This sample Mood Disorders Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of psychology research paper topics, and browse research paper examples.
Mood and emotion add depth and meaning to our lives and to our interactions with other people. Our moods change from day to day, sometimes quite unexpectedly. We all suffer from “the blues” occasionally, and it is hoped we all experience periods of blissful happiness. It is important, however, to differentiate between mood disorders, formerly known as affective disorders, and normal mood fluctuations.
The purpose of this research-paper is to provide an overview of current as well as historical conceptualizations of mood disorders. Diagnostic criteria, etiological theories, and treatment strategies are discussed.
Consider the following individuals. Which of them appear to be suffering from a mood disorder?
Jon, 21, was arrested and charged with careless and reckless operation of a motor vehicle after he was clocked driving his car at 90 mph near the college campus where he is enrolled as a senior. The arresting officer suspected that Jon was under the influence of alcohol or drugs but all toxicology screens yielded negative results. While being transported to the jail, Jon was belligerent and tried to strike an officer. Once he was put into a cell, Jon continued to talk loudly and rapidly throughout the night.
Ellen, 23, never seems happy. Her friends, who’ve known her since childhood, agree that she has seemed sad more days than not since finishing college two years ago. Ellen evidences low self-esteem and has difficulty making decisions. Her friends have begun to avoid her because she seems so “needy.” Ellen’s appetite and sleep patterns are within normal limits and she is not suicidal.
Julie, 32, a resident of the upper Midwest, dreads the onset of winter. Each year for the past three years, Julie has felt extremely lethargic and unable to concentrate during the fall and winter months. She usually gains close to 15 pounds during a winter season. She is not surprised by this weight gain, as she typically craves donuts and pastries during this time of the year. Julie lacks interest in most activities over the winter and spends a great deal of time in bed. During the spring and summer, Julie craves fresh fruit and salads, enjoys hiking, and feels like a different person.
Debra, 50, works in an office building. Last summer, the air-conditioning system malfunctioned for several weeks. Due to the resulting high humidity, mold began to grow on the interior walls of the offices. Although she doesn’t smoke and has never suffered from respiratory problems before, Debra began exhibiting symptoms of asthma. After she received limited relief from inhaled medications, her physician prescribed a four-week course of oral corticosteroids. During the first two weeks of this treatment (which seemed to relieve her breathing problems), Debra began to have trouble sleeping and felt depressed. When at work, Debra has trouble concentrating. She finds herself feeling irritable with coworkers for reasons she would have previously considered to be trivial. One day, when asked an innocuous question about a report she had prepared, she burst into tears. Debra wonders if her mother’s horror stories about mood shifts during menopause possibly could be true.
Ron, 39, has seemed very sad for over a month. When he is alone, he sometimes cries. He experiences so much trouble concentrating he cannot follow the plot of his favorite half-hour television comedy show. Some nights, Ron thinks about death because he feels guilty for being alive. His wife died of cancer six weeks ago and he wonders why he didn’t die instead.
Many people would agree that Ron appears to be depressed but, perhaps surprisingly, of the individuals just described, Ron is the only one who may not qualify for a mood disorder diagnosis.1
Classification Of Mood Disorders
According to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR; American Psychiatric Association, 2000), all mood disorders involve an altered or pathological mood state. Perhaps the most well-known mood disorders are the depressive disorders, which include major depressive disorder, dysthymic disorder, and depressive disorder not otherwise specified. These disorders involve only depression or dysthymic symptomatology; hence, the term unipolar depression is frequently used to denote these disorders. In contrast, the bipolar disorders include bipolar I disorder, bipolar II disorder, cyclothymic disorder, and bipolar disorder not otherwise specified. These disorders involve both depression and mania or hypomania. Finally, DSM-IV-TR includes two other mood disorders that are classified according to presumed etiology. These disorders are mood disorder due to a general medical condition and substance-induced mood disorder.
Major Depressive Disorder
Major depressive disorder (MDD) is diagnosed when at least one major depressive episode can be documented. According to DSM-IV-TR (APA, 2000), episodes of major depression are characterized by, for two or more weeks, the presence of at least five out of nine specified symptoms. Although variability is permitted in how the minimum criteria are met, one of two cardinal symptoms must be present.
The first cardinal symptom is dysphoric mood. In most cases, this altered mood state presents as persistent dysthymia (depression) although irritability may be observed, particularly in children and adolescents. The second cardinal symptom is anhedonia, or an omnipresent lack of interest in or ability to experience pleasure in normally pleasurable activities. The remaining seven diagnostic criteria encompass symptoms considered to be vegetative (hypersomnia or insomnia, unintended weight gain or loss, and fatigue), symptoms considered to be cognitive (difficulty concentrating or an inability to make decisions), and symptoms typically thought of as emotional (feelings of worthlessness, excessive guilt, and suicidal thoughts). Furthermore, a diagnosis of MDD is appropriate only if the just mentioned symptoms cannot be better accounted for by a psychotic disorder diagnosis such as schizophrenia or schizoaffective disorder. Finally, a diagnosis of MDD cannot be made if the individual’s history suggests there has ever been a manic or hypomanic episode.
Specifiers may be attached to a diagnosis of MDD to provide supplementary information about the current episode. For example, DSM-IV-TR (APA, 2000) provides criterion sets for catatonic features specifier, melancholic features specifier, and postpartum onset specifier. In addition, specifiers that describe the course of recurrent episodes, such as Seasonal Pattern Specifier, are available. Taken together, the use of these specifier sets is intended to facilitate treatment selection and to increase the predictive validity of the diagnostic categories.
