This sample Depressive and Anxiety Disorders Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Introduction
Following the development of standardized diagnostic systems in the early 1980s (e.g., Research Diagnostic Criteria of Spitzer and colleagues and the DSM-III of the American Psychiatric Association) and their incorporation into large-scale epidemiological studies, there has been widespread acceptance of the dimensional nature of the common anxiety and depressive disorders. Such dimensional concepts can be readily incorporated into large-scale population-health and health service development plans. Importantly, they place an emphasis on detection and active management of the very common mild and moderately severe cases. In this environment, the center of clinical management is shifted from specialist care settings (for more severe, prolonged, treatment-resistant, comorbid and medically complicated) to primary care.
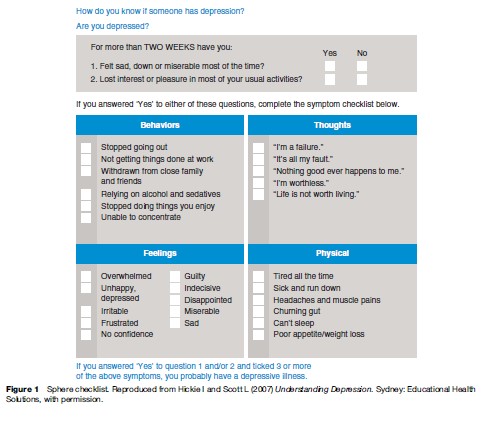
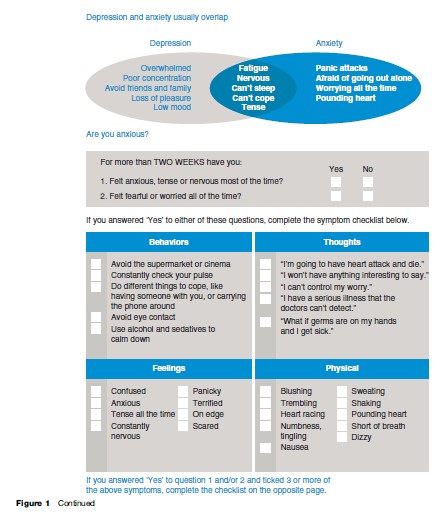
These broad concepts of depression and anxiety have predictive value for key outcomes such as response to available treatments, disability, and premature death. They incorporate the key symptom domains (e.g., affective, cognitive, sleep–wake cycle, somatic, behavioral, and self-harm) and they can also be readily incorporated into public and professional education campaigns as well as everyday clinical practice. For example, simple checklists can be widely circulated through e-health, media, print, and health-care distribution systems (see Figure 1 for an example from the SPHERE-program in Australia).
Clinical debate as to the best ways to describe the relationship between different anxious and depressive phenotypes (e.g., mixed anxiety and depression, generalized anxiety and its relationship to dysthymia (symptoms of depression), and major depression), and between different depressive dimensions (e.g., major versus minor depression and unipolar versus bipolar spectrum disorders) will continue until more discrete pathophysiological pathways are identified. The development of future international diagnostic systems (e.g., DSM-V) has signaled this necessary move from over reliance on imprecise cross-sectional phenotypes to diagnostic categories based on putative causal paths.
A great deal of academic effort has been expended in epidemiological and clinical studies that seek to differentiate anxiety from depressive disorders or subtype the multiple and complex presentations of these conditions. These efforts have reflected traditional but simplistic belief systems about causality (e.g., psychosocial vs. biological) or the relevance of subtyping to the selection of specific medical or psychological therapies (e.g., only certain subtypes of depression benefit from one or other antidepressant medication; only psychological therapies should be provided to persons with anxiety disorders). In the absence of discrete biological or psychosocial markers of illness risk, illness onset, diagnostic subtypes, predictors of response to specific treatments, or illness course, we continue to work with broad syndromal concepts rather than valid or discrete diagnostic categories. Consequently, anxiety and depressive syndromes typically co-occur when studied either cross-section ally or longitudinally, and generic terms such as common mental disorders are used.
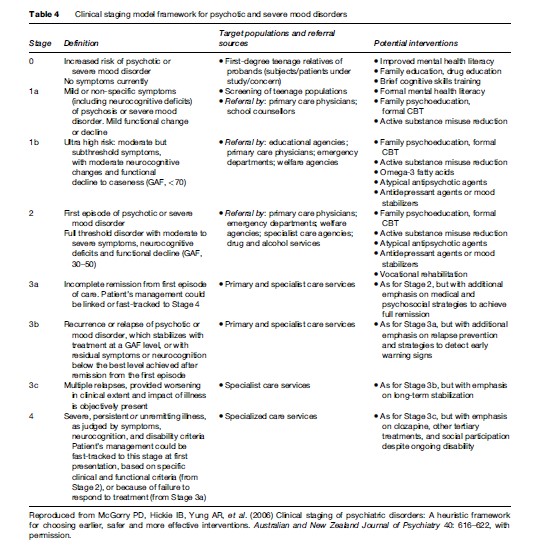
Another important development in the clinical theorizing about common mental disorders has been the development of clinical staging models. Within this paradigm there is clear recognition that those at risk (Stage 0: as a result of exposure to relevant biological or psychosocial risks) or those with earlier and less severe manifestations of illness (Stage I: subthreshold symptoms with disability; and II: first clear episode with disability) are very common and likely to respond well to a range of information, e-health, and brief clinical interventions. These all have the potential advantages of being able to be delivered to large numbers of persons at relatively low cost either directly or with the assistance of a wide range of community agencies. They are particularly relevant to application in primary health care, education, and workplace settings. Specialized health-care workforces are more likely to be engaged preferentially in the provision of care to persons with more severe illnesses, those who have failed to respond to simpler clinical interventions, or those with major physical health, substance misuse, or other social complications of their conditions.
