both sides of the chest. Dullness to percussion may be present and the breath sounds may be reduced or even absent. Crackles may be heard over the affected portion of lung. Endobronchial tuberculosis can cause pronounced narrowing of major bronchi so that a fixed monophonic wheeze may be heard. In chronic disease where an element of healing and fibrosis has taken place, there may be distortion of the upper airway so that tracheal deviation toward the side that is most affected can be detected. Amphoric breathing caused by air passing across a large cavity may be heard. In very extensive disease, the patient may appear breathless at rest due to pulmonary insufficiency. If a very large fluid-containing cavity is present, a succusation splash may be elicited. (The patient is rocked back and forth while seated upright and then suddenly stopped from moving. A splashing sound caused by liquid in the chest continuing to move backward and forward is heard on auscultation.)
A full examination may reveal signs of tuberculosis at other sites. Pulmonary and nonpulmonary disease may coexist, particularly in immunosuppressed patients.
All these signs may be present in other chest diseases and are therefore not diagnostic on their own.
Investigations
As is the case for any disease, investigation to diagnose tuberculosis may be nonspecific or specific. The chest radiograph is an example of a nonspecific investigation. It may provide a clue toward the diagnosis, but this can only be confirmed by the specific bacteriological investigations of smear and culture.
Radiographic Changes
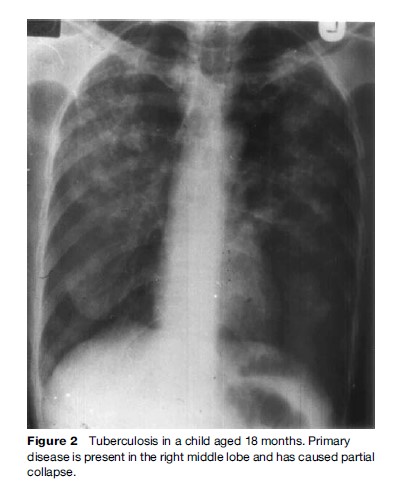
No radiographic pattern is diagnostic of tuberculosis. Some patterns are highly characteristic of tuberculosis but it should be remembered that the disease can only be confirmed bacteriologically. The distribution or radiological shadowing shows a predilection for the upper lobes and particularly the posterior segments. Bilateral disease is common, the shadowing being fluffy or patchy or nodular. Cavitation may be present, which can vary from multiple small cavities less than 1 cm in diameter to a single cavity occupying most of a lobe. In severe disease, the upper parts of the lung may be completely destroyed, leaving air spaces as infection and shadowing move into the reaming lower lobes (Figures 1, 2, and 3).
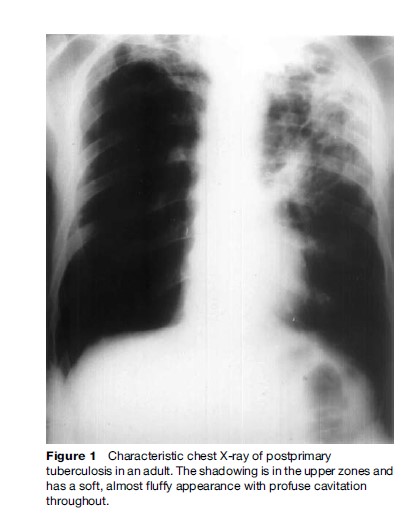
Chronic disease may result in volume loss and fibrosis, with elevation of the hila and if the disease is predominantly unilateral in deviation of the trachea and mediastinum. Calcification may develop after some time, usually years, and indicates a degree of healing. The presence of soft-edged shadows in the region of calcification suggests reactivation of previously healed disease. The presence of shadowing does not necessarily indicated active disease. This can only be shown by bacteriological methods. Inactivity can only be shown by negative sputum cultures and the failure of a particular radiographic lesion to change with time or treatment.
A normal chest radiograph may be present even in bacteriologically proven disease. Tuberculosis may present with virtually any radiographic pattern so the clinician may miss the diagnosis of tuberculosis if appropriate specimens are not sent. This is particularly true where the patient is immunosuppressed, as can occur in AIDS.