Dysthymic Disorder
Dysthymic disorder (dysthymia) is a chronic form of depression. According to DSM-IV-TR (APA, 2000), to be considered chronic, a depressed mood must be present, more days than not, for at least two years. (Again, this mood may be irritable, rather than depressed, in children and adolescents.) During this same two-year period, at least two of the following must be present: lack of appetite or overeating, hypersomnia or insomnia, lack of energy, low self-esteem, trouble concentrating, and hopelessness. Although these symptoms must cause significant impairment or distress if the diagnosis is to be assigned, the symptoms cannot rise to the level of major depressive disorder, at least during the initial two-year period of mood disturbance required for the diagnosis of dysthymic disorder. A major depressive episode may be superimposed on an existing dysthymic disorder. Keller and Shapiro (1982) coined the term double depression to describe this condition.
Depressive Disorder Not Otherwise Specified
This diagnostic category is reserved for those cases in which significant depressive symptoms are present but the full symptom pattern does not meet the required criteria for mood disorder due to a general medical condition and substance-induced mood disorder, or for any other specific Axis I disorder.
Bipolar I Disorder
Bipolar I disorder is diagnosed when there is evidence of one or more manic episodes or mixed episodes (APA, 2000). A manic episode involves an abnormal change in mood that lasts at least one week. This mood may be elevated, expansive, or irritable. In addition, at least three of nine other symptoms must be present. These additional symptoms include inflated self-esteem, decreased need for sleep, pressured speech, flight of ideas, distractibility, psychomotor agitation, and uncharacteristic and excessive involvement in reckless activities. A mixed episode is diagnosed if, during a week’s time, the criteria for both a manic episode and a major depressive episode are met.
Typically, an individual diagnosed with bipolar I disorder will have experienced a previous episode of major depression. The diagnosis can be made, however, in the absence of evidence of depression, as it is expected that any individual who exhibits mania eventually will develop depression during the course of the disorder.
Similar to those provided for use when diagnosing major depressive disorder, descriptive feature and course specifiers may be attached to a diagnosis of bipolar I disorder to provide supplemental information. In addition, the specifier, with rapid cycling, can be appended to either a bipolar I or a bipolar II disorder diagnosis. Professionals use this specifier when the individual has experienced four or more episodes of abnormal mood during the past 12 months. Rapid-cycling may influence the choice of pharmacological interventions (Suppes, Dennehy, & Gibbons, 2000) and is usually indicative of a poorer prognosis.
Bipolar II Disorder
Bipolar II disorder is diagnosed when there is evidence of one or more major depressive episodes accompanied by at least one hypomanic episode. Hypomania is a less severe form of Mania. (The prefix hypo signifies “below,” so the word hypomania means “below mania.”) Although hypomania is not as extreme as mania, it represents an abnormally elevated mood state, nevertheless. The diagnostic criteria for a hypomanic episode indicate that the abnormal mood must persist throughout the day for at least four days. In addition, at least three of nine other symptoms must be present. These latter symptoms are the same as those used to determine the presence of a manic episode.
Cyclothymic Disorder
Cyclothymic disorder (cyclothymia) is a chronic disorder that involves bouts of hypomanic symptoms alternating with bouts of depressive symptoms. Although these symptoms must cause the individual to experience significant impairment or distress for the diagnosis to be warranted, the severity or pervasiveness of the symptoms must not rise to the level of those seen in either bipolar I disorder or bipolar II disorder.
Bipolar Disorder Not Otherwise Specified
This diagnostic category is reserved for those cases in which significant bipolar symptoms are present but the full symptom pattern does not meet the criteria for bipolar I disorder, bipolar II disorder, cyclothymic disorder, or any other specific Axis I disorder.
Mood Disorder Due to a General Medical Condition
This diagnosis is assigned only when there is strong evidence that a particular, identifiable general medical condition acted as a physiological precipitant for the pathological mood state. Hypothyroidism is an example of a general medical condition that may precipitate depression, whereas manic states may be precipitated by hyperthyroidism.
Substance-Induced Mood Disorder
This diagnosis is assigned only when there is strong evidence that use of a particular, identifiable substance precipitated the pathological mood state. Examples of drugs that may precipitate depression include corticosteroids and reserpine. Antidepressant drugs may precipitate mania, particularly in individuals at risk for the development of bipolar disorders (Mitchell et al., 2001).
Prevalence Of Mood Disorders
Depression has been labeled the “common cold” of psychopathology. Although this characterization overstates its occurrence (and its detrimental effects), major depressive disorder (MDD) is one of the more common psychiatric dis-orders. Kessler and colleagues (2005) report that 16.4 percent of the people in the United States meet the criteria for MDD at some point during their lives. Further, approximately 2.5 percent will meet the criteria for dysthymic disorder during their lives. MDD occurs approximately twice as often in women as in men. Kessler et al. report that during the latter half of the 20th century, the average age of onset decreased. At the present time, the median age of onset is in the early 20s, although MDD can occur at any age.
The bipolar disorders are much less prevalent than the depressive disorders. Kessler et al. (2005) estimate that 4 percent of the population will meet the criteria for either bipolar I or bipolar II during their lives. Another 4 percent will meet the criteria for cyclothymic disorder. The bipolar disorders occur equally often in men and women, with a median age of onset in the 20s. Bipolar symptoms that occur for the first time much later in life are likely due to a general medical condition.
Cultural Factors
The prevalence of mood disorders varies cross-culturally. In the past, it has been difficult to make global comparisons because different diagnostic criteria have been operational in different parts of the world. In an attempt to correct this problem, Weissman and colleagues (1996) carried out a large-scale, cross-cultural study utilizing standard diagnostic criteria. For MDD, the lowest prevalence was found in Taiwan (1.5 percent) and the highest prevalence in Beirut (19 percent). Other studies have suggested that the particular symptom pattern displayed by clients may be moderated by culture. For example, Kleinman (2004) revealed that the symptom pattern displayed by depressed Asian clients is more likely to include an abundance of somatic symptoms. Thus, it is a bit difficult to interpret the results of the data gathered by Weissman et al. Certainly, future research investigating cultural factors is warranted.