Burden Of Depressive And Anxiety Disorders
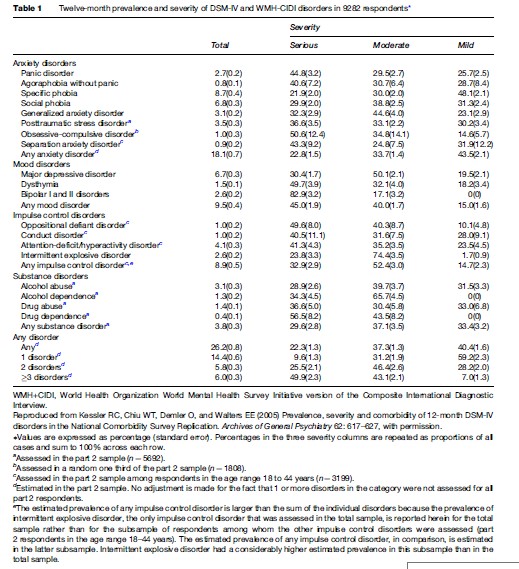
Anxiety and depressive disorders are among the most common health conditions. At least one in ten persons will report symptoms and associated reduction in work or social function in any 12-month period. When combined with co-occurring harmful use of alcohol or other substances (which is particularly important for men), the estimates increase to one in five adults in any 12-month period, as shown in Table 1. As depression is common right across the lifespan, lifetime risk for depression may be as high as 30% for men and 40% for women.
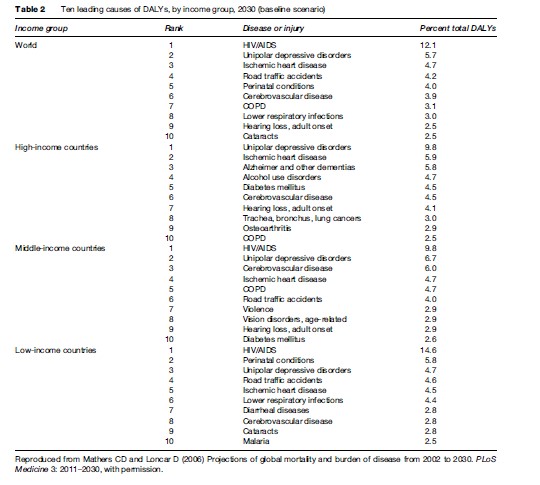
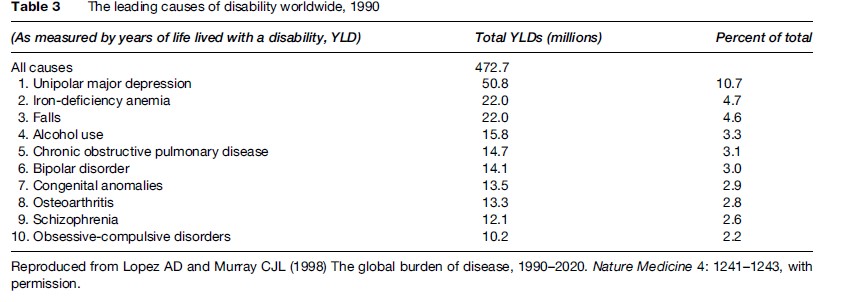
There is no doubt that one of the most important drivers to public, professional, and health policy attention to the importance of depression and anxiety has been the improved measures of health-related disability used in association with the global burden of disease studies. For the first time, the real impact of these common conditions could be directly compared with that of other health problems. To the surprise of many, the overwhelming contribution of unipolar major depression demanded attention.
In 2000, depression was the leading cause of disability as measured by years lived with disability (YLDs) and the fourth leading contributor to the global burden of disease (DALYs – disability-adjusted life years, which is the sum of years of potential life lost due to premature mortality and the years of productive life lost due to disability). By the year 2020, depression is projected to become the second highest cause of DALYs calculated for all ages and both sexes. Today, depression is already the second cause of DALYs in the age category 15–44 years for both sexes combined.
Not only is depression the major cause of health related disability internationally, but its contribution is only likely to increase in both developing and developed nations (see Mathers and Loncar, 2006; The Lancet Series on Global Mental Health, 2008). Given the lack of population-based campaigns to reduce this impact and the increasing recognition of the contribution of early-onset anxiety and depressive disorders to other health conditions (e.g., vascular disease) and other key risk factors (e.g., tobacco, alcohol, substance misuse, overweight), international and national health bodies have increasingly moved to develop more appropriate responses (Lancet series on Global Mental Health, 2007).
A more critical discourse has developed with regards to the accuracy of these health burden predictions. Typically, the attention of the international health community has been focused on those more traditional physical health areas (e.g., infectious diseases, cardiovascular diseases, and cancer) that make large contributions to premature death rather than ongoing disability. The largely hidden disability associated with common forms of anxiety and depression is often more evident to those with a wider community focus on education, training, employment, welfare, housing, and legal services than those who work within general health or specialist mental health-care settings. The specific ways in which mental health leads to poor physical health outcomes has been significantly underestimated (Lancet Series on Global Mental Health, 2007) (Tables 2 and 3).