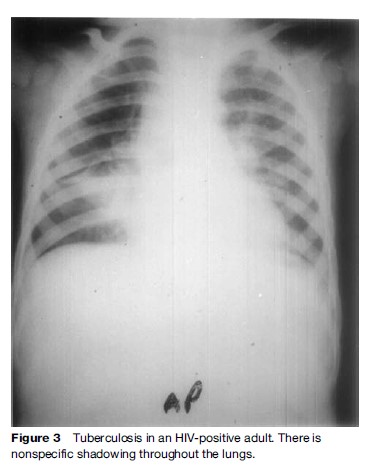
Miliary disease can present with innumerable small lung nodules. This usually occurs as a result of lymphohematogenous dissemination.
Other radiographic techniques such as CT scanning do not add very much to the diagnosis of tuberculosis but can be useful in establishing or excluding a differential diagnosis.
In very poorly resourced countries, the chest radiograph should only be done after several sputum smears have been negative on direct smear for acid-fast bacilli and a course of broad-spectrum antibiotics have failed to give relief of symptoms.
Primary tuberculosis as distinct from post primary disease described above results in a completely different pattern of radiographic change, characterized by hilar and paratracheal lymph gland enlargement with or without adjacent lung shadowing. Though this pattern is more common in children (see ‘Diagnosis in Children’ below), it may occur in adults, in the UK, particularly in those of Indian subcontinent ethnic origin.
Bacteriology
Sputum Smear
The unique character of the mycobacteria is that they are acid fast. Once stained with an aniline dye such as carbol fuchsin, they resist discoloration with acid and alcohol and are therefore termed acid and alcohol-fast bacilli or AAFB, usually shortened to acid-fast bacilli or AFB. The fixed smear is then counterstained with methylene blue or malachite green so that the AFB are seen as red bacilli on a blue-green background (Figure 4(a)).

This allows the detection of AFB specimens using a simple staining technique described by Ziehl in 1882 and modified by Neelsen in 1883. This is now universally known as the Ziehl-Neelsen (ZN) technique, and despite being over 100 years old, it remains the major tool in the rapid diagnosis of tuberculosis.
The one modification of the ZN technique is the use of a fluorescent stain such as auramine and light from an ultraviolet source. The advantage of this is that it is less onerous on the microscopist, although the rate of false positives is higher. Slides found positive on fluorescent staining should be checked by ZN staining. The equipment needed is also considerably more expensive (Figure 4(b)).
The detection of sputum by direct microscopy means that there are at least 5000 organisms/ml of sputum and sometimes up to ten times that number. Such a patient is considered to be infectious. Fewer than 5000/ml means that the smear is unlikely to be positive. In the UK, 56% of patients diagnosed as having pulmonary TB are sputum smear-negative. These patients are regarded, on the basis of a number of contact surveys, as noninfectious.
The main role of microscopy is therefore to identify the truly infectious patient so that the chain of infection can be halted by treatment. It is accepted that 2–3 weeks of treatment with standard antituberculosis drugs will render most patients noninfectious.
Specimens
Ideally, at least three sputum collections on successive days should be provided. A single specimen will miss approximately 25% of microscopically positive and approximately 50% of culture-positive cases. If sputum is not available, other means of obtaining a sample should be attempted. In children, this is best achieved by gastric aspiration. A nasogastric tube should be put in place overnight and the gastric contents aspirated as the child wakes in the morning. If the child is mature enough to obey instructions, he should be asked to cough and swallow for 10 min before aspiration.
In the adult, induction of sputum should be attempted using nebulized twice-normal saline for 10 min.
Alternatively, bronchoalveolar lavage using a fiberoptic bronchoscope, which enables specific site sampling, can be used. Care must be taken to ensure the bronchoscope is properly disinfected between cases, since false-positives on smear can occur because of contamination with environmental mycobacteria. Mycobacterium chelonei is the organism most likely to be involved.
Specimens from nonpulmonary sites will include aspiration of pleural fluid, pus from any abscess, and cerebrospinal fluid (CSF) for suspected meningitis. If possible, tissues from a site should be sent for culture.
To detect genitourinary disease, 50 ml of early morning urine specimen should be examined on successive days.
With the advent of HIV infection leading to AIDS, due to dissemination of infection, mycobacteria may be obtained from other specimens such as feces, blood, or bowel biopsies.
Culture
The isolation of M. tuberculosis in pure culture provides a definitive diagnosis. However, this is achieved in only approximately 80% of reported cases, even in developed countries, and the diagnosis then has to be made on the clinical and/or radiological features, sometimes with histological evidence (see below).
