This sample Psychology of Eating Research Paper is published for educational and informational purposes only. Free research papers are not written by our writers, they are contributed by users, so we are not responsible for the content of this free sample paper. If you want to buy a high quality research paper on any topic at affordable price please use custom research paper writing services.
Abstract
Eating is a complex human behavior that is influenced by cultural, social, personality, and biological factors. Dieting, obesity, and overeating all are important social and health problems within applied psychology. The absence of demonstrably successful weight loss programs, as well as controversy over the supposed health benefits of weight loss in the long term, casts doubt on the popular notion that dieting makes people healthier.
Outline
- Introduction
- Cultural and Environmental Influences on Food Selection
- Social Influences on Eating Behavior
- The Role of Personality in Eating Behavior
- Set Point Model of Weight Regulation
- Obesity and the Problem of Eating Too Much
- Overcoming Obstacles to Weight Control
1. Introduction
One might think that a behavior so essential to our survival as eating would be fully explained through biology. It might seem that, like other essential behaviors such as sleeping and breathing, one could neatly explain the physiological mechanisms at work just before we put food into our mouths. However, decades of research into the biological mechanisms involved in eating have produced rather disappointing results. It seems that humans just do not do a very good job of eating in accordance with verifiable hunger and satiety cues. The biological perspective of eating posits that we should eat when our metabolic energy fuels are expended. However, one problem with this explanation of eating behavior is that humans often report feeling ‘‘hunger’’ despite ample energy stores in the form of body fat. Furthermore, most of us eat much more food than we require to remain alive. Another problem with the biological explanation of eating is that overall blood glucose levels (another index of metabolic energy) do not correspond well with reported hunger or (again) eating behavior. Finally, the hormone and neurotransmitter involvement in hunger and eating is especially complex and not yet completely understood, with several hormones potentially involved (e.g., leptin, insulin, ghrelin, cholecysokinin). Rather than being determined by iatrogenic biological markers, humans’ eating behavior seems to be largely determined by factors outside the individual. This research-paper examines the psychology of eating and attempts to answer the question of why we generally tend not to eat according to hunger and fullness. Culture and environment, sensory factors, social factors, and even personality can influence food choice and eating behavior, and all of these factors take us further away from eating according to our internal hunger and satiety cues. The article also examines the problems of eating too much and obesity as well as what applied psychology can tell us about the solutions to these complex health problems.
2. Cultural And Environmental Influences On Food Selection
In general, our diets are made up of what is readily available for us to eat. To a large extent, our culture decides for us the type of food we can eat as well as the portion sizes we consider to be normative. In brief, we tend to eat what is put in front of us. For instance, the North American diet, replete with an overabundance of saturated fats and larger portion sizes as compared with its international counterparts, can at least partially explain North America’s relatively high obesity rates. Experimental studies have confirmed that the more we are served, the more we eat.
Humans and animals alike experience food neophobia, that is, an intrinsic fear of trying new or novel foods. This fear is believed to serve a protective function in that it dissuades us from eating foods with which we are not familiar and that might not be safe. Factors that have been shown to increase food neophobia include knowledge that the food is of animal origin as well as trait and state anxiety. Factors that decrease our unwillingness to try new foods include modeling by others trying the new food, information about the nutritional value of the food, information about the good taste of the food, and mere exposure to the food. In addition to the role of culture in determining our diets, personal learning experience dictates which foods we will and will not tend to include in our diets. Negative food associations are formed quite readily. For example, a single episode of upper gastrointestinal illness (i.e., vomiting) after eating a particular food can be enough to produce a strong and resilient conditioned taste aversion. Presumably, this aversion has a protective function by keeping us away from a food that may make us sick again and endanger our health. Interestingly, illness after ingesting foods of animal origin is more likely to lead to the development of a conditioned taste aversion than is illness after eating fruits, grains, or vegetables.