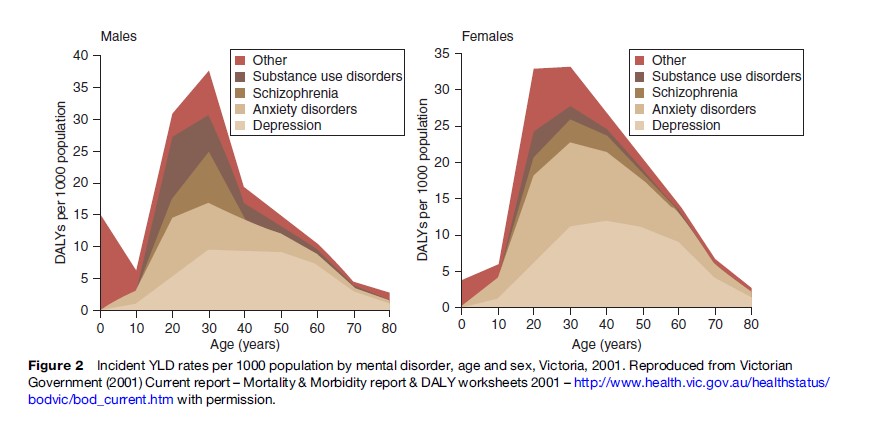
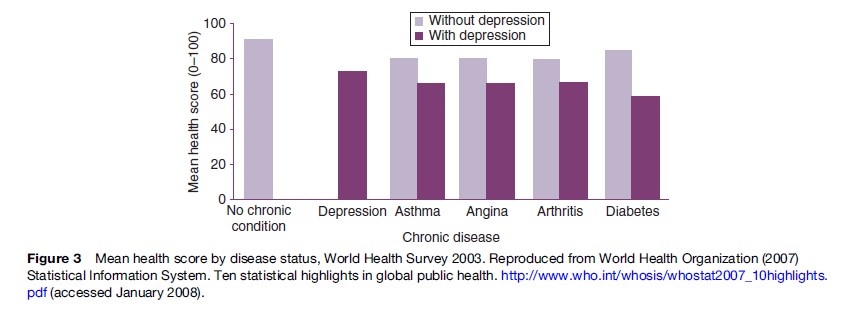
A basic risk relationship exists between increasing severity and duration of anxious and depressive symptoms and a range of adverse outcomes, including impairment of daily functions, premature death, increased rates of misuse of alcohol, tobacco, and other drugs, and poor physical health (notably increased rates of cardiovascular disease). The significance of these common conditions has been a surprise to many national and international health policy bodies. However, this is the predictable impact from disorders that commence in adolescence or early adult life, are associated with significant decrements in daily function (particularly reductions in education, training, and employment), persist or frequently recur, go largely untreated, lead to secondary medical morbidity and harmful use of alcohol and other substances, and do not result typically in major decrements in life expectancy. That is, a pattern of chronic ill health and disability is established just at that point in the life cycle where communities expect to receive the greatest returns on previous investments in childhood health and education. Figure 2 demonstrates that the per capita incident nonfatal burden attributable to mental health (primarily depression and anxiety) is far greater in early adulthood than at any other age. Depressive disorders also commonly accompany other medical conditions, particularly in aging populations. When depression does co-occur with other common medical conditions, the degree of resultant disability is higher than for any other combination of health conditions. This is illustrated in Figure 3, those with depression and another chronic condition had much lower mean health scores when compared with people who had only a chronic condition. These patterns were consistent even after adjusting for other sociodemographic variables.
Risk Factors
Each of the major risk factor domains (genes, family environment, and individual-specific environment) influence depressive and anxiety disorders in a distinct manner. There is also a complex interaction between these risk factors that is still to be unraveled. What is absolutely clear is that social determinants affect mental health throughout life. People who are at the lower end of the socioeconomic ladder experience twice the risk of serious illness and premature death as those near the top. This effect is not limited to lower-income countries but rather is consistent across the spectrum of society. Specifically, the most disadvantaged groups in any community experience greater incidence of depression, drug use, anxiety, hostility, and feelings of hopelessness, which all rebound on physical health.
Our understanding of the specific nature of both the biological and social risk factors to anxiety and depression have advanced significantly in recent years. At this time, we have moved well beyond the simplistic nature vs nurture debates of previous decades. On the basis of extensive twin and other genetically informative population and family studies, it is clear that at least 30% of the population-based risk to depressive disorders in adults can be attributed to additive genetic factors. Of the 70% of risk that is not readily attributed to genetic factors, most (up to 60%) is due to current (or unique) environmental factors rather than childhood (about 10%) experiences.
For those anxiety and depressive disorders that are present in early adult life, it appears that many of the genetic influences are shared in common and that overt differences in clinical presentation may be attributed to differential exposure to other environmental risk factors (e.g., personal trauma, dysfunctional parenting styles, or other interpersonal factors). Importantly, it is now clear that the pattern of genetic and environmental risk factors varies across the life span, with new genetic and environmental factors (particularly related to vascular disease and neurodegenerative disorders) beginning to emerge in later life.