Differential Diagnosis
Accurate diagnosis of mood disorders is critical for treatment success. A complete discussion of differential diagnosis is beyond the scope of this research-paper, although one key issue should be mentioned. Because the treatment options for MDD (unipolar depression) typically differ from those utilized during the depressive phase of bipolar disorders, it is crucial that the clinician assess depressive episodes carefully. Table 83.1 presents some of the differences frequently observed between unipolar and bipolar depression. In addition, as noted above, MDD is not diagnosed if there has ever been a manic or a hypomanic episode. Thus, it is important to question clients carefully about past experiences. If a client is unable to supply reliable information, family members and/or medical records may provide needed historical data. Ghaemi (2001) suggested the mneumonic DIGFAST to aid the clinician in assessment of manic and hypomanic symptoms: distractibility, insomnia, grandiosity, /light of ideas, activities, speech, thoughtlessness.
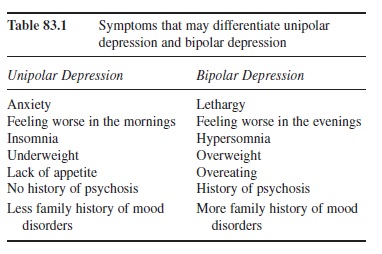 Table 83.1 Symptoms that may differentiate unipolar depression and bipolar depression
Table 83.1 Symptoms that may differentiate unipolar depression and bipolar depression
Etiology Of Mood Disorders
Theories about the etiology, or cause, of mental disorders have been put forth for centuries. In this section, historical ideas as well as current formulations regarding the etiology of mood disorders will be discussed. For the sake of clarity, biological and psychological theories regarding causality are delineated in separate sections. It is important to note, however, that in reality, biological and psychological functioning cannot be so neatly partitioned.
Biological Theories
Hippocrates, often called the father of modern medicine, is credited with suggesting that mental disorders have physical causes. During the time that Hippocrates lived, the fifth century BCE, mental and physical illnesses typically were viewed as punishments from the gods. Hippocrates broke with this predominant, psychogenic tradition, and proposed instead that the root cause of these illnesses was in the physical body. More specifically, he posited that imbalances in four humours, or bodily fluids, were to blame for various mental illnesses and personality alterations. Melancholia, a form of depression, was hypothesized to result from an excess of black bile. Although Hippocrates’ precise ideas did not stand up to scientific scrutiny, his notion that mood alterations may result from imbalances in the body portends aspects of contemporary thought.
Modern biological theories regarding the etiology of mood disorders may be classified into two broad divisions—those with a genetics focus and those with a neuroscience focus. These divisions are somewhat artificial but are used here for the sake of simplicity.
Genetics
Researchers have investigated the theory that genes play a role in the development of mood disorders through the use of the family method, the twin method, and the adoptee method. For example, in the family method, the first step is to identify individuals with the disorder in question. These are called index cases or probands.
Because the degree to which genes are shared by the biologic relatives is known, the contribution of genes in the development of a disorder can be estimated through the use of this method. If a disorder occurs more frequently in first-degree relatives of a proband than in second-degree relatives, this suggests that the disorder has a genetic component. One caveat must be mentioned here: In addition to sharing more genes, first-degree relatives also are more likely than second-degree relatives to share a common environment. Thus, a higher rate of disorder in first-degree relatives could be attributable, at least in part, to environmental factors.
The results of family studies, twin studies, and adoption studies suggest that bipolar disorders have a much stronger genetic component than do depressive disorders. These results have been replicated across a number of studies.
Researchers also have used linkage analysis to study the contribution that genes may make to the development of a disorder. With this method, investigators collect blood samples from families in which the specific disorder is known to occur. Gene markers (inheritance patterns for known characteristics) are identified, and any similarities in the inheritance patterns of the known characteristic and the disorder under investigation are identified. In this manner, it may be possible to identify the chromosome(s) that carry the gene or genes related to the studied disorder. In 1987, linkage analysis using the Amish as research subjects reported the identification of a gene marker for bipolar I disorder on chromosome 11 (Egeland et al., 1987). Although this study generated great excitement when it was published, several studies have failed to replicate this finding. Given the heterogeneity of mood disorder symptoms, most researchers believe that multiple genes are likely to be implicated versus a solitary gene.
Neuroscience
The neuroscience perspective assumes that mood disorders are due to abnormal brain processes. The two primary lines of research have investigated neurotransmitter abnormalities and brain structure and function abnormalities.
Neurotransmitters are chemicals that allow neurons (single nerve cells) to communicate with one another. The three neurotransmitters that have received the most empirical attention in the study of mood disorders are serotonin, norepinephrine, and dopamine. Early studies of the role of neurotransmitters in mood disorders suggested that depression was caused by a deficit of key neurotransmitters, whereas mania was caused by an excess of these neurotransmitters. More recent studies have suggested that these ideas are overly simplistic and have focused instead on possible abnormalities in the receptor sites. In persons prone to the development of mania, receptor sites may be too numerous or too easily excited. In addition, research has begun to examine the role of second messengers (neurotransmitters are now known as first messengers) in psychopathology. Second messengers are intracellular chemicals that are thought to play a role in adjusting the sensitivity of receptor sites. The two second-messenger systems thought to be relevant to the bipolar disorders are the cyclic adenosine monophosphate system and the phosphoinositode system (Manji & Lenox, 2000).
The notion that structural and functional abnormalities in the brain may play a role in the development of mood disorders has begun to receive empirical attention. Advancements in imaging techniques such as the development of magnetic resonance imaging (MRI) allow researchers to examine brain structures at a level of detail that previously could be accomplished only at autopsy. Perhaps more important, techniques that allow functional aspects to be evaluated (fMRI, PET scans) have been developed.
Studies of brain structure have revealed that longstanding major depressive disorder (MDD, recurrent,) may be associated with smaller hippocampal regions and diminished volume in the prefrontal cortex area (Sheline, 2000). The hippocampus is thought to play a critical role in the consolidation of long-term memories whereas the prefrontal cortex is involved in planning, decision making, and motivation.