Sensory qualities of foods themselves may override our bodies’ hunger and satiety cues, resulting in our eating either more or less of the foods. For instance, we generally eat more as a function of the variety of foods we are offered, with total food intake increasing with greater variety. Even variety in the texture of a single type of food we are offered (e.g., different pasta shapes, ice cream vs milkshake) can increase our total food intake as compared with the presentation of a single texture of that food alone. The taste of a food also moderates our desire to eat more or less of it. Foods that are high in sugar and fat are intrinsically more appealing to the human palate, so it is not surprising that we are more likely to consume more of these foods when we are given the opportunity. According to the evolutionary perspective, this preference for sweet and fatty foods is due to those foods’ scarcity during the hunting-and-gathering phase of human evolution and their energy content per gram of food as compared with foods high in protein. We can also lose our appetite for eating a specific food, a phenomenon known as sensory specific satiety, but then begin eating again when a new food is introduced. Most of us have experienced a resurgence of appetite for dessert, despite feeling full after finishing dinner. It is as though our bodies ‘‘get bored’’ of a particular food or taste after a while, prompting us to seek out more variety in our diets. This effect would presumably have a positive impact on our health by increasing the number of nutrients in our system.
Despite the cultural variations in cuisine and food selection, research has shown that humans are generally good at self-selecting a nutritionally balanced diet—at least they are as children. In a classic series of studies by Davis, human toddlers were offered a ‘‘buffet-style’’ meal plan and were allowed to choose the type and amount of food they ate. Her results showed that the toddlers self-selected foods that together made up a nutritionally balanced diet and resulted in a normal and stable pattern of weight regulation.
3. Social Influences On Eating Behavior
Although we may start out with an intrinsic appetite for foods that will maximize our chances of being healthy as well as a general reliance on internal hunger and fullness cues, as we grow, our eating is more likely to be influenced by non-nutrient-related variables. One social factor affecting how much we eat is the number of people who are present in a given situation. We generally eat more as a power function of the number of people present. One proposed explanation for this social facilitation of eating behavior is related to competition for food resources; that is, we do not want to lose out on the opportunity to eat by letting our companions get to the food first. Another explanation is that the mere presence of people may provide distraction from our satiety cues. Of course, in real life, the presence of eating companions is often confounded by other factors that stimulate eating such as the variety and quantity of foods available (e.g., the ‘‘dinner party’’ effect). There is some evidence that the relationship between people who are eating together also moderates this social facilitation effect; that is, we are more likely to eat dessert when our eating companions are friends than when they are strangers. This suggests that the presence of others, particularly others with whom we are socially close, reduces inhibitions around eating. Interestingly, the idea that we eat more with more people present does not appear to hold true for obese and dieting individuals, who actually eat less when eating with others and are prone to splurge when eating alone. Presumably, for these individuals, an impression management motive—the desire to present themselves to others as being small eaters—overrides the effect of social facilitation of eating.
In addition to the mere presence of other individuals, the eating behavior of those individuals affects our own eating behavior. Modeling by others has a strong influence on eating behavior in that individuals tend to match the amount eaten by those with whom they are eating. For instance, even when we are very hungry, we will tend to match a small amount eaten by our companions.
4. The Role Of Personality In Eating Behavior
Personality also influences diet and eating behavior. The goal of weight loss or weight maintenance is the most common reason for efforts to control one’s eating.
Herman and Polivy’s ‘‘restraint theory’’ of eating behavior emphasizes the importance of chronic attempts at dieting as a predictor of food intake and has been very influential in the study of eating behavior. In research studies, restrained eaters (or chronic dieters) have been shown to demonstrate several differences with respect to their eating as compared with their unrestrained eating counterparts. Psychologically, restrained eaters exhibit higher body dissatisfaction, lower self-esteem, and a higher drive for thinness. Although dieters’ eating can be characterized essentially as an attempt to reduce energy intake (calories, fat, and/or portion size), they are especially prone to overeating. Laboratory studies of eating often employ a taste test methodology to demonstrate this effect. Participants are allowed to ad lib eat as part of an ostensible taste test during which they rate the different taste properties of the food (e.g., sweetness, saltiness). Their total food intake is measured by subtracting the weight of the plate(s) (or, in some cases, counting the number of food items eaten such as candies) after the experiment from the preexperiment weight. Sometimes, participants are given a ‘‘preload’’ or snack to eat before the taste test, and they are typically exposed to an independent variable of interest before the eating task. Disinhibited eating or overeating among dieters has been demonstrated to occur in response to ingestion of a high-calorie preload (e.g., milkshake, chocolate bar), stress, perceived weight gain, food cues, lowered mood, positive mood, exposure to thin media images, and even anticipated future overeating. With all of these and more potentially disinhibiting factors, it is not surprising that studies have shown that dieters tend to eat more overall, and also weigh more, than do nondieters. As noted previously, humans are inclined to select foods based on their sensory qualities. Obese and dieting individuals are particularly dependent on external and sensory cues in deciding how much of a food to eat, showing a heightened preference for good-tasting food over that of their normal-weight or nondieting counterparts.