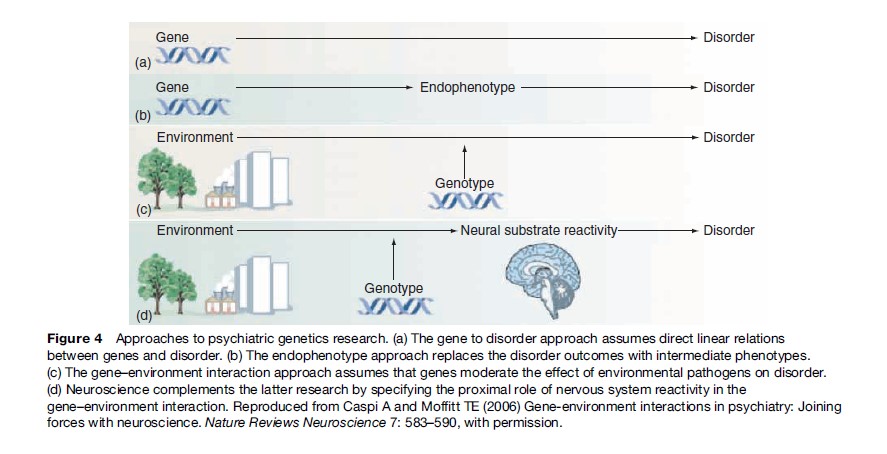
Perhaps the most significant development in our understanding emerged with the publication of longitudinal studies demonstrating the additional risks that occur when an individual has both specific polymorphisms of genes of biological relevance to anxiety and depression (e.g., selective serotonin transporter) and exposure to specific childhood (e.g., maltreatment) or adult (e.g., recent interpersonal stressors) environmental factors (Caspi and Moffitt, 2006). These specific gene–environment interactions have long been postulated but not previously documented. They allow us to move beyond simplistic genetic or environmental models of adult mental health problems to focus on the actual pathways that may be relevant. Inherent in these emerging models is the complex dance between genetic substrates and the timing and extent of relevant environmental exposures, as shown in Figure 4 (see discussion in Caspi and Moffit, 2006). This more detailed knowledge may assist us in designing more targeted preventative and early intervention strategies. Certainly it has already led to a much more active reconsideration of the roles of specific environmental risk factors and the ways in which such risks may help us (in combination with other new neuroscience technologies such as structural and functional brain imaging) to better understand the biological mechanisms underpinning common anxiety and depressive disorders.
Age Of Onset Of Anxiety And Depression
For the common forms of anxiety and depression, the typical age of onset is the teenage or early adult years. Seventy-five percent of the common conditions commence before the age of 25 years. While various forms of anxiety are common in childhood, many are closely associated with perturbations in family and kin environments and do not necessarily persist into adulthood. Temperamental characteristics, such as social inhibition or social anxiety, which are the precursors of adult disorders, are often evident in early childhood and the preadolescent period. These temperamental characteristics appear to have their own genetic (e.g., polymorphism of the serotonin transporter gene) and/or other neurobiological determinants (e.g., heightened amygdala response to fearful stimuli).
The phenotypes associated with the onset of the more classical mood disorders begin to emerge in the adolescent era. There has been some debate about the variation in symptom patterns in younger persons with an emphasis on features such as increased somatic features of anxiety, irritability, inattention, brief and unstable mood variations, disturbed sleep–wake cycle, and persistent fatigue states. The disorders are also least likely to be identified or treated by health professionals during this period. Consequently, the age for first active treatment is often at least a decade after onset of the clinical manifestations of the disorder. By that time, the condition is likely to have become chronic or recurrent and to be associated with significant alcohol or other substance misuse, tobacco use, or other markers of social disability (reduced educational achievement, reduced employment, and dysfunctional interpersonal relationships).
Figure 4 Approaches to psychiatric genetics research. (a) The gene to disorder approach assumes direct linear relations between genes and disorder. (b) The endophenotype approach replaces the disorder outcomes with intermediate phenotypes. (c) The gene–environment interaction approach assumes that genes moderate the effect of environmental pathogens on disorder. (d) Neuroscience complements the latter research by specifying the proximal role of nervous system reactivity in the gene–environment interaction. Reproduced from Caspi A and Moffitt TE (2006) Gene-environment interactions in psychiatry: Joining forces with neuroscience. Nature Reviews Neuroscience 7: 583–590, with permission.
While many subtyping models of depressive disorders have been developed by clinicians, largely on the basis of cross-sectional phenotypic studies and short-term treatment trials, a system that simply differentiates early-onset (typically before 25 years of age) from late-onset cases (typically after 60 years) appears to have closer links with basic patterns of pathophysiology. It is also likely to be of greater utility in terms of increasing public awareness of relevant risk factors and the value of pursuing different preventive strategies or treatment regimens at different ages.
For early-onset depressive disorders, the emphasis will inevitably continue to be on development of universal prevention programs in childhood and the early adolescent period. When combined with early identification and treatment of major anxiety disorders in childhood and the early school years as well as identification and active management of significant anxiety and depressive disorders during the secondary school period, there is an opportunity for major reductions in lifetime burden estimates. Given the emerging evidence of the adverse effects of untreated depression on critical brain regions such as the hippocampus and the positive effects of some treatments on brain growth factors (e.g., antidepressant and second-generation antipsychotics that increase levels of brain-derived neurotrophic factor), we will increasingly see an emphasis on not just ‘symptom reduction’ and social recovery but also brain protection for those with early-onset disorders. Figure 5 shows the level of hippocampal reduction in association with early and late-onset depression.
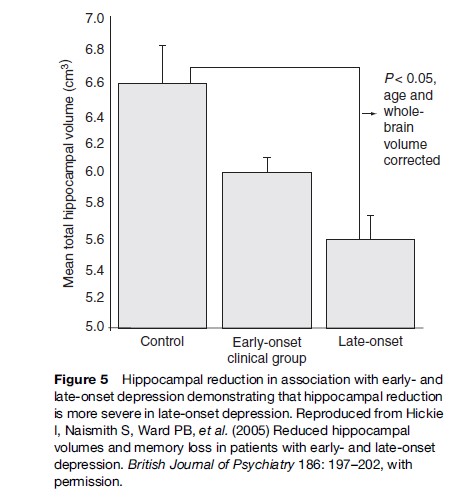
For those with late-onset depressive disorders, it is now evident that different genetic, vascular, and other medical and environmental risk factors play major roles. Typically, the onset rate of new anxiety and depressive disorders declines with increasing age. Onsets in this age range are typically due less to changing psychosocial circumstances than the onset of physical illness, brain changes, and/or social isolation or decreased participation due to ill health. Neuroimaging and neurocognitive research indicate that the patterns of brain change demand not only traditional antidepressant therapies but an increased emphasis on improved vascular and general medical health. Importantly, new opportunities for prevention arise in this age range. The clearest relates to improved vascular health, but this may well be complemented by a variety of other behavioral (increased exercise), dietary, and supplement (increased folate, B group vitamins, antioxidants and omega-3 fatty acids), employment, and socialization strategies.