In the UK, the most commonly used medium for the isolation of tubercle bacilli is Lowenstein-Jensen (LJ). This is a simple egg-based medium that has undergone few modifications since its original description in the 1930s. From a sputum specimen positive by direct microscopy, LJ will show growth within 2–3 weeks at 37 C. The colonies are rough and beige to brown in color and show up well on the green background, because of the presence of malachite green. Smear-negative sputa and specimens from nonpulmonary sites may not give growth for 6–8 weeks.
Some laboratories use a liquid medium such as Kirchner, to which an antibiotic mixture can be added to help suppress the growth of other bacteria, but since it is a liquid reporting is more difficult because the liquid has to be centrifuged and ZN staining of the deposit then undertaken.
Other methods used include the BBL-Septi-Chek AFT system and the BACTEC460 radiometric system. Both of these use Middlebrook 7H9 broth. In the BACTEC system, the broth incorporates a [14C]-labeled substrate, producing [14C]-labeled CO2, which is automatically monitored in the head space gas by the machine.
Molecular Diagnostic Techniques
The advent of molecular technology has led to the development and implementation of tests that are both rapid and sensitive for the detection and identification of mycobacteria. They can be used in several ways: For the detection of mycobacteria, the specific detection of the M. tuberculosis complex, the differentiation of the M. tuberculosis complex, and the detection of drug resistance.
Molecular detection methods use some common steps, starting with the amplification of nucleic acid sequences. The best known and the most widely employed is the polymerase chain reaction (PCR). Other techniques include transcription-mediated amplification (Amplified PTC-2, Gen-probe, San Diego, CA, USA), strand displacement amplification (Probe-Tec ET, Becton Dickenson, Franklin Lakes, NJ, USA), and the QB replicase Galileo system (Gene-Trak/Vysis, IL, USA). These alternative techniques have shown comparable performance to PCR. Detection systems can be colormetric, such as in the line probe assay, or LiPA (Innogenetics, Zwijndrecht, Belgium) and Amplicor TB (Roche Diagnostics, Indianapolis, IN, USA) or through chemiluminescent or fluorescent tagging of probes.
A major problem for these molecular techniques is cost. While it is relatively easy to scale up production of kits of molecular detection methods, once they have been developed, their execution requires skilled laboratory personnel, the concurrent performance of multiple controls, several dedicated laboratory areas, and the use of relatively expensive consumable reagents. All of these factors make the costs prohibitive for laboratories in developing nations. Furthermore, in developing nations, where perhaps 95% of mycobacterial disease is due to the MTB complex, the use of molecular techniques to differentiate mycobacteria other than tuberculosis (MOTT) is of little benefit as the incidence of these infections is relatively rare.
Performance
The performance of molecular techniques in routine clinical use is hard to determine. While tests are being evaluated, they are performed by expert technicians in ideal conditions. Often, when these techniques are translated inappropriately to ill-equipped laboratories, performance will markedly decrease and contamination will generate many false-positive results. Without appropriate rigorous quality control, this may go undetected. The lack of a perfect gold standard for evaluation further complicates the issue. Discrepancies between culture data and molecular data are re-evaluated with reference to presumptive clinical diagnosis; however, where agreement is found the flawed gold standard is taken to be correct and to validate the result.
Similarly, the sensitivity of such tests is hard to determine. It is sometimes claimed that sensitivity will be theoretically as low as one bacillus, or genome equivalent; however, this is not generally borne out by experimental data. It is likely that organisms will be lost during sample preparation and, in the particular case of mycobacteria, clumping leads to uneven distribution of bacteria throughout the sample, so that duplicate tests often give discrepant results, which can be hard to interpret. The presence of inhibitors, such as drug metabolites or hemoglobin in the sample, can further reduce the sensitivity of the tests on individual samples. The expense of commercially available molecular diagnostic kits has led many laboratories to develop their own in-house assays, which, when suitably controlled, have similar sensitivity and specificity to those of commercial systems.
Limitations
While molecular diagnostic tests provide rapid results, they have several drawbacks. They cannot replace conventional culture techniques and must be used in conjunction with culture to ensure optimal isolation rates and to establish archive cultures for further studies. Multiple negative, positive, and inhibition controls must be performed with each assay, to assure quality and reliability, elevating costs and the time required. Tests should only be carried out by staff with an adequate level of training and skill in molecular testing. Due to the high cost of these tests in routine use, samples should be prioritized rather than tested universally.