Functional studies have demonstrated that people with MDD show excess activation in the amygdala when shown sad or angry faces (Sheline et al., 2001). The amygdala is thought to play a role in the processing of emotional stimuli and in the storage of emotionally tinged memories. Interestingly, this abnormal response abates after treatment for depression.
Psychological Theories
The early Greeks were not alone in attributing the cause of mental disorders to supernatural beings. Written records from the Egyptians, the Babylonians, and the Chinese document a prevailing belief in demonology, or the belief that an evil being or spirit can inhabit a person’s body and control his/her mind and behavior. In the New Testament, the book of Mark (Chapter 5) relates that Jesus exorcised demons and then cast them into a herd of swine, effectively curing a man of his illness. Although Hippocrates (and later Galen) attempted to separate medicine from magic, religion, and superstition, after the influence of Greco-Roman thought waned in Europe, there was a widespread return to demonology as the predominant view. During the time known as the Dark Ages and continuing through the Middle Ages, hope for a cure from mental illness was the province of the church.
Beginning in the 18th century, a number of psychological frameworks emerged to explain mental illnesses. Sigmund Freud’s ideas are of particular relevance to depression. In his seminal paper, “Mourning and Melancholia” (1917/1961a), Freud contrasted the clinical picture of melancholia (depression) with that of normal grief. More specifically, Freud noted that although these states may involve superficial similarities, anger, a natural part of the grieving process, is typically directed outward toward the lost love object, whereas in depression, this negative affect is directed inward toward the self. Based on his clinical observations, Freud further noted that self-blame and self-recrimination are central characteristics of depression but not of mourning.
According to Freud’s formulation, the loss of the mother or the loss of the mother’s love may render a young child more vulnerable to the development of depression in adulthood. If the child is unable to find an acceptable mother substitute, Freud hypothesized that the young child will create a representation of the lost object within him- or herself. As the child mourns the loss of the mother object, the normal ambivalence and anger toward the object are no longer directed outward, as in normal grief, but rather are directed inward toward the introjected object. Because the introjected object has become fused with the child’s own ego, or sense of self, these feelings of ambivalence and anger become directed toward the self. Moreover, given this psychic foundation, significant losses suffered in adulthood elicit the same sort of self-directed anger. In this fashion, Freud elegantly explains the prolonged self-blame and self-recrimination observed during depressive episodes that arise following a real or symbolic loss. Although Freud recanted aspects of this formulation in his subsequent work (1923/1961b, 1933/1961c), these ideas continued to exert a powerful influence on the practice of psychiatry for over a half century (Bemporad, 1985).
Aaron Beck, a psychiatrist, initially was taken with Freud’s ideas vis-à-vis retroflected anger and depression. Beck reasoned that, if these ideas were indeed correct, the dreams of depressed patients should exhibit themes of anger and hostility. In an early study, Beck (1961) examined the dream content reported by depressed patients. To his surprise, on the dimension of hostility and anger, the dream content reported by depressed persons did not differ from that reported by normal controls. However, Beck noted that the dream content reported by the depressed group did differ in one important regard; namely, the depressed patients’ dreams were replete with themes related to deprivation, punishment, and exclusion. Using the psychoanalytic technique of free association, Beck continued to probe the thought processes and feelings of his depressed patients. Through this work, Beck (1963) came to the realization that although specific thought content differed across his depressed patients, the commonalities were striking. Themes of loss and deprivation were pervasive; his depressed patients seemed universally to view the world, the self, and the future in an unrealistically negative light. He further observed that his patients were likely to find evidence to support their biased views given their apparent biases in cognitive processing. For example, Beck noted that depressed individuals were likely to engage in selective abstraction. In selective abstraction, one small negative detail in a situation receives undue attention, which causes the entire situation to be perceived in a negative light.
Drawing on these rich clinical examples, Beck published a diathesis-stress model to explain the etiology of depression in 1967. Like Freud, Beck asserted that childhood experiences could render an individual vulnerable to the development of depression later in life. Beck proposed that an early experience such as parental loss could lead to the development of negatively biased self-referent ideas or schemas. He termed these negatively valenced ideas about the self, the world, and the future the negative cognitive triad. His ideas make intuitive sense if we recall the ego-centricity of young children, as well as their tendency to engage in magical thinking. A young child who says to his sister during a momentary bout of anger, “I hate you and wish you’d go away,” is likely to believe he caused her death if she should happen to die.
Beck proposed that these negative schemas are latent until they are activated by a relevant event such as the loss of a psychologically important relationship in adulthood. Thus, like Freud, Beck traces the diathesis of depression to childhood, and, like Freud, Beck proposes that the stress occurs in adulthood. Beck’s ideas differ from Freud’s in that he does not consider parental loss to be the only possible trigger for the formation of negatively biased depressogenic schemas. For example, a child who feels that she cannot live up to the high standards set by her parents may develop negative schemas. These schemas would not be activated in adulthood by an interpersonal loss but could be activated by an event involving achievement failure, such as a job loss.
Once negative schemas are activated, they serve to guide the screening, encoding, and organization of incoming information. Because negatively biased information about the self, the world, and the future is consistent with the pre-vailing cognitive set, this information receives differential attention and more elaborative encoding. Consequently, this information is memorialized more readily.
Beck also asserted that depressed persons maintain their cognitive set or negatively toned schemas through the systematic use of particular cognitive processing biases. Although a full discussion of these processing errors is beyond the scope of this research-paper, a few noteworthy examples must be mentioned. As previously discussed, Beck noted that depressed individuals tend to engage in selective abstraction. Beck further hypothesized that depressed persons make arbitrary inferences—that is, they tend to draw conclusions in the face of insufficient evidence. Finally, Beck posited that depressed persons tend to engage in overgeneralization—that is, they are apt to base general rules or conclusions on solitary incidents. Taken together, these processing errors lead depressed individuals to see themselves, the world, and the future in negative, absolute, judgmental, and overly simplistic terms. Such views tend to maintain and exacerbate the depressive symptoms.