Recent Neurobiological Models Of Depression
For the last 50 years, our neurobiological theories of depressive disorders have rested largely on circumstantial evidence of altered serotonin, norepinephrine, or dopamine neurotransmission. These functional monoamine models assume structural integrity within relevant frontal, subcortical, and temporal lobe nuclei and their connecting white matter tracts. However, there has always been an uneasy fit between this pharmacological model and the delay in clinical response, lack of difference in clinical outcomes associated with different neuropharmacological entities, benefits of medications that do not act principally on the monoamine systems, and evidence of progressive structural brain changes in persons with both unipolar and bipolar depressive disorders.
In the last 25 years, structural and functional brain imaging techniques have clearly demonstrated that substantive regional brain alterations occur in both early and late-onset major depressive disorders, as well as bipolar disorder. These regional brain changes are likely to reflect various alterations to the neural micro circuitry, including neuronal, glial cell, and synaptic components. In addition to regional changes affecting cortical and subcortical nuclei, disruption of white matter tracts and reduction in size of the frontal lobes, subcortical nuclei, and the hippocampus have all been detected and linked with key phenotypic features such as psychomotor change, cognitive impairment, and poorer illness outcomes.
Given the epidemiological linkages of mid-life depression with late-life cognitive impairment and dementia, there is now a need to reconsider the underlying nature of this association. Previously, it was assumed that such associations were unlikely to be causal but more likely to reflect shared risk factors, such as small vessel cerebrovascular disease or other late-life neurodegenerative processes. However, the clear demonstration of reduced hippocampal size and the likely association between such reductions and duration of untreated illness suggests that structural brain changes in depression may create a unique neurobiological vulnerability to later-life dementia syndromes.
Consistent with these findings in human studies, relevant neurobiological correlates of depression have emerged in animal models. Some of the most interesting include impaired hippocampal neurogenesis, impaired synaptogenesis, and altered glial cell structure and function. The therapeutic effect of antidepressant medicines in rat models appears to be dependent on restoration of normal patterns of neurogenesis in the hippocampus. Additionally, small changes in absolute cell numbers are associated with major changes in critical neurocircuit functioning.
Evidenced-Based Interventions
Community and health development programs for under resourced communities with poor physical health status often ignore the importance of common mental health conditions, despite the direct and large contributions of poor mental health to lack of sustainable change in health and economic indicators. In contrast, these communities often place high worth on programs that promote such concepts as emotional and social well-being, reduction in premature death due to suicide, injury, and accidents, as well as increased achievements in education, employment, and social participation as a result of promotion of better mental health alongside active identification and management of common mental health problems.
Delivery Of Evidence-Based Treatments Through Collaborative Care Models
As a consequence of the prevalence of anxiety and depression, the lack of investment in mental health care historically, negative community attitudes, and the patterns of organization of health systems established in the nineteenth and early twentieth centuries, even in the best resourced health systems, only a minority of those affected receive any care, let alone evidence-based treatments (see The Lancet Series on Global Mental Health, 2008). Future health service planning needs urgently to look at new methods of service delivery (e.g., e-health informational and clinical services – web examples of beyondblue, blue pages, moodgym, reachout central; reliance on educational and primary care-based workforces and promotion of collaborative care models) if we are ever to make substantial progress.
Two of the most important considerations here relate to the maintenance of choice in access to preferred treatments as well as the promotion of continuous improvement in the quality of services provided. Community surveys continue to highlight strong consumer preferences for increased access to nonpharmacological treatments, self-care strategies, detailed information about treatment options and self-monitoring tools. The emphasis on preference for psychological treatments is not limited to developed countries. The planning for delivery of adequate nonpharmacological strategies in developing countries has not been sufficiently addressed. Another major consideration is the continued emphasis in many primary care treatment settings on the short-term use of inexpensive sedatives and hypnotics rather than engagement in active antidepressant therapy. Negative community attitudes toward the use of antidepressant medicines persist and are reinforced by media and some professional stereotypes that overemphasize side effects, capacity for dependence, and links with self-harm or violence to others.
Of perhaps greater importance than the long-standing debate on the relative merits of pharmacological as compared with other modes of treatment has been the neglect of the issues of ensuring adequate adherence to any evidence-based therapy to achieve full remission and prevent recurrence. While such issues have been highlighted within clinical trial environments, they require significant restructuring of health-care systems (with greater use of information technologies, recall systems, and active monitoring tools) and greater emphasis on engaging consumers and carers in long-term rather than short-term treatment plans.
There is now no doubt that collaborative (or stepped) care models of clinical service, as shown in Table 4, deliver on the twin objectives of active engagement and continuous quality improvement. Sadly, even in well-resourced countries many professional groups and third-party insurance systems continue to promote more limited fee-for-service or other disjointed service models. In some national and private insurance systems, health care for mental disorders may be actively excluded or care severely restricted. The next major challenge for improved care for mental disorders such as anxiety and depression will be active recognition by health-care systems that when poorly managed these conditions are chronic, disabling, and costly to treat. In contrast, when actively managed with the appropriate and ongoing mix of psychological and medical care, costs are minimized and good health and economic outcomes are achieved.