Serological Testing
A wide variety of serological tests have been used in an attempt to diagnose tuberculosis. All have lacked necessary sensitivity and specificity because of the diversity of the antigenic determinant of the tubercle bacillus and exposure to environmental mycobacteria that share antigens with the tubercle bacillus. These methods have never progressed beyond the research stage and have been overtaken by more accurate molecular methods (see the section titled ‘Molecular diagnostic techniques’).
Interferon Gamma Release Assays
For nearly a century, the tuberculin skin test was the only tool available for the detection of latent tuberculosis infection. The last decade has seen the emergence of interferon-gamma release assays (IGRAs) for the diagnosis of tuberculosis infection in clinical practice. Two assays are currently commercially available, the Quantiferon-TB Gold and the ELISPOT assay. These tests involve the incubation of whole blood (Quantiferon) or peripheral blood mononuclear cells (ELISPOT) with antigens that are specific to Mycobacterium tuberculosis and quantifying the synthesis of interferon gamma by T cells to diagnose tuberculosis infection. Current evidence suggests interferon-gamma release assays have higher specificity than the tuberculin skin test, better correlation with surrogate markers of exposure to Mycobacterium tuberculosis in low-incidence settings, and less cross-reactivity as a result of BCG vaccination compared with the tuberculin skin test (Pai et al., 2007). While these tests have been investigated predominantly for the diagnosis of latent tuberculosis infection, recent evidence suggests that the tuberculin skin test and Quantiferon-TB Gold have similar sensitivity in persons with culture-confirmed infection. However, as with the tuberculin skin test, negative IGRA results do not exclude the diagnosis of tuberculosis (Mazurek et al., 2007). Furthermore, the sensitivity and specificity of these assays are unclear in children and in patients with HIV infection.
Differential Diagnosis
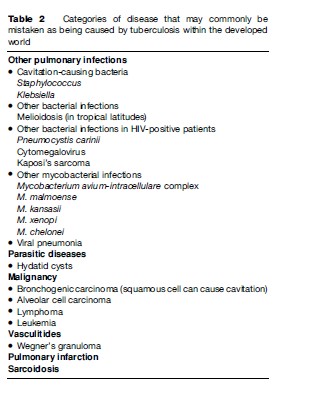
The differential diagnosis of tuberculosis depends very much on the geographical area of origin and the ethnic origin of the patient. Table 2 lists the categories of the disease that may commonly be mistaken as being caused by tuberculosis within the developed world.
Investigation Of Alternative Diagnoses
The isolation of M. tuberculosis confirms the diagnosis of tuberculosis. Where this has not been done, an element of doubt over the diagnosis remains.
First, have adequate specimens for bacteriology been obtained? If the patient is unable to produce sputum, using nebulized inhaled twice-normal saline may be used to carry out sputum induction. It is important that these procedures be carried out in an appropriate isolation chamber to ensure that cross-infection does not occur.
Bronchoscopy with lavage may also be used to obtain specimens. This procedure provides a means of directly visualizing the bronchial tree to exclude the presence of centrally located tumors. Bronchoscopy also provides a means of biopsy either directly or transbronchially using radiographic imaging. Histological examination of such biopsies is important in establishing a differential diagnosis such as malignancy.
Because of the increased risk of tuberculosis in HIVinfected individuals, HIV testing should be considered for any patient with disease.
If the diagnosis is suspected on a plain chest film, further radiographic imaging may help establish an alternative diagnosis. A lateral film can be helpful. The radiographic lesion caused by tuberculosis is characteristically posterior in its location in the upper or lower lobes. CT scanning can be helpful in establishing the exact site of a lesion and can be used for any site in the body. Magnetic resonance imaging is helpful in identifying lesions in solid tissue such as muscle or bone. Some form of direct imaging should be carried out if operative intervention to obtain tissue for diagnosis is being considered. Aspiration fluid such as pus from an abscess or pleural fluid should be carried out if present for bacteriology. The adenosine deaminase (ADA) concentration is usually raised in the latter. Lymph node disease can be established using fine needle aspiration.
