This sample Health Systems of South Asia Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Introduction
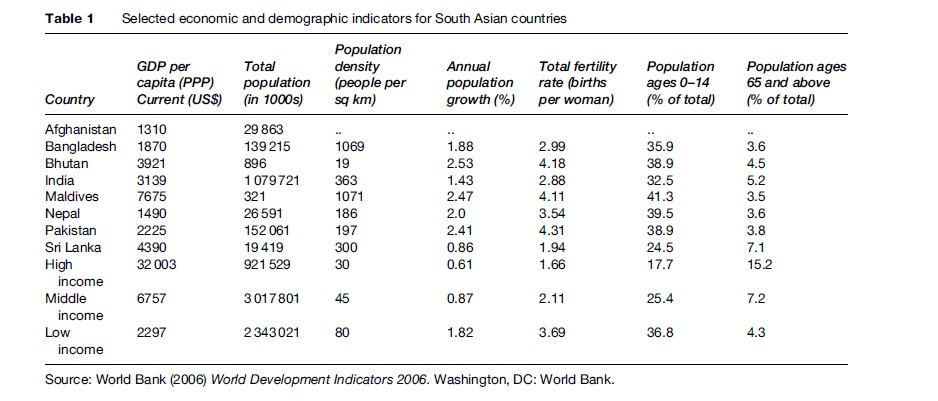
South Asia, as per the World Bank’s regional classification, consists of eight countries – Afghanistan, Bangladesh, Bhutan, India, Maldives, Nepal, Pakistan, and Sri Lanka. Three of the countries in the region – India, Pakistan, and Bangladesh – are ranked among the ten most populous countries in the world. All the countries in the region except Sri Lanka have higher than replacement fertility rates. The replacement rate is equal is to 2.1 births per woman (Table 1). The population age 65 years and above constitutes only 5% of the total population in South Asia, compared to 15.2% in high-income countries. South Asia is home to nearly half of the world’s poor. The poverty incidence (less than $1-a-day income) is estimated to be 30% in Bangladesh and India, 24% in Nepal, and 20% in Pakistan. The region has the second worst health outcomes, next only to sub-Saharan Africa. The region accounts for one-third of the world’s maternal deaths. However, the region also includes countries (e.g., Sri Lanka) and subnational areas in some countries (e.g., Kerala in India) that have health outcomes comparable to those in developed countries.
Health Status Of The Population
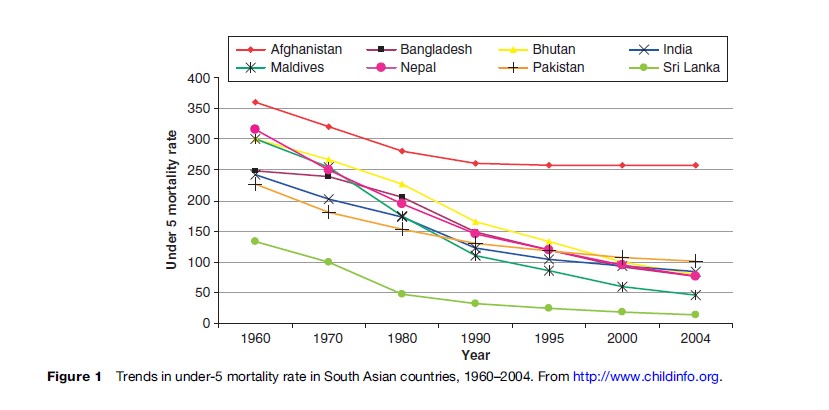
The average life expectancy at birth in South Asia is 63 years and ranges from 62 years in Nepal to 74 years in Sri Lanka (Table 2), lower than the average of 70 years in East Asia. Between 1960 and 2004, age 5 and under mortality rates per 1000 live births declined from 266 to 92 in the region, although the gains were not uniform across countries (Figure 1). Little improvement has been seen in the child survival status in Afghanistan since 1990.