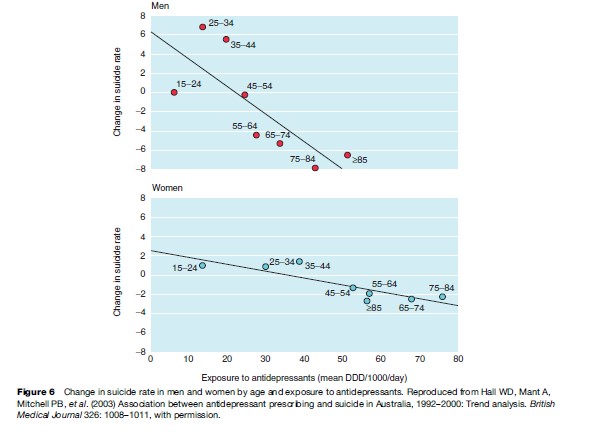
Impact Of Increased Treatments On Suicide Rates
One of the most important arguments for increasing access to treatments for those with anxiety and depressive disorders is to reduce premature death due to suicide, accident, and other injuries and other medical complications such as coronary heart disease. The most impressive evidence for the benefit to be derived by increased treatment of mild and moderately severe depressive disorders in recent years has been the associated decline in suicide rates in proportion to the increase in access to care, as demonstrated in Figure 6. While this interpretation has been debated, sufficient evidence has accumulated across a large number of countries and treatment settings to support this interpretation (policy references). Of concern have been the recent reports that decreased provision of treatments to young persons in the United States and Europe (after regulatory bodies issued specific warnings about the potential dangers associated with antidepressant therapy) has now been associated with an upward spike in deaths due to suicide. International suicide prevention research has typically focused on other large community, demographic, and social factors (including reducing access to lethal means), while placing less emphasis on those clinical care factors that have a strong evidence base. These more recent studies suggest that particularly in well-resourced and socially stable countries, greater emphasis should now be placed on improved access to evidence-based care.
Matching Pathophysiological Models To Clinical Practice
The most recent large clinical effectiveness trials – Sequenced Treatment Alternatives to Relieve Depression (STAR*D) – provide even more reason to challenge the existing pharmacological dogma. What is most impressive in these studies is the marked effect of prolonged duration of pharmacological treatment. Independent of the specific characteristics of the treatment provided, fewer than 30% responded in the first 12 weeks of SSRI treatment, while another 20–30% responded in the next 14 weeks, and a further 12–20% responded in the last phase, as shown in Figure 7. This prolonged time course of additional clinical benefits is consistent with the view that full recovery depends on fundamental changes in underlying cellular or circuit elements.
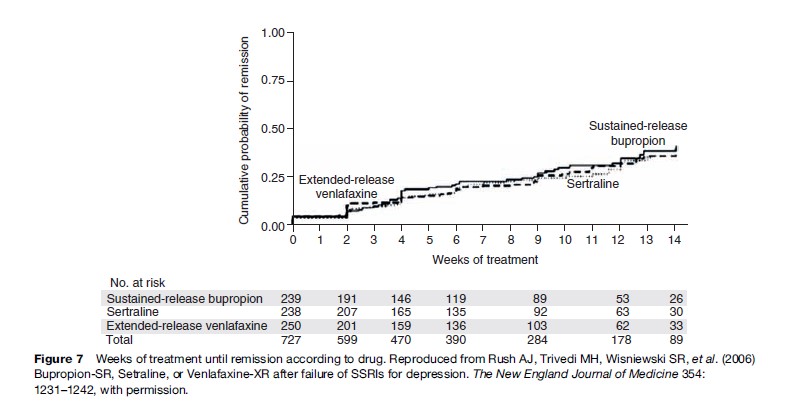
To date, we do not have evidence from clinical studies that clinical recovery is linked directly to increases in hippocampal or other regional brain volumes or specific markers of neurogenesis or synaptogenesis. In the interim, the clear indication is that acute treatments may need to be prolonged to achieve maximal neurobiological benefits. Additional considerations include more active consideration of proposed neuroprotective compounds. These include not only the traditional psychopharmacological agents such as lithium carbonate, but also the second-generation antipsychotics that have been shown both to increase brain-derived neurotrophic factor (BDNF) as well as reduce brain changes during the early phases of psychotic disorders. Other potential augmentation or treatment strategies include folic acid, antioxidants, statins, and omega-3 fatty acids.
Primary And Indicated Preventative Interventions
Some of the key social risk factors (e.g., dysfunctional parenting; physical, sexual, or emotional abuse) to adult anxiety or depression are clearly operative in early life and, hence, it is a key period for consideration of relevant primary preventative health programs. Of greatest interest from a broad population health perspective are those broad social, community, and family-based approaches that promote both good physical and mental health in pregnancy and throughout the early years. Prenatal identification of cases of anxiety and depression, which can lead not only to immediate treatment of the mother, but also to active engagement of the partner and extended family with consequent increased practical and emotional support following the birth, has obvious appeal (see beyondblue, the National Depression Initiative and beyondblue postnatal depression, Beyondblue Schools Research Initiative, 2007). For similar reasons, increased detection and treatment of postnatal depression has been extensively promoted.
Most population health planning (including most health service systems) has made little provision for early intervention and indicated prevention particularly for these adolescent and early adulthood cases of depression and anxiety. The challenge of youth mental health is now recognized internationally. Traditional health systems tend to focus on child health needs (infectious diseases, nutrition, immunization, management of developmental difficulties) and then the needs of adults in mid and later life (musculoskeletal, cardioand cerebrovascular, cancer, dementia, and diabetes). Such traditional patterns of organization of services are therefore weakest at that period of life when the need for early and effective intervention for anxiety and depressive disorders is greatest.