Biopsy specimens should be sent for bacteriological culture as well as histology.
Serological testing often helps to diagnose Wegner’s granulomatosis when the antinuclear cytoplasmic antibody (ANCA) may be raised. The serum angiotensin converting enzyme (ACE) may be high in sarcoidosis.
Diagnosis In Children
The diagnosis in children is usually more difficult than in adults. The reason for this is that primary disease, which children usually suffer from, is paucibacillary, that is has relatively few bacilli, making bacteriological diagnosis problematic. Primary infection in the lung is the initial focus of inflammation in the alveolus and the proximal enlargement of the lymph glands draining the site.
In developing countries, approximately half of all children are diagnosed by screening the contacts of an adult patient with infectious disease. They are usually therefore asymptomatic when the diagnosis is made.
Presentation
A history of tuberculosis contact is therefore the single most important fact in diagnosing tuberculosis in children. They may present with symptoms of upper respiratory tract infection with cough, coryza, and malaise. A chest radiograph may show the features of primary tuberculosis with a small peripheral opacity at the site of initial infection (Gohn focus) and enlargement of the hilar and paratracheal glands on the same side of the chest (Figure 3).
Enlargement of the lymph glands surrounding a main bronchus or endobronchial tuberculosis may cause complete obstruction of a main bronchus with resulting collapse of the peripheral lung, causing an apparent sublobar or lobar pneumonia. Sometimes, only partial obstruction occurs so that air is drawn into the lung but not blown out, with resulting inflation of the affected lobe and even shifting away of the mediastinum.
Bacteriology
Bacteriological confirmation of disease in children, particularly under the age of 4 years, is the exception rather than the rule. Bacteriological specimens are best obtained by gastric aspiration. A nasogastric tube should be passed the night before and then the first aspirate after waking sent for bacteriology. If possible, the child should be induced to cough a few times before the aspiration is drawn off. Results from bronchoscopy are no more likely to be positive than from gastric aspiration.
Distinguishing Features
In a paper comparing children with confirmed TB with those who did not have TB but some other respiratory infection, only the history of household contact was found to be a distinguishing feature. The same study found no specific clinical feature such as weight loss, respiratory signs, or organomegaly helped to distinguish tuberculosis from a chest infection due to another cause. From radiography, only hilar gland or hilar and paratracheal gland enlargement were helpful distinguishing features.
The tuberculin test was significantly positive in only 41% of the children with confirmed tuberculosis. This compared with no children with a positive test among those not thought to have tuberculosis.
A number of authors have set up a scoring system for diagnosing tuberculosis in children. One such system divides the potential population in countries of low prevalence and high prevalence. A history of contact and a positive tuberculin test scores higher in the low-prevalence country score because children of a high-prevalence country are more likely to encounter infection in the community in which they live, outside of their own homes.
It should be said that these scoring systems have not yet been subjected to rigorous trials.
A recent study from Spain, which unfortunately did not include controls without tuberculosis, showed a 49.1% bacteriologically positive yield. This study included patients up to the age of 18. Bacteriological confirmation was higher in the older age group.
The Tuberculin Test
The tuberculin test is a test that detects previous infection with M. tuberculosis. It entails the injection of purified protein derivative (PPD) of M. tuberculosis into the skin. This can be done either with a single injection (the Mantoux test) or using a six-pronged, spring-loaded gun (the Heaf test). The efficacy of the test depends on the body’s ability to mount a type IV hypersensitivity to the injected protein when previously infected with M. tuberculosis. Different countries use different strengths of PPD and use different cut-off points to define a positive test. In the UK, the standard test uses 10 units of PPD (0.1 ml of 100 units/ml) for the Mantoux test, which is read 48–72 h after injection. A size of induration greater than 14 mm in diameter indicates infection. For the Heaf test, undiluted solution containing 100 000 International Units of PPD is smeared onto the skin and the spring gun caused to inject into the skin through the solution.
Interpretation of the test may be difficult. It is a test of infection, not necessarily disease. In the UK, 25% of the population over the age of 60 may be expected to have a positive test from infection incurred earlier in life. In the very elderly, positivity may wane due to decline in the efficacy of the immune system. The test may be rendered weakly positive by previous BCG vaccination or by infection with environmental mycobacteria. In severe disease, the tuberculin test may be negative. As a rule, it is a useful diagnostic test when positive in the young.