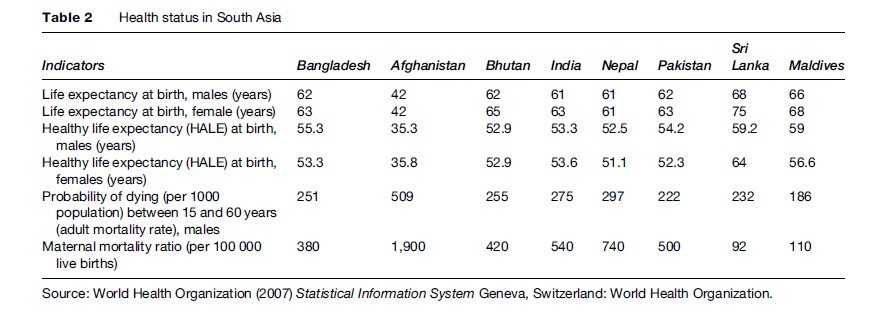
Though the maternal mortality per 100 000 births has been estimated to have declined from 870 in 1990 to 500 in 2000, the rate is still unacceptably high and is 25 times higher than that in the developed world. The lifetime risk of dying during pregnancy for a woman in South Asia is 1 in 43, compared to 1 in 30 000 in Sweden. However, the regional average hides considerable intercountry variations that range from as low as 92 in Sri Lanka to 540 in India and 1900 in Afghanistan (Table 2). The lifetime risk of dying during pregnancy in Afghanistan is one in six – one of the highest in the world. South Asia has the unfortunate distinction of having the lowest proportion of births attended by skilled health-care personnel, increasing from only 30% in the 1990s to 36% in 2004.
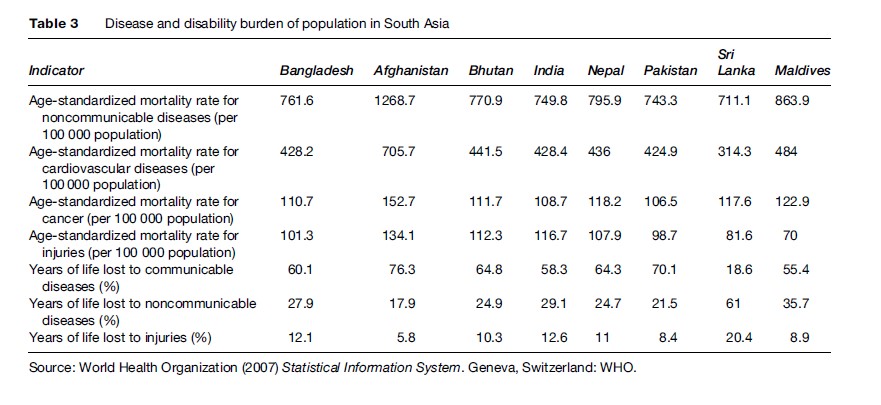
Rampant iron and other micronutrient deficiencies, combined with overall undernutrition, especially among the poor, is not only keeping children at an educational learning disadvantage from an early age: it is also leading to intergenerational transmission of poverty and other disabilities. Widespread undernutrition among women, including high rates of iron deficiency anemia, is of particular concern, especially among poor women. Almost 47% of the disability-adjusted life years (DALYs) lost in the region are accounted for by communicable, maternal, perinatal, and nutritional conditions. Infectious and parasitic diseases contribute to 23% of the DALYs lost, followed by neonatal (10%) and respiratory infections (9%). Communicable diseases contribute to the maximum years of life lost in all the countries in the region, except Sri Lanka. The brunt of communicable diseases is mainly borne by children, women, and marginalized sections of the population.
Infections such as tuberculosis (TB) continue to be the leading cause of death among young adults. Three of the 10 countries with the largest number of TB patients are in South Asia, with Afghanistan having the highest prevalence and mortality rate of 661 cases and 92 deaths, respectively, per 100 000 population. India carries the world’s greatest burden of TB cases. Though some improvement has been made in TB control, the situation is likely to be complicated by the spreading HIV epidemic. Over 2 million people are estimated to be coinfected with both HIV and TB as well as the emergence of drug-resistant strains in the region. In addition, a significant proportion of the regional population continues to live in malaria-prone areas with significant morbidity and mortality.