In higher-income countries, there has been some recognition of the importance of the adolescent-onset period. This has led to the development of universal primary intervention programs aimed to promote mental health awareness, reduce social, interpersonal, and other known risk factors (including alcohol and other substance misuse and bullying), teach specific cognitive and behavioral skills, and/or enhance other community supports (see Gatehouse Project, 2007; beyondblue Schools Research Initiative, 2007). These have been delivered mainly through school-based settings and more recent projects have attempted to integrate such initiatives into the ongoing early high school curriculum and related school environment. The longer-term value of such programs is not yet evident, but this remains a critical arena for development.
Other clinically based early intervention and indicated prevention programs are now under development internationally (see Headspace, 2008; Headstrong, n.d.). Such programs promote not only new pathways to care for young persons but also earlier engagement through e-health and other primary care health and education systems, provision of effective multidisciplinary care early in the course of illness, long-term professional and self-care packages, reduction of secondary alcohol and other drug use, and return to education, training, and employment as key outcome variables. The effectiveness of e-health-based interventions has been well demonstrated and offers real hope of providing low-cost and accessible interventions to young persons (particularly young men) who do not readily engage with clinical services.
Improving Public Understanding Of Anxiety And Depressive Disorders
The lack of provision of effective treatments to persons with anxiety and depression is perceived by health professionals internationally as the major challenge for future health policy and service development. Quite often, however, surveys of those who experience these disorders, and their families and care providers, prioritize the reduction in the consequences of lack of accurate information and overt stigma, as shown in Table 5. These negative effects take many forms and extend well beyond the expression of negative personal attitudes to include restrictions of access to health care as well as significant barriers to full participation in employment, education and training, insurance, and other financial systems.
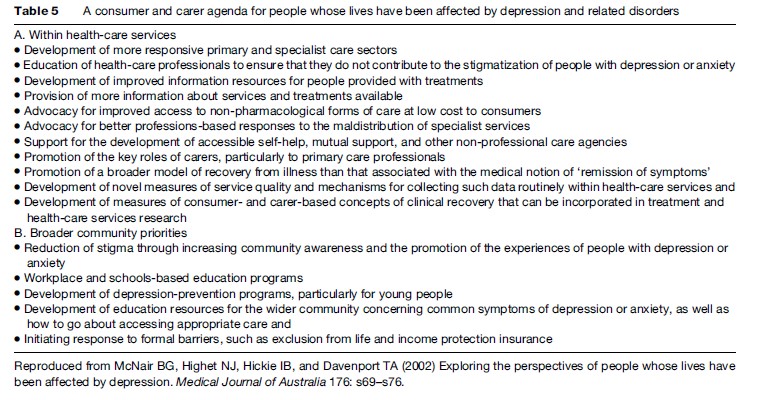
A wide variety of factors have been identified that contribute to these adverse experiences for persons who have these common mental disorders. Some are largely historical and relate to the basic lack of knowledge about the physiological correlates and adverse health and economic consequences of living with untreated forms of anxiety and depression. Others relate to the low priority individuals give to the relative importance of mental health as distinct from physical health problems, as shown in Table 6.
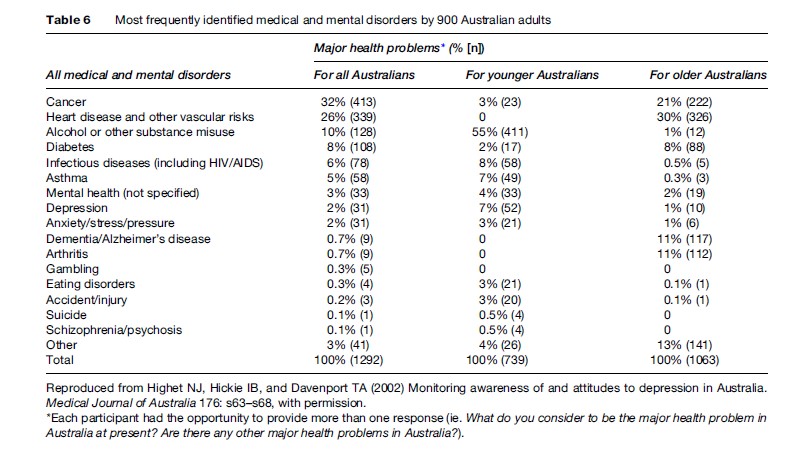
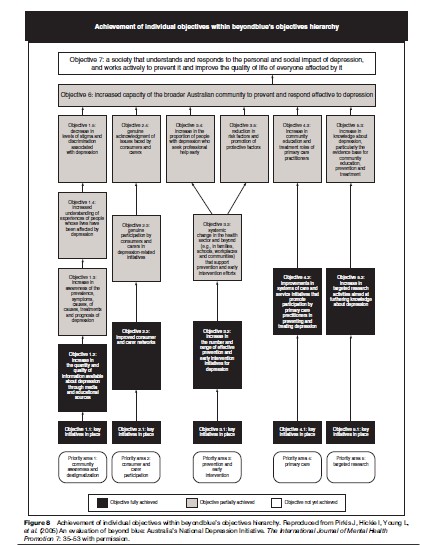
These views have underpinned the development of measures of mental health literacy (see Jorm et al., 2006) and supported the implementation of specific regional (see Hickie, 2004), national (Beyondblue, the National Depression Initiative (2008)) and local interventions to increase community awareness, promote positive views of help-seeking, and reinforce accurate knowledge of the benefits of professional or self-care interventions. It has been possible, at least in some better-resourced countries, to develop a comprehensive and integrated approach to increased public awareness, consumer and care provider participation, removal of societal barriers and primary health-care reform (see Figure 8). An important part of this movement has been the systematic study of the attitudes and knowledge of different health-care professionals. Consumers of care often report that the most negative attitudes they encounter are expressed by general health and other specialist mental health providers.