Diagnosis Of Nonrespiratory Disease
Central Nervous System Tuberculosis
Presentation
Onset is usually insidious, with fever, malaise, weight loss, headache, double vision, altered consciousness, and meningism. Cranial neuropathies resulting in double vision and facial weakness may occur in isolation. In infants, there may be failure to thrive and bulging of the fontanelles. Focal neurological signs such as weakness of one side or one limb or the upper or lower limbs together may occur.
Differential Diagnosis
Tuberculosis meningitis must be distinguished from other bacterial and viral meningitis. In HIV-positive patients, fungal or cryptococcal meningitis occurs in 5–10% of patients.
Investigation
The majority of cases of tuberculous meningitis occur in the developing world where resources in confirming the diagnosis are poor. Examination of the central spinal fluid (CSF) by a lumbar puncture is the cornerstone of investigations. Characteristically, there are white cells present, which are predominantly lymphocytes. The CSF protein concentration is usually raised (>500 mg/l) and glucose lowered, less than 60% of the blood sugar. Smear microscopy may be negative in up to three-quarters of patients and cultures negative in up to half. A great proportion of tuberculous meningitis cases are therefore not proven bacteriologically. The tuberculin test may be negative, because the ability to mount the immune reaction for the skin test may be compromised by the severity of the disease.
Superficial Tuberculous Lymphadenitis
This is the commonest form of extrapulmonary tuberculosis in both HIV-negative and HIV-positive individuals. The patient usually complains of swelling of the neck, in the submandibular or supraclavicular glands (beneath the jaw and above the collarbone). Glands in the axillae or the inguinal region (armpit or groin) may rarely be involved. Swelling is usually slow and painless, but they may be tender on palpation. The diagnosis is made by aspiration or biopsy.
If occurring in children, environmental mycobacteria rather than the tubercle bacillus is the usual cause in developed countries. In HIV-infected patients, the burden of bacteria may be so great that smear will show loads of bacteria. Smear results in the HIV-negative patient are usually negative.
Bone And Joint Tuberculosis
Half of all bone and joint tuberculosis affects the spine. The next most commonly affected areas are the other large weight-bearing joints. Other sites that may be involved include the elbow, shoulder, wrist, hand, and fingers. Nonarticular parts of the skeleton such as the ribs, scapula, or skull may be affected. As with other nonrespiratory sites, bone and joint disease is seen much more frequently in patients of Asian ethnic origin and HIV-infected patients.
The radiological features are often very characteristic. In vertebral disease, there is destruction of the disc with narrowing of the disc space. This is followed by destruction and collapse of the adjacent vertebral bodies starting anteriorly. The result is a collapse and forward flexion of the spine at the site of disease, with the typical deformity of Pott’s disease of the spine. In severe cases, the vertebral column may become unstable, with resultant crushing of the spinal column and paraplegia below the lesion.
In peripheral joint tuberculosis, the commonest radiographic abnormalities are bony erosions and destructive changes and joint space narrowing.
The diagnosis is based on the radiographic changes. Where possible, specimens should be obtained for bacteriology.
Gastrointestinal Tract And Peritoneal Tuberculosis
Tuberculosis should be considered in any patient with fever and abdominal symptoms, particularly if they are from a developing country or are HIV-infected. The most common symptom complex is malaise, abdominal pain, fever, and weight loss. Constipation is more common than diarrhea. Disease may present as an acute pain, and fever is more commonly slow and insidious at onset.
Infection may disseminate to the peritoneal cavity with fluid in the cavity (ascites) with distention.
Ascetic fluid may be aspirated for bacteriology. The diagnosis may be made at laparotomy, where white dots (tubercles) can be seen studded throughout the abdominal contents. The unsuspecting surgeon may confuse the appearance with secondary carcinoma, but histological specimens and bacteriology will show tuberculosis. High levels of ADA may be found in the fluid. Radiography such as plain abdominal film, barium meal and follow-through, enema, and CT scanning may lead to a suspicion of tuberculosis but are nonspecific. Bulky mesenteric or retroperitoneal lymph nodes may be seen and be mistaken for lymphoma or carcinoma.
Genitourinary Disease
Urinary tract disease characteristically presents with pain on passing urine, blood in the urine, and loin and abdominal pain. Constitutional symptoms such as fever, weight loss, malaise, and night sweats are unusual. Any part from the kidney to the urethra may be affected.