Shortly after Beck published his theory about the origins of depression, another significant theory was put forth by Seligman (1974). At the core of Seligman’s original model was the notion of learned helplessness. Seligman and his colleagues demonstrated that dogs subjected to inescapable shock evidenced lingering motivational, behavioral, and emotional deficits. More specifically, after being shocked while immobilized in a Pavlovian harness, dogs made no effort to escape painful shocks when placed in a shuttlebox the next day, even though escape was now easily attainable. When in the shuttlebox, the dogs behaved passively and “looked depressed.” Seligman and his colleagues hypothesized these dogs had learned that outcomes and their responses were noncontingent. In the initial shock condition involving the Pavlovian harness, the dogs were, indeed, helpless to escape the shock. The outcome (shock) was not contingent upon their responses (whimpering, howling, squirming in the harness, etc.). However, when the situation changed (the shuttlebox condition) and escape was possible, the dogs did not alter their behavior to match the new situation. In essence, they had learned to be helpless.
Seligman and his colleagues proposed that a similar mechanism may operate in depression. Under normal circumstances, when faced with an aversive event, a person will engage in escape responses or in responses intended to preclude the occurrence of the event. For example, in the case of an impending unwanted romantic breakup, a partner may plead, avoid conversations about the relationship, make promises, give gifts, and so forth to try to forestall the breakup. If the person is unable to avert the breakup through these various actions, he or she may come to believe that life events and his or her responses are independent of one another. In other words, the individual may learn to be helpless.
Seligman’s conceptualization meshes well with many observed features of depression and may make intuitive sense to anyone who has known a depressed family member, roommate, or friend. Although we may feel guilty for feeling this way, it can be frustrating to be in close contact with people who are depressed because of their apparent lack of motivation and unwillingness to engage in even the simplest of activities. However, Seligman’s ideas do not mesh with all observed aspects of depression. For example, as previously discussed, self-blame is a hallmark of depression. Abramson and Sackheim (1977) point out the paradox here—why would depressives engage in self-blame if they feel they have no control over outcomes, as the learned helplessness model proposes? Abramson, Seligman, and Teasdale (1978) revised the model to take cognitions into account.
The reformulated model, known as the attributional model, highlights the kinds of causal explanations people create for positive and negative events. These attributions or explanations can be classified on three independent dimensions. An attribution can be classified as internal (personal) versus external (environmental), stable (permanent) versus unstable (temporary), and global (related to many life areas) versus specific (related to one life area or situation). To understand how these three dimensions apply to real-life situations, let’s imagine what sort of explanations three students might generate for their poor performance on a midterm exam. Carol tells herself she performed poorly because the professor graded unfairly (external). She decides that the final exam will be graded differently because students complained vociferously about the grading when the professor returned the midterm exams (unstable). Finally, Carol remembers she doesn’t have to take any more courses from this professor (specific). Thus, Carol has made an external, unstable, and specific attribution for her poor academic performance. On the other hand, Tom tells himself he failed the exam because he didn’t study (internal) and that although he failed all of his midterm exams (global), he’s now working fewer hours at his job so he can catch up on his studying before the final exams (unstable). Tom has made an internal, global, and unstable attribution for his failure. Finally, Laura believes that she failed the exam because she doesn’t understand the material (internal), that she’s unlikely to understand the material any better in the future (stable), and that her poor performance indicates she probably doesn’t belong in college (global). Laura has made an internal, stable, and global attribution for her academic failure. This model suggests that people who make internal, global, and stable attributions for negative outcomes (like Laura) are more likely to become depressed.
Although the attributional model generated a great deal of research, contradictory findings led to a final revision of the model in 1989 (Abramson, Metalsky, & Alloy). This revision, termed the hopelessness model, posits that cognitive processes and attributional style may predict a subtype of depression, coined hopelessness depression. In this final formulation, it is proposed that hopelessness, whether arising from one’s habitual attributional style or from other factors such as low self-esteem, leads to the development of depression.
Psychological theories that explain mania are relatively scarce. One perspective suggests that mania arises as a defense against an aversive psychological state, such as underlying low self-esteem. One intriguing study (Winters & Neale, 1985) provides support for this hypothesis. In this study, normal control participants, participants with bipolar disorder in remission, and participants with unipolar disorder in remission were asked to complete a number of paper-and-pencil questionnaires designed to assess self-esteem. Some of the measures used were face valid—that is, the explicit content of the items made it apparent that self-esteem issues were being assessed. On these more obvious measures of self-esteem, the unipolar group scored significantly lower than did the bipolar group, which did not differ, from the normal control group. However, an indirect assessment of self-esteem was also included in the study. Participants were presented with hypothetical situations and required to draw inferences about the situations. The types of inferences drawn provided an indirect measure of self-esteem and self-worth. On this latter task, the bipolar group’s performance did not differ from that of the unipolar group. Taken together, these results suggest that individuals with bipolar disorder may have negative self-views that are not apparent when measured explicitly.
Treatment Interventions For Mood Disorders
Treatment interventions may be characterized as psychological interventions or biologic interventions.
Psychological Interventions
Numerous studies have demonstrated the efficacy of psychological interventions in the treatment of depression. Cognitive-behavioral therapy (CBT) is particularly effective in this regard.
The basic premise of CBT flows logically from Beck’s model of depression. Recall that Beck proposed that depression is characterized by the activation of negatively toned schemas. These schemas are maintained by systematic cognitive errors, such as selective abstraction and overgeneneralization. In essence, the client’s thinking style is causing her pathological mood state. Through a variety of techniques, CBT works to alter these maladaptive thinking patterns. Beck also includes a behavioral component in his therapeutic intervention. This component, known as behavioral activation (BA), involves structured activities designed to provide the depressed person with successful experiences. Recent studies have targeted only the BA component of Beck’s therapy. Results suggest that BA therapy may be effective in treating depression in the absence of the full CBT regimen.