Herman and Polivy’s ‘‘boundary model’’ of overeating posits that restrained eaters have a cognitively determined ‘‘diet boundary’’ that exists before the experience of satiety. This boundary represents what a dieter believes he or she should eat. Under normal conditions, food intake is expected to remain within the limits set by the diet boundary. However, once eating has surpassed the boundary limit (e.g., by ingesting a high-calorie preload such as a milkshake), eating will continue until eventual fullness is achieved. Herman and Polivy labeled this event the ‘‘what the hell’’ effect; given that the dieter’s self-imposed diet boundary has already been surpassed, the dieter continues to eat until satiety and sometimes even beyond. Therefore, intended eating behavior for restrained eaters is cognitively determined by perceptions of what should be eaten in terms of type or quantity of food. In contrast, unrestrained eating is relatively more determined by an awareness of hunger or satiety cues.
5. Set Point Model Of Weight Regulation
There is solid evidence for a genetic factor in body weight determination. In terms of weight, adopted children tend to resemble their biological parents more than they do their adoptive parents. Identical twins, even when reared apart, are more similar in terms of weight than are fraternal twins or siblings. These examples suggest that genetics plays a role in determining one’s ‘‘set point,’’ that is, a type of internal sensor around which weight is regulated. When fat levels fall below this set point, the body responds by slowing metabolic processes so as to require fewer calories, thereby making the body more efficient in its energy expenditures and fighting against the depletion of fat stores. Keys and colleagues demonstrated this scenario in an experimental study of human semistarvation during World War II. Participants in the study were young men who agreed to lose 25% of their body weights for the study for the purpose of determining the best way in which to refeed starving people in war-torn Europe. On rations of 50% of their original daily caloric intake, the men initially lost weight quickly. However, over the 6-month starvation phase of the experiment, the men’s rate of weight loss reached a plateau, with many participants’ rations needing to be cut even further to achieve the desired weight loss. Keys’s starving participants exhibited a number of symptoms characteristic of the body’s corrective action of falling below its normal weight (and, presumably, below its set point in this initially nondieting sample). The men became irritable, miserable, hungry, and obsessed with thoughts of food. Their basal metabolic rates decreased significantly, indicating their bodies’ desire to conserve as many calories as possible. They became apathetic and lethargic, avoiding as much physical activity and energy expenditure as possible. They had very strong urges to overeat, and when they were allowed to eat during the refeeding phase of the experiment, they overate and demonstrated a preference for high-calorie foods that would increase their fat stores most quickly, a situation that is consistent with the predictions of set point theory.
In another study of the effects of overeating that also found evidence supporting the set point theory, Sims and colleagues recruited prison inmate volunteers to gain 25% of their body weights as part of an experiment. The men’s food intake was increased, and their physical activity was decreased and controlled. At first, the volunteers gained weight easily, but the rate of weight gain soon slowed and their daily caloric intake had to be increased for them to continue gaining. One man did not reach his goal weight even though he consumed more than 10,000 calories per day. Once the men reached their goal weights, the men continued to require extra calories to maintain their higher than normal weights. During the experiment, these volunteers began to be repulsed by food and had to force themselves to eat. Many considered dropping out of the study due to the discomfort of overeating. Physical responses included an increased basal metabolic rate and profuse sweating, indications that their bodies were eliminating the excess calories they were ingesting. After the experiment, there were differences in how quickly the men returned to their preexperiment weights, with two participants (both with family histories of obesity) never reaching their original weights.