While South Asia is still grappling with control of traditional infectious diseases, it is being confronted with new emerging infectious diseases; the most obvious is HIV/AIDS. Over 5 million people in South Asia are living with HIV. Over 90% of those infected are living in India. Although the rate in the population at large is still low (0.9%), in absolute numbers due to its large population, India has one of the largest HIV-positive populations in the world, second only to South Africa. Other countries in the region, such as Bangladesh, Pakistan, and Nepal, have a low prevalence among the general population, but have significantly higher rates among subpopulations that are engaging in high-risk behaviors, such as injecting drugs with contaminated needles and high-risk sex behavior.
While the challenge of communicable diseases continues, the burden of noncommunicable diseases has also started to increase (40% of the DALYs lost), followed by injuries (12% of the DALYs lost) (Table 3). Other than Sri Lanka, all the other countries are in different stages of epidemiological transition of diseases, that is, from communicable to noncommunicable. Many of the noncommunicable diseases affect young and middle-aged populations, which adversely affects workforce productivity. Cardiovascular diseases, diabetes mellitus, and chronic obstructive pulmonary diseases have already reached epidemic proportions in India. Moreover, the burden of injuries is increasing in the region, especially those due to road accidents in the working-age population.
However, with better uptake of preventive services (e.g., immunization, clean water and sanitation, better nutrition, maternal services, etc.), the communicable diseases are relatively more concentrated among the poor, while the noncommunicable diseases are rising across all the socioeconomic groups, contrary to the commonly held view that noncommunicable diseases are diseases of the rich. A number of risk factors including tobacco and alcohol consumption are much higher in the poorest population in South Asia. This is leading to a double burden of communicable and noncommunicable diseases among the poor, which has the potential to accentuate the inequities in health outcomes. Though the consumption of ‘manufactured’ cigarettes – a major form of tobacco consumption in developed countries – is relatively low in South Asia (only 3–4% of world comsumption compared to South Asia’s share of 23% of the global population), tobacco consumption is highly prevalent in South Asia and takes many other forms and as handrolled cigarettes (bidis), chewing tobacco inside a betal leaf, etc. Smoking prevalence varies from 18% in Nepal to 26% in India.
Status Of Underlying Determinants Of Health
Water Supply And Sanitation
Access to clean drinking water and improved sanitation still remains suboptimal in South Asia. However, this access varies across countries, with Afghanistan having the lowest access to improved water sources (13%) and sanitation (8%). Ninety percent of the population in Pakistan has access to improved water supply, and 91% of the population in Sri Lanka has access to improved sanitation. Rural areas in general have poorer access to both clean drinking water and improved sanitation.
Education
South Asian health systems continue to be challenged by massive educational deprivation, with 56% of women in the region being illiterate in 2004. Female education and literacy have many secondary health-enhancing effects both on health systems and health outcomes. With the exception of Sri Lanka (89%) and Maldives (96%), all other countries in South Asia have less than 50% female literacy rates, with the lowest rates observed in Afghanistan (13%), followed by Nepal (35%), Pakistan (36%), and India (48%). Both the primary school enrollment and school completion rates continue to show widespread gender disparities at the expense of female students.
Health Systems In South Asia
Organization Of Health Systems
All countries in the region have a national ministry of health. However, the health systems are decentralized in line with the overall public administration decentralization (e.g., Bangladesh and India). Decentralization has, however, led to overlapping roles and responsibility across different administrative levels. Primary health-care approaches have been adopted to deliver personal curative and individual preventive health services such as family planning services, maternal health services, and childhood immunization services. Certain vertical health programs sponsored by central health agencies are embedded within the overall context of an integrated primary health-care system.
Infrastructure And Human Resources
Most of the countries have a relatively well-developed hierarchical network of health facilities. The lower-level health facilities are often not fully functional or reliable as the resources are quite thinly spread, and the population served by the most peripheral health facility vis-a`-vis available staff is relatively high. For example, in India the most peripheral health facilities (subcenter) are staffed by a single female paramedical health worker who serves a population of 5000. The situation is compounded by a high level of vacancies. In almost all the countries in South Asia, household outreach either through community or government health workers stationed at the lowest-level health facilities is common, and the effectiveness of these services varies across countries.