Interpersonal psychotherapy (IPT) also is effective in the treatment of depression. This approach, which developed out of the psychoanalytic model, has at its heart the depressed person’s interpersonal needs. Unlike traditional psychoanalytic therapy, IPT is designed to be time-limited. Further, rather than focusing on repressed material from early life, IPT targets the client’s current life situation. Studies have shown IPT to be effective for MDD in a wide variety of client groups.
As is discussed in the section describing biological interventions, the bipolar disorders are typically treated with medication. Recently, however, intervention studies have examined the possibility that family therapy and marital therapy may be useful adjuncts in the treatment of bipolar disorders. Similar to the findings reported for schizophrenic individuals and their families, family conflict and high levels of expressed emotion exacerbate the symptoms of bipolar disorders. In a number of studies, Miklowitz and colleagues (2000) demonstrated the efficacy of a family-based program in preventing the recurrence of manic episodes. Interestingly, this effect was largely independent of medication compliance. Thus, the use of psychological interventions to aid in the treatment of bipolar disorders may increase.
Biologic Interventions
The first antidepressant drugs were introduced in the 1950s. During the last two decades, numerous antidepressant drugs have appeared on the market. Although drugs do not alleviate all the symptoms of depression for many individuals, drugs are often the first treatment option people encounter when seeking help for depression. Table 83.2 presents a sampling of the drug types currently used in the treatment of mood disorders.
As can be seen from Table 83.2, monoamine oxidase inhibitors (MAOIs), tricyclics, selective serotonin reuptake inhibitors (SSRIs), and atypical antidepressants are prescribed for the treatment of depression. Although the precise mode of action is not completely understood and probably differs across and within these drug classes, in general, antidepressant drugs are thought to increase the availability of key neurotransmitters at the neuronal synapse. Researchers also have proposed additional mechanisms of action, such as secondary messengers.
As their name indicates, MAOIs act to inhibit an enzyme known as monoamine oxidase. (The suffixes indicates the substance is an enzyme.) This enzyme normally functions in the synaptic gap to selectively break down surplus neurotransmitter belonging to a class denoted as mon-amines. If the normal breakdown can be delayed, thereby keeping active neurotransmitter in the synaptic gap for a longer time, a given amount of neurotransmitter will have a greater impact on the postsynaptic neuron.
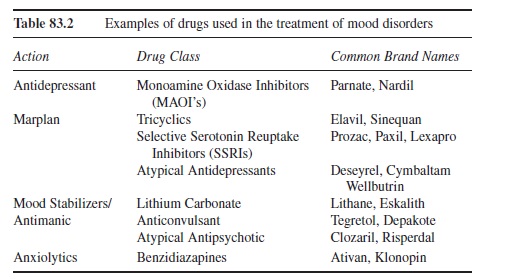 Table 83.2 Examples of drugs used in the treatment of mood disorders
Table 83.2 Examples of drugs used in the treatment of mood disorders
MAOIs were one of the first drug types to show efficacy in the treatment of depression; however, these drugs can cause a hypertensive crisis (severe headache, soaring blood pressure, vomiting) if foods containing tyramine (e.g., aged cheese, red wine, Brussels sprouts, salami) are consumed. In addition, drugs that act on the sympathetic nervous system (e.g., cocaine, some decongestants) interact with MAOIs. Partly for these reasons, this class of drug is less likely than other classes of drugs to be prescribed today.
Bipolar disorders are typically treated with drugs. Lithium carbonate, a salt, was approved to treat mania in the 1970s. This mood stabilizer remains the predominant treatment, especially during early phases of the disorder. Unfortunately, research suggests that more than half of the patients treated with lithium will develop resistance to it within three years of treatment initiation (Nemeroff, 2000). In addition, up to 40 percent of patients treated with Lithium will show an inadequate initial treatment response (Tohen & Grundy, 1999). Finally, treatment with lithium requires careful management, as it has a narrow therapeutic-to-toxic dose ratio.
Anticonvulsants are also frequently used to stabilize mood when treating bipolar disorders, particularly when lithium has proved ineffective. Convulsions are not a symptom of the bipolar disorders, of course; however, the mood stabilizing properties of these drugs were discovered serendipitously during trials investigating their use in treating epilepsy. Anxiolytics (antianxiety drugs) may be used on a short-term basis to aid in the management of mania, although side effects preclude their long-term use.
All drugs have side effects, of course. A complete discussion of the side effects of drugs used to treat mood disorders is well beyond the scope of this research-paper. However, the propensity of antidepressant drugs, particularly the tricyclics, to trigger manic symptoms deserves mention. As discussed in the section on differential diagnosis, it is vital to distinguish between unipolar and bipolar depression, in part to avoid triggering manic symptoms during the treatment for depression. For a discussion of this issue as well as an excellent review of the literature evaluating pharmacologic interventions for the bipolar disorders, please see R. A. Rivas-Vazquez, Johnson, Rey, Blais, and A. Rivas-Vazquez (2002).
In the early 1990s, interest emerged in treating depression with an herbal remedy, St. John’s wort (Hypericum perforatum). Anecdotal reports suggested that St. John’s wort effectively alleviates depression, a contention that was upheld by an early study (Linde et al., 1996). More recently, however, in a well-controlled randomized trial, St. John’s wort was shown to have no effect in the treatment of moderate depression (Hypericum Depression Trial Study Group, 2002). To complicate matters further, because herbal supplements are not considered drugs, their manufacture is not tightly regulated. Therefore, potency of an herbal preparation may vary widely within and across manufacturing lots. Finally, because herbal remedies cannot be patented, pharmaceutical companies have been reluctant to devote significant resources to investigating their efficacy. Unfortunately, this reluctance, although understandable, may serve to limit our knowledge of alternative therapies.