In sum, there is evidence that our body weights and shapes have a genetic component, but changes in eating behavior, hormones, or other variables can also produce weight gain or loss. Because of this apparent contradiction, some researchers have abandoned the set point theory of weight regulation in favor of a ‘‘settling zone’’ alternative. In 2002, Levitsky argued that within the biologically determined range or zone of body weight, actual body composition may ‘‘settle’’ at a value determined by behavior. Furthermore, the width of one’s settling zone may also depend on individual factors such that some individuals will naturally experience greater weight fluctuations over time than will others.
6. Obesity And The Problem Of Eating Too Much
Although genetics can predispose individuals to higher than average weights, there is no doubt that overeating can contribute to obesity. Because of societal pressure to be thin and the stigma against overweight persons in many parts of the world, the obese and dieting populations overlap considerably. Therefore, many of the disinhibiting factors discussed in the preceding section operate regularly on the eating behavior of obese persons, leading to frequent episodes of overeating. In the preceding section, it was pointed out that overeating can occur beyond the point of satiety and until stomach capacity is eventually reached. Binge eating consists of eating episodes that involve consuming large quantities of food (e.g., twice a normal serving) combined with a feeling of being out of control. For binge eaters, food intake may continue until they reach capacity, and there is never really a sense of feeling as if they have eaten enough to satisfy their hunger. Binge eating combined with compensatory behaviors, such as self-induced vomiting, excessive exercise, extreme food restriction, and laxative abuse, is the hallmark of bulimia nervosa, an eating disorder. ‘‘Binge eating disorder,’’ although not currently a formal diagnostic category, is characterized by regular binge eating episodes without attempts at compensation and is estimated to be highly prevalent in the obese population.
There is little consensus on the technical definition of obesity. Traditionally, charts that provide normal weight ranges for various heights and body frame sizes were the standard tool for determining normal weight and overweight. These charts were originally published by the Metropolitan Life Insurance Company in 1959, were based on associated mortality rates, and have undergone revisions during more recent years. Another method that gained popularity during the 1990s is the body mass index (BMI), which is defined as BMI = kg/m2. A BMI of 20 to 25 is considered to be medically ideal, and obesity is defined as a BMI of 30 or more. However, unlike the Metropolitan Life Insurance charts, BMI does not take into account gender, age, or body frame. Body fat distribution can be estimated through one’s hip-to-waist ratio. A low hip-to-waist ratio indicates that the person is carrying fat around their midsection, whereas a high hip-to-waist ratio indicates a relatively small waist and larger hips. The skinfold technique measures the thickness of a pinch of skin, usually under the upper arm. Despite the convenience and low cost of all these techniques, none of them is very accurate at measuring body fat. The most accurate method for assessing body fat is the water displacement method, whereby the individual is immersed in a tank of water and the displaced amount of water is measured. Obviously, this method has its practical drawbacks.
Obesity is unquestionably socially undesirable in many cultures today. But is it actually unhealthy? Unfortunately, the research is unclear as to how much weight gain is associated with increased health risks such as hypertension and cardiovascular disease. Being obese (BMI > 30) has reliably been shown to put people at a significantly elevated risk for all-cause morbidity, premature death, type 2 diabetes, gallbladder disease, high blood pressure, sleep apnea, respiratory problems, liver disease, osteoarthritis, reproductive problems (in women), and colon cancer. However, those in the overweight category (25 < BMI < 30) might not experience much more risk than do those in the normal weight range. Furthermore, weight loss itself can be a health risk for some. Most experts agree that there is a U-shaped relationship between weight and mortality and that a person’s optimal weight range is uniquely determined by his or her own biology, varying with age and even ethnic background.
7. Overcoming Obstacles To Weight Control
Of course, the most common method for weight loss is caloric restriction through dieting. However, most normal-weight dieters would be healthier if they did not diet at all. Dieting has psychological costs (e.g., irritability, hunger, food obsession), may be ineffective in improving health, and can worsen body dissatisfaction. Anorexia nervosa, another eating disorder, is characterized by extreme food restriction despite very low weight. The dieting of anorexics typically has a compulsive quality to it, and anorexia nervosa is routinely a difficult disorder to treat.