Almost all the countries have tried community mobilization using community health workers.
Although in aggregate, the availability of health manpower in South Asia is relatively better than that in sub-Saharan Africa, again, it varies greatly across countries. The number of physicians per 1000 population varies from just 0.2 in Afghanistan to 0.9 in Maldives. Similarly, the number of nurses per 1000 population varies from 0.14 in Bangladesh to just more than one in Maldives and Sri Lanka. The number of hospital beds per 10 000 population ranges from just 1.5 in Nepal to 29 in Sri Lanka.
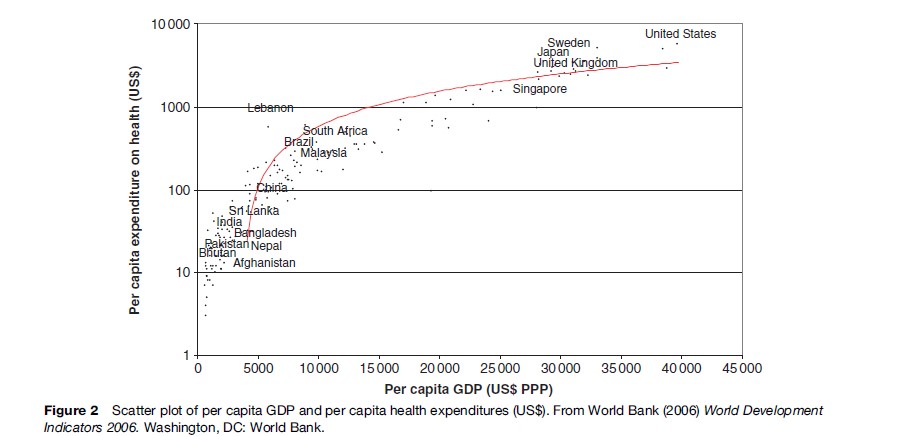
Health Expenditures
Compared to double-digit expenditures on health as a percent of gross domestic product (GDP) in high-income countries, the percent of GDP spent on health varied from 2.4% in Pakistan to 6.2% in Maldives (Figure 2). In 2005, the total public health spending as a percent of general government expenditures was less than 10% in most countries except in Maldives (13.8%). Among the three largest countries, it varied from 2.6% in Pakistan to 3.9% in India to 5.8% in Bangladesh (Table 4). Even in absolute terms, the per capita expenditures on health in South Asia were suboptimal. With the exception of Maldives, all other countries in South Asia had per capita expenditures on health less than $31 (U.S.), which is one one-hundredth of what is spent in a high-income country. Afghanistan, Bangladesh, Bhutan, and Nepal relied heavily (>10% of total health expenditures) on external sources.
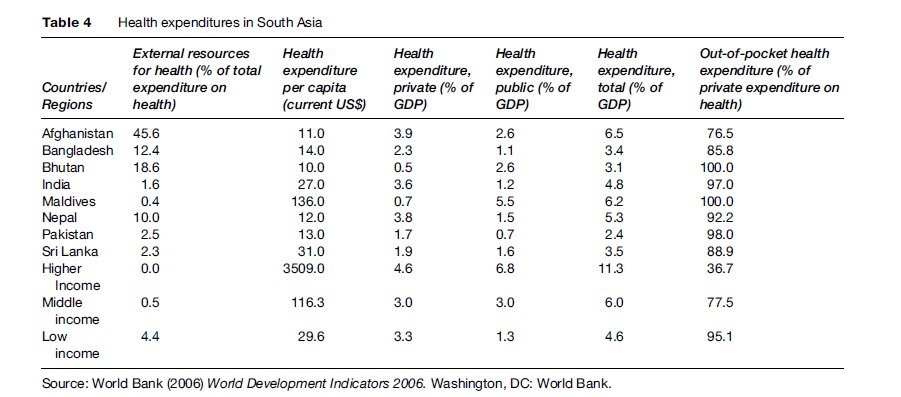
Health systems in South Asia are dominated by private sector financing. Except in Bhutan and Maldives, private expenditures on health exceed public expenditures: in India they are almost three times the public expenditures, and more than twice those in Bangladesh and Nepal (see Table 4). The proportion of private health expenditure to the total health expenditure in this region surpasses the proportion of private health expenditures in most countries of the world, including the United States.