All biological treatments for mood disorders are not pharmacological in nature. For example, electroconvulsive therapy (ECT) is used frequently to treat severe depression. This intervention, known colloquially as “shock therapy,” was introduced in the 1930s by two Italian scientists, Cerletti and Bini. The first patient Cerletti and Bini treated was suffering from “incoherent schizophrenia.” After receiving multiple ECT treatments, the man purportedly was able to work and to live a normal life. The notion that electrically induced convulsions served a therapeutic function gained rapid acceptance in the field.
Early treatment with ECT was brutal. Strong seizures frequently resulted in broken bones, and significant retrograde memory losses following treatment were not uncommon. The public’s trust in ECT as a viable treatment option was eroded further by its negative portrayal in the popular 1975 movie, One Flew Over the Cuckoo’s Nest. Moreover, for many years, ECT was used to treat a broad spectrum of mental illnesses in the absence of scientific evidence demonstrating its utility for these diverse illnesses.
The application of ECT today bears little resemblance to earlier practices. Current practice is strictly governed by guidelines put forth by the American Psychiatric Association (2001). For example, administration of general anesthesia precludes the patient from experiencing pain during the procedure. Additionally, the routine use of muscle relaxants prevents broken bones. Although the seizure activity elicited by the electrical current is observed on an electroencephalogram (EEG) during the procedure, no outward convulsion occurs. Memory problems are also minimized—but not totally avoided—by current practices.
Although it is not known precisely how ECT exerts its beneficial effect, empirical evidence suggests that ECT may be the best biological treatment available for severe depression and for refractory depression. ECT acts more rapidly than medication or psychotherapeutic interventions, so its use may be indicated in the face of extreme suicidality. Finally, ECT may be the treatment of choice for individuals for whom the use of antidepressant medication would be especially risky. (Many antidepressant medications exert cardiovascular effects.)
Despite dramatic improvements in the side-effects panel for ECT, concerns about treatment-induced memory problems have continued to surface. Some patients report lingering short-term memory deficits for weeks or even months after the procedure, although it is important to keep in mind that memory and concentration difficulties are, in and of themselves, symptoms of MDD. Consequently, it is possible that these reported cognitive deficits merely represent residual aspects of the original disease process versus an iatrogenic symptom. Nevertheless, an alternative manner of inducing therapeutic seizures has received increased empirical attention over the last decade.
Magnetic seizure therapy (MST) employs rapidly alternating strong magnetic fields to induce a therapeutic convulsion. MST offers more precise control over activation of the seizure, such that areas of the brain especially critical for memory may be spared (Lisanby, Luber, Schpaepter, & Sackheim, 2003). An intriguing study conducted by Moscrip, Terrace, Sackheim, and Lisanby (2006) suggests that MST may indeed offer a memory-sparing advantage over ECT. Using a within-subjects crossover design, Rhesus monkeys were given daily electroconvulsive shock (ECS), MST, and sham (anesthesia-only) interventions in five-week blocks. Prior to receiving each intervention, the animals were trained on learning and memory tasks. Results indicated that memory for previously learned material was poorer in the ECS condition compared to both the sham and the MST condition. Further, the time required to complete the memory tasks was longest following ECS, whereas time to task completion did not differ between the sham condition and the MST condition. Given these results, more work to investigate the effectiveness of this treatment in alleviating depression is sorely needed.
Summary
This research-paper provided an overview of our knowledge of mood disorders. As we move farther into the 21st century, it is likely that our knowledge of the etiology and treatment of these disorders will increase exponentially. Newer technologies such as fMRIs now allow living, functioning human brains to be studied in great detail. The Human Genome Project, now complete, will likely provide invaluable data for studying the contributions genes make to many forms of illness. As we increase our understanding of the biology of mood disorders, the importance of psychosocial factors should not be ignored. It remains a challenge for us truly to integrate research on the mind with research on the body.
References:
- Abramson, L. Y., Metalsky, G. I., & Alloy, L. B. (1989). Hopelessness depression: A theory-based subtype of depression. Psychological Review, 96, 358-372.
- Abramson, L. Y., & Sackheim, H. A. (1977). A paradox in depression: Uncontrollability and self-blame. Psychological Bulletin, 84, 835-851.
- Abramson, L. Y., Seligman, M. E. P., & Teasdale, J. D. (1978). Learned helplessness in humans: A critique and reformulation. Journal of Abnormal Psychology, 87, 49-74.
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., Rev. ed.). Washington, DC: Author.
- American Psychiatric Association. (2001). The practice of ECT: Recommendations for treatment, training, and privileging. Washington, DC: Author.
- Beck, A. T. (1961). A systematic investigation of depression. Comprehensive Psychiatry, 2, 163-170.
- Beck, A. T. (1963). Thinking and depression: 1. Idiosyncratic content and cognitive distortions. Archives of General Psychiatry, 9, 324-333.
- Beck, A. T. (1967). Depression: Clinical, experimental, and theoretical aspects. New York: Harper & Row.
- Beck, A. T., Rush, A. J., Shaw, B. F., & Emery, G. (1979). Cognitive therapy of depression. New York: Guilford Press.
- Bemporad, J. R. (1985). Long-term analytic treatment in depression. In E. E. Beckham & W. R. Leber (Eds.), Handbook of depression: Treatment, assessment, and research. Homewood, IL: Dorsey.
- Calabrese, J. R., Shelton, M. D., Bowden, C. L., Rapport, D. J., Suppes, T., & Shirley, E. R. (2001). Bipolar rapid cycling: Focus on depression as its hallmark. Journal of Clinical Psychiatry, 62, Suppl. 1434-1441.
- Egeland, J. A., Gerhard, D. S., Pauls, D. L., Sussex, J. N., Kidd, K. K., Alien, C. R., et al. (1987). Bipolar affective disorders linked to DNA markers on chromosome 11. Nature, 325, 783-787.