There are several obstacles to weight loss through dieting. A person’s genetically influenced set point may be higher than his or her desired weight, and efforts at reducing caloric intake may be counterproductive and result in decreased metabolism and increased fat stores. Dieting individuals show an increased preference for restricted or forbidden foods and are more sensitive to sensory food cues, eating more good-tasting foods— foods that are also likely to be higher in sugar and/or fat content. Emotional states may lead to overeating or binge eating. Finally, calorically dense foods are all too available and convenient, leading to unbalanced food choices. With an increasingly thin and lean physical ideal for both men and women, it is not surprising that there has been a rise in more drastic weight loss methods over recent years. All of the drastic weight loss methods are unhealthy. Extreme restriction and elimination of a food category from an individual’s diet are nutritionally ill advised. Fasting, surgery, and diet drugs have significant and sometimes fatal health risks associated with them. Even when weight loss is achieved (and regardless of the method used), weight loss is very difficult to maintain in the absence of permanent lifestyle changes and good nutritional habits.
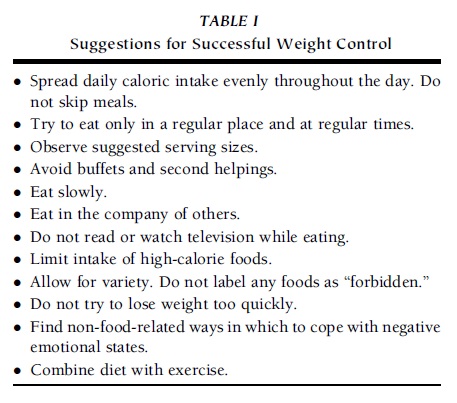 TABLE I Suggestions for Successful Weight Control
TABLE I Suggestions for Successful Weight Control
However, despite the low success rates of weight loss methods in general, most experts agree that the way in which individuals select foods and eat can have a positive impact on their weight and health. Table I displays suggestions for achieving a healthy and stable weight. The goal of these behaviors is to bring one’s eating more in line with bodily cues of hunger and satiety and to try to override many of the psychological factors that can lead to overeating.
In addition to these practical ways in which to make eating more in tune with the body’s needs, cognitive factors can be modified to reduce a reliance on dieting. Specifically, there is evidence that many dieters demonstrate unrealistic expectations for weight loss. They believe that profound and positive changes will result from losing weight in terms of their success in personal, social, and/or professional realms. In reality, weight loss rarely brings about the type of happiness that dieters anticipate. In addition, many chronic dieters demonstrate ‘‘false hope beliefs’’ around dieting. That is, despite numerous failed attempts in the past, these dieters believe that the next diet will surely work. Previous diet failures are frequently attributed to lack of will power or perseverance on the part of the dieters rather than to the intrinsically difficult nature of successful long-term weight loss. Not only is this belief incorrect, but it can also be demoralizing, often exacerbating the poor self-image that precedes dieting efforts.
References:
- De Castro, J. M., & Plunkett, S. (2002). A general model of intake regulation. Neuroscience and Biobehavioral Reviews, 26, 581–595.
- Drewnowski, A. (1995). Energy intake and sensory properties of food. American Journal of Clinical Nutrition, 62, S1081–S1085.
- Fairburn, C. G., & Brownell, K. D. (2003). Eating disorders and obesity: A comprehensive handbook (2nd ed.). New York: Guilford.
- Hetherington, M. M. (1996). Sensory-specific satiety and its importance in meal termination. Neuroscience and Biobehavioral Reviews, 20, 113–117.
- Levitsky, D. A. (2002). Putting behavior back into feeding behavior. Appetite, 38, 143–148.
- Martins, Y., Pelchat, M. L., & Pliner, P. (1997). ‘‘Try it; it’s good and it’s good for you’’: Effects of taste and nutrition information on willingness to try novel foods. Appetite, 28, 89–102.
- Ogden, J. (2003). The psychology of eating. Oxford, UK: Blackwell.
- Polivy, J., & Herman, C. P. (2002). Causes of eating disorders. Annual Review of Psychology, 53, 187–214.
- Stunkard, A. J., Sorensen, T. I. A., Hanis, C., Teasdale, T. W., Chakraborty, R., Schull, W. J., & Schulsinger, F. (1986). An adoption study of human obesity. New England Journal of Medicine, 314, 193–198.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to order a custom research paper on any topic and get your high quality paper at affordable price.