In most of the South Asian countries, more than 90% of the total private expenditures on health come from out-of-pocket expenditures, with the exception of Bhutan and Maldives. Private prepaid plans as a percent of private expenditure on health are almost negligible. Not surprisingly, catastrophic expenditures on health care are one of the major reasons for impoverishment in the region.
The private sector is a major provider of health services, for example, personal curative services, which include services for treatment of diarrhea and childhood pneumonia, malaria, TB, and so on. In most of the South Asian countries, the private sector is very diverse, largely unregulated, and works in an uncoordinated manner in comparison to the public sector. The private sector has made curative services more accessible to the population but has been blamed for many adverse outcomes such as the development of drug resistance against TB and malaria. The private sector also does not participate in the diseases surveillance network, causing a major bottleneck in dealing with early detection of epidemics.
Use And Access To Health Services
The overall use of health services as measured by use of skilled delivery care and access of care for childhood fever remains rather low as shown in (Tables 5 and 6). Less than 10% of all births take place in health facilities in Bangladesh and Nepal. Similarly, health care was sought for only 18% and 25% of children with fever in Bangladesh and Nepal, respectively.
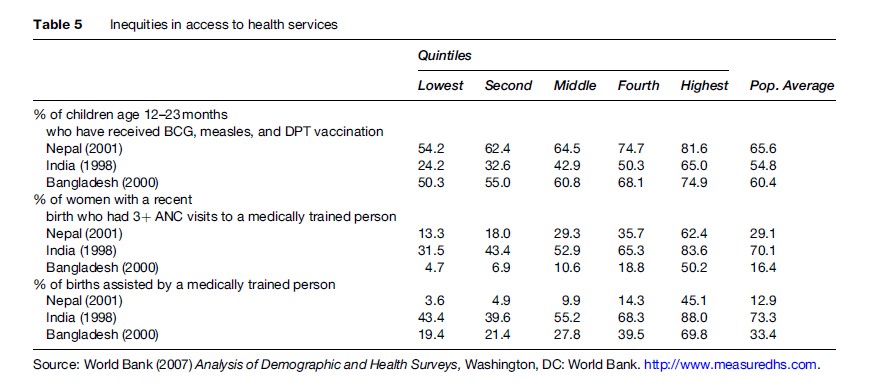
In addition to lower overall use of services, there are significant disparities in access to health services as measured by the use of different health services such as childhood immunization, antenatal care and skilled delivery care in different population quintiles based on household wealth (Table 5). Within countries, the presence of a skilled attendant at delivery is the most inequitably distributed indicator (Table 6).
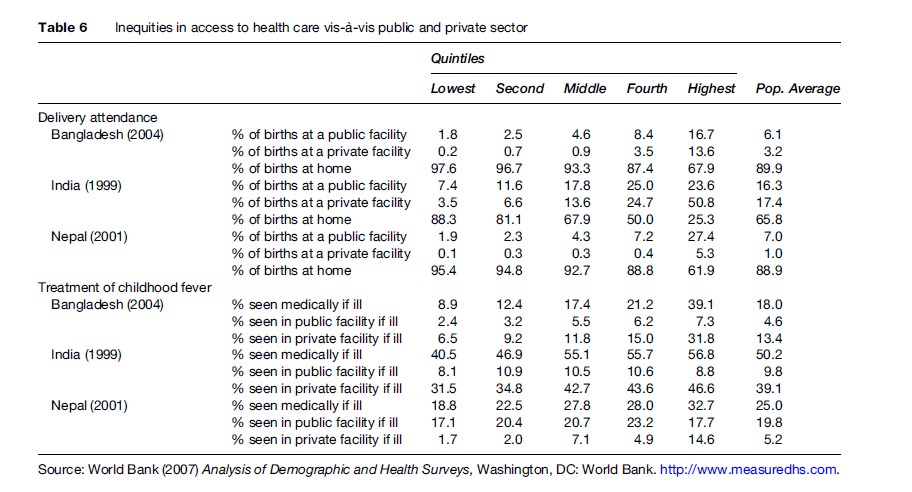
Another characteristic feature of use of health services in South Asia is the relatively higher use of private health facilities among those who chose to seek care. For example, in India, almost half of all institutional deliveries takes place in private health facilities (17.4% in private versus 16.3% in public, see Table 6). In general, though a relatively higher proportion of people in the wealthier population quintiles use the private facilities, the use remains substantial even in the lower socio-economic quintile of the population. For example, in India and Bangladesh, the reported use of private health facilities for treatment for childhood fever was almost five and three times, respectively, that of public health facilities (Table 6).