- Freud, S. (1961a). Mourning and Melancholia. In J. Strachey (Ed. and Trans.), The standard edition of the complete psychological works of Sigmund Freud (Vol. 14). London: Hogarth. (Original work published 1917)
- Freud, S. (1961b). The ego and the id. In J. Strachey (Ed. and Trans.), The standard edition of the complete psychological works of Sigmund Freud (Vol. 19). London: Hogarth. (Original work published 1923)
- Freud, S. (1961c). New introductory lectures on psychoanalysis. In J. Strachey (Ed. and Trans.), The standard edition of the complete psychological works of Sigmund Freud (Vol. 22). London: Hogarth. (Original work published 1933)
- Ghaemi, S. N. (2001). Bipolar disorder and antidepressants: An ongoing controversy. Primary Psychiatry, 8, 28-34.
- Ghaemi, S. N., Lenox, M. S., & Baldessarini, R. J. (2001). Effectiveness and safety of long-term antidepressant treatment in bipolar disorder. Journal of Clinical Psychiatry, 62, 565-569.
- Hypericum Depression Trial Study Group. (2002). Effect of Hypericum perforatum (St. John’s wort) in major depressive disorder: A randomized, controlled trial. Journal of the American Medical Association, 287, 1807-1814.
- Johnson, M. H., & Magaro, P. A. (1987). Effects of mood and severity on memory processes in depression and mania. Psychological Bulletin, 101, 28-10.
- Keller, M. B., & Shapiro, R. W. (1982). “Double-depression”: Superimposition of acute depressive episodes on chronic depressive disorders. American Journal of Psychiatry, 139, 438-442.
- Kessler, R. C., Chiu, W. T., Demler, O., & Walters, E. E. (2005). Prevalence, severity, and co-morbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 617-627. Kleinman, A. (2004). Culture and depression. New England Journal of Medicine, 351, 951-953.
- Linde, K., Ramirez, G., Mulrow, C. D., Pauls, A., Weidenhammer, W., & Melchart, B. B. (1996). St. John’s wort for depression—An overview and meta-analysis of randomized clinical trials. British Medical Journal, 313, 253-358.
- Lisanby, S. H., Luber, B., Schpaepter, T. E., & Sackheim, H. A. (2003). Safety and feasibility of magnetic seizure therapy (MST) in major depression: Randomized within-subject comparison with electroconvulsive therapy. Neuropsychopharmacology, 28(10), 1852-1865.
- Manji, H. K., & Lenox, R. H. (2000). The nature of bipolar disorder. Journal of Clinical Psychiatry, 61, Suppl. 1342-1357.
- Marangell, L. B., Yudofsky, S. C., & Silver, J. M. (1999). Psychopharmacology and electroconvulsive therapy. In R. E. Hales, S. C. Yudofsky, & J. A. Talbott (Eds.), The American Psychiatric Press textbook of psychiatry (3rd ed., pp. 1025-1132). Washington, DC: American Psychiatric.
- Miklowitz, D. J., & Goldstein, M. J. (1997). Bipolar disorder: A family-focused treatment approach. New York: Guilford Press.
- Miklowitz, D. J., Simoneau, T. L., George, E. L., Richards, J. A., Kalbag, A., Sachs-Ericsson, N., et al. (2000). Family-focused treatment of bipolar disorder: One-year effects of a psychoeducational program in conjunction with pharmaco-therapy. Biological Psychiatry, 48, 582-592.
- Mitchell, P. B., Wilhelm, K., Parker, G., Austin, M. P., Rutgers, P., & Malhi, G. S. (2001). The clinical features of bipolar depression: A comparison with matched major depressive disorder patients. Journal of Clinical Psychiatry, 62, 212-216.
- Moscrip, T. D., Terrace, H. S., Sackheim, H. A., & Lisanby, S. H. (2006). Randomized controlled trial of the cognitive side effects of magnetic seizure therapy (MST) and electroconvulsive shock (ECS). International Journal of Neuropsychopharmacology, 9(1), 1-11.
- Nemeroff, C. B. (2000). An ever-increasing pharmacopoeia for the management of patients with bipolar disorder. Journal of Clinical Psychiatry, 61, Suppl. 1319-1325.
- Rivas-Vazquez, R. A., Johnson, S. L., Rey, G. J., Blais, M. A., & Rivas-Vazquez, A. (2002). Current treatments for bipolar disorder: A review and update for psychologists. Professional Psychology: Research and Practice, 33, 212-223.
- Seligman, M. E. P. (1974). Depression and learned helplessness. In R. J. Friedman & M. M. Katz (Eds.), The psychology of depression: Contemporary theory and research. Washington, DC: Winston-Wiley.
- Sheline, Y. I. (2000). 3D MRI studies of neuroanatomic changes in unipolar major depression. Biological Psychiatry, 48, 791-780.
- Sheline, Y., Barch, D., Donnelly, J. M., Ollinger, J. M., Snyder, A. Z., & Mintun, M. A. (2001). Increased amygdala response to masked emotional faces in depressed subjects resolves with antidepressant treatment: An fMRI study. Biological Psychiatry, 50, 651-658.
- Suppes, T., Dennehy, E. B., & Gibbons, E. W. (2000). The longitudinal course of bipolar disease. Journal of Clinical Psychiatry, 61, Suppl. 923-930.
- Tohen, M., & Grundy, S. (1999). Pharmacologic approaches for treatment-resistant mania. Psychiatric Annals, 28, 629-632.
- Weissman, M. M., Bland, R. C., Canino, C. J., Faravelli, C., Greenwald, S., et al. (1996). Cross-national epidemiology of major depression and bipolar disorder. JAMA, 276, 293-299.
- Winters, K. C., & Neale, J. M. (1985). Mania and low self-esteem. Journal of Abnormal Psychology, 94, 282-290.
- Woods, S. W. (2000). The economic burden of bipolar disease. Journal of Clinical Psychiatry, 61, Suppl. 1338-1341.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to order a custom research paper on any topic and get your high quality paper at affordable price.