In the male, the most common sites affected are the epididymis and the prostate gland. Presentation is usually with pain and swelling. The commonest presentation in the female is infertility followed by pelvic pain, excessive menstrual loss, amenorrhea, and vaginal discharge.
Diagnosis may be suspected by radiographic (an intravenous urogram) or CT investigation. This characteristically shows dilatation of the renal pelvis with ureteric stricture. Calcification within the renal pelvis and in other extrarenal sites may be seen in chronic disease. Culture of M. tuberculosis is the key to diagnosis. Early morning urine specimens should be taken for culture on at least three consecutive days. A positive smear is unusual. The diagnosis may be made histologically from a surgical specimen if tuberculosis is not suspected (see below).
Pericardial Tuberculosis
This usually occurs in young adults and presents insidiously as fever, night sweats, malaise, weight loss, substernal pain, fast heart rate, cough, and a pericardial friction rub. If there is a pericardial effusion with tamponade, there may be breathlessness, reduced blood pressure, a raised jugular venous pressure, an enlarged liver, and peripheral edema. The chest X-ray may show an enlarged cardiac shadow with pleural effusions. In chronic constrictive pericarditis, calcification of the pericardium may be seen on X-ray. Pulmonary tuberculosis may also be seen.
An echocardiogram may show the presence of an effusion or thickening of the pericardium. Adenosine deaminase (ADA) may be raised in the pericardial fluid. Diagnosis is confirmed by identifying M. tuberculosis. This is unusual from the fluid, but a positive result is more likely from a pericardial biopsy.
Tuberculosis Of The Skin
Cutaneous tuberculosis is rare but is re-emerging where HIV infection is prevalent. A primary cutaneous skin complex may occur by direct inoculation of tubercle bacilli into the skin by trauma. The commonest form of secondary cutaneous tuberculosis is lupus vulgaris in which dull, reddish, thickened lesions appear on the head, face, and limbs. It is slowly progressive and may take many years to diagnose. The diagnosis may be made by histology but is always only confirmed by bacteriology.
Ethnic Minority Groups
Because nonrespiratory tuberculosis is so much more common in ethnic minority persons, tuberculosis should be considered if any symptoms or signs persist for more than 6 weeks, for example, backache or a swelling, in such an individual.
Histological Features
The basic inflammatory response to infection by M. tuberculosis is the granuloma. This consists of a chronic, compact collection of activated macrophages, the principal bacteria-engulfing cells in the blood, which are termed epithelioid cells once positioned in the granuloma. Some of these fuse together to form multinucleated giant cells. In time, many granulomas may fuse together. The central part may then break down to form a cheese-like material, so-called caseous necrosis. The histological appearance is virtually diagnostic of mycobacterial infection. Granuloma formation without caseation may be caused by a number of diseases including sarcoidosis, leukemia, and a foreign body. A positive histological finding may be present in any organ system.
Diagnosis In HIV-Infected Individuals
The diagnosis may frequently be missed in HIV-infected individuals because the infection can substantially alter the way tuberculosis affects the patient and therefore the presentation can vary.
The patient is likely to be very much more ill and prostration may occur. The tuberculin test is often negative.
The presence of lung cavitation is less frequent in the HIV-infected tuberculosis patient so that the concentration of bacteria in expectorated sputum is not as great. The result is that the diagnosis based on sputum smear positivity is not so easily made. This is particularly problematic as HIV-positive tuberculosis is commonest in the poorest countries of Africa, where more expensive methods of diagnosis such as culture are not routinely available.
The radiographic pattern of disease in HIV may not show the characteristic upper zone shadowing and cavitation. There may be generalized shadowing throughout the lung fields or predominantly lower-zone shadowing. As a general rule, the lower the patient’s CD4 count, the less characteristic the pattern is likely to be.
Nonpulmonary sites, particularly meningeal disease and disseminated disease, are more likely, particularly as CD4 counts fall. Bacterial counts within tissue are very much higher than in HIV-negative disease, and a smear of a tissue biopsy may show ZN-fast organisms in profusion. Also, bacteriological examination of blood and feces is more likely to be positive than in the HIV-negative patient.