Bibliography:
- Caspi A and Moffitt TE (2006) Gene-environment interactions in psychiatry: Joining forces with neuroscience. Nature Reviews Neuroscience 7: 583–590.
- Hall WD, Mant A, Mitchell PB, Rendle VA, Hickie IB, and McManus P (2003) Association between antidepressant prescribing and suicide in Australia, 1992–2000: Trend analysis. British Medical Journal 326: 1008–1011.
- Hickie I and Scott L (2007) Understanding Depression. Sydney, Australia: Educational Health Solutions.
- Hickie I, Naismith S, Ward PB, et al. (2005) Reduced hippocampal volumes and memory loss in patients with earlyand late-onset depression. British Journal of Psychiatry 186: 197–202.
- Highet NJ, Hickie IB, and Davenport TA (2002) Monitoring awareness of and attitudes to depression in Australia. Medical Journal of Australia 176: s63–s68.
- Kessler RC, Chiu WT, Demler O, and Walters EE (2005) Prevalence, severity and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 62: 617–627.
- Lopez AD and Murray CJL (1998) The global burden of disease, 1990–2020. Nature Medicine 4: 1241–1243.
- Mathers CD and Loncar D (2006) Projections of global mortality and burden of disease from 2002 to 2030. PLoS Medicine 3: 2011–2030.
- McGorry PD, Hickie IB, Yung AR, et al. (2006) Clinical staging of psychiatric disorders: A heuristic framework for choosing earlier, safer and more effective interventions. Australian and New Zealand Journal of Psychiatry 40: 616–622.
- McNair BG, Highet NJ, Hickie IB, and Davenport TA (2002) Exploring the perspectives of people whose lives have been affected by depression. Medical Journal of Australia 176: s69–s76.
- Pirkis J, Hickie I, Young L, et al. (2005) An evaluation of beyond blue: Australia’s National Depression Initiative. The International Journal of Mental Health Promotion 7: 35–53.
- Rush AJ, Trivedi MH, Wisniewski SR, et al. (2006) Bupropion-SR, Setraline, or Venlafaxine-XR after failure of SSRIs for depression. The New England Journal of Medicine 354: 1231–1242.
- State Government of Victoria Department of Human Services (2001) Current report – Mortality and Morbidity report and DALY worksheets 2001. http://www.health.vic.gov.au/healthstatus/bodvic/bod_current.htm (accessed January 2008).
- World Health Organization (2007) Statistical Information System. Ten statistical highlights in global public health. http://www.who.int/whosis/whostat2007_10highlights.pdf (accessed January 2008).
- Airan RD, Meltzer LA, Roy M, et al. (2007) High-speed imaging reveals neurophysiological links to behaviour in an animal model of depression. Science 317(819); 5 July 2007 (10.11126/science/ 1144400).
- Castren E, Voikar V, and Rantamaki T (2007) Role of neurotropic factors in depression. Current Opinion in Pharmocology 7: 18–21.
- Christensen H, Griffiths KM, and Jorm AF (2004) Delivering interventions for depression by using the internet: Randomised controlled trial. British Medical Journal 328: 265.
- Hickie I (2004) Treatment guidelines for depression in the Asia Pacific region: A review of current developments. Australasian Psychiatry 12 (supplement 1): s33–s37.
- Insel TR (2007) Shining light on depression. Science 317: 757–758.
- Jorm AF, Barney LJ, Christensen H, et al. (2006) Research on mental health literacy: What we know and what we still need to know. Australian and New Zealand Journal of Psychiatry 40: 3–5.
- Kessler RC, Berglund P, Demler O, et al. (2005) Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 62: 593–602.
- Kruijshaar ME, Barendregt J, Vos T, et al. (2005) Lifetime prevalence of estimates of major depression: An indirect estimation method and quantification of recall bias. European Journal of Epidemiology 20: 103–111.
- The Lancet Series on Global Mental Health: Article Collection (2007) http://www.thelancet.com/online/focus/mental_health/collection (accessed January 2008).
- Lopez AD, Mathers CD, Ezzati M, Jamison DT and Murray CJL (eds.) (2006) Global Burden of Disease and Risk Factors. New York: Oxford University Press.
- Mann JJ, Apter A, Bertolote J, et al. (2005) Suicide prevention strategies: A systematic review. Journal of the American Medical Association 294: 2064–2074.
- Patel V, Flisher AJ, Hetrick SE, and McGorry PD (2007) Mental health of young people: A global public-health challenge. Lancet 369: 1302–1313.
- Pezawas L, Meyer-Lindenberg A, Drabant EM, et al. (2005) 5-HTTLPR polymorphism impacts human cingulated-amygdala interactions: A genetic susceptibility mechanism for depression. Nature Neuroscience 8: 828–834.
- Pirkis J, Hickie I, Young L, et al. (2005) An evaluation of beyond blue: Australia’s national depression initiative. The International Journal of Mental Health Promotion 7: 35–53.
- Sanderson K, Andrews G, Correy J, et al. (2003) Reducing the burden of affective disorders: Is evidence-based health care affordable? Journal of Affective Disorders 77(2): 109–125.
- Sartorius N (2001) The economic and social burden of depression. Journal of Clinical Psychiatry 62(supplement) 15: 8–11.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.