Diagnosis In Resource-Poor Settings
In very poor countries, the expense of chest radiography in the diagnosis of tuberculosis should be avoided if possible. A patient with symptoms of tuberculosis, particularly if they have had a cough for more than 3 weeks, should provide up to three specimens of sputum. If these are negative, the patient should be treated with a broadspectrum antibiotic for 2 weeks. If symptoms persist, sputum specimens should again be sent for AAFB smear. Only if all the sputum samples are negative should a chest radiograph be done to establish a possible diagnosis.
Conclusions
Tuberculosis is a disease caused by M. tuberculosis, which can affect any organ in the body but most commonly affects the lungs.
The diagnosis of tuberculosis is made first on the basis of symptoms, which is what the patient complains of. In pulmonary disease, these are most commonly cough, weight loss, malaise, night sweats, and less commonly, chest pain and breathlessness. Secondly, the diagnosis is made by the signs, which the health professional elicits, on examination of the patient. These may be relatively few but include fever, evidence of weight loss, and in advanced disease, alteration in breath sounds characteristic of pneumonia, usually in the upper lobes. Thirdly, the diagnosis is made on the basis of investigations, which may be specific or nonspecific. The chest radiograph is an example of a nonspecific investigation, which may lead to a suspicion of tuberculosis but cannot prove the presence of the disease.
Only the isolation of M. tuberculosis complex from a sample from the patient, usually sputum, can confirm the presence of tuberculosis.
Bibliography:
- American Thoracic Society (2000) Diagnostic standards and classification of tuberculosis in adults and children. American Journal of Respiratory and Critical Care Medicine 161: 1376–1395.
- Davies PDO (1998) Clinical Tuberculosis, 2nd edn. Dordrecht: Springer.
- Mazurek GH, Weis SE, Moonan PK, et al. (2007) Prospective comparison of the tuberculin skin test and 2 whole-blood interferon-gamma release assays in persons with suspected tuberculosis. Clinical Infectious Diseases 45: 837–845.
- Migliori GB, Raviglione MC, Schaberg T, et al. (1999) Tuberculosis management in Europe. Recommendations of a Working Group of the European Respiratory Society (ERS), the World Health Organization (WHO), and the International Union Against Tuberculosis and Lung Disease, European Region (IUATLD). European Respiratory Journal 14: 978–992.
- Pai M, Dheda K, Cunningham J, Scano F, and O’Brien R (2007) T-cell assays for the diagnosis of latent tuberculosis infection: Moving the research agenda forward. Lancet Infectious Diseases 7: 428–438.
- Crofton J, Horne N, and Miller F (1999) Clinical Tuberculosis, 2nd edn. New York: MacMillan.
- Davies PDO (ed.) (2008) Clinical Tuberculosis, 4th edn. London: Chapman and Hall.
- Davies PDO and Ormerod LP (1999) Case Presentations in Clinical Tuberculosis. London: Arnold.
- Davies PDO, Girling DJ, and Grange JM (1996) Tuberculosis. In: Weatherall DJ, Ledingham JGG, and Warrell DA (eds.) Oxford Textbook of Medicine, 3rd edn., pp. 638–660. Oxford, UK: Oxford University Press.
- Fourie PB, Becker PJ, Festenstein F, et al. (1998) Procedures for developing a simple scoring method based on unsophisticated criteria for screening children for tuberculosis. International Journal of Tuberculosis and Lung Disease 2: 116–123.
- Harries AD and Maher D (1996) TB/HIV: A Clinical Manual. Geneva, Switzerland: World Health Organization.
- Merino JM, Alvarez T, Marrero M, et al. (2001) Microbiology of pediatric primary pulmonary tuberculosis. Chest 119: 1434–1438.
- Rom WN and Gary S (eds.) (1996) Tuberculosis. Boston, MA: Little Brown and Co.
- Rose AMC, Watson JM, Graham C, et al. (2001) Tuberculosis at the end of the 20th century in England and Wales: Results of a national survey in 1998. Thorax 56: 173–179.
- Schaaf HS, Beyers N, Gie RP, et al. (1995) Respiratory tuberculosis in childhood: The diagnostic value of clinical features and special investigations. Pediatric Infectious Diseases 14: 189–194.
- Seaton A, Seaton D, and Leitch AG (2000) Crofton and Douglas’s Respiratory Diseases. Oxford, UK: Blackwell Science.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