Health Systems Performance
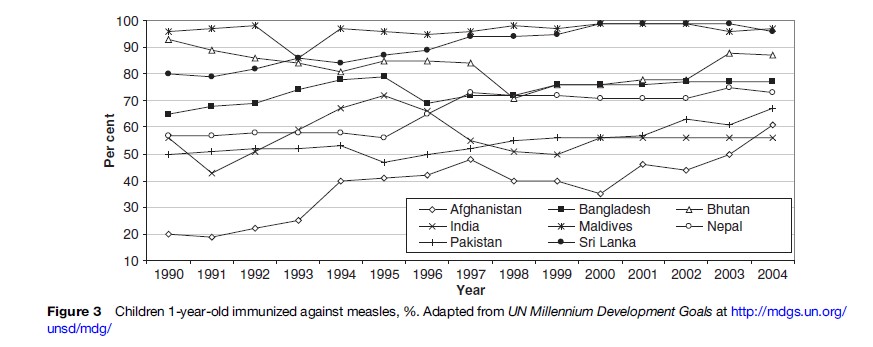
The World Health Report published by the World Health Organization in 2000 compared the relative performance of various health systems worldwide, based on key functions of the health systems (e.g., oversight, investment and training, provision, financing) and objectives of the health systems (e.g., responsiveness and fairness). All the South Asian countries except Sri Lanka and Bangladesh (ranked 76 and 88, respectively) were ranked in the bottom half of 184 countries included in the analysis (India, 112; Pakistan, 122; Bhutan, 124; Maldives, 147; Nepal, 150). Childhood immunization is an important service delivered by public health systems in the region, for which data are available over the past decade. Figure 3 shows the trends in measles immunization among 1-yearold children in South Asian countries. Afghanistan, India, and Pakistan consistently have been the bottom performers throughout the last decade. South Asia still has a long way to go to meet health-related Millennium Development Goals (MDGs) (Figure 3).
Issues And Challenges Facing South Asia’s Health Systems
Institutional And Governance Issues
Although more financial investments are needed in almost all the South Asian countries to improve coverage and quality of services, improved governance of public health institutions can lead to further efficiency gains and effectiveness, even at current investment levels. The general malaise of rampant absenteeism in public health facilities, indulgence of public health workers in private practice during official duty hours and/or after duty hours (moonlighting), and use of public facilities to further private practice continue to undermine governments’ efforts to increase access of critical health services, especially to disadvantaged sections of the population. Hence, the governance issues should be a greater priority and addressed urgently to ensure greater discipline among the health workforce and to increase their accountability to the end users.
Unlike banking and finance sectors, in which focused reforms can yield quick results, governance of health and education sectors is harder to improve because of the geographically dispersed nature of the services, large workforce, various layers of hierarchies, political nexus of lower officials with local politicians, and lack of a management group distinct from the technical one. The lack of a separate managerial body for public health is a major constraint in improving governance of the health sector in South Asian countries. It is therefore paramount to change the service rules and regulations to create a separate management team for the health department, in which technical staff could opt for managerial work (with thorough management training) through lateral entry at various stages of their careers.
The governments in the region appear to be overwhelmed by the dual task of both financing and providing services. They should ‘steer’ and delegate the responsibility of ‘rowing’ to either the private sector or lower tiers of government, using appropriate performance-based incentive systems based on health outcomes and effective monitoring and evaluation systems to ensure performance-based contracts are achieved. Innovative public-private partnerships and public-public partnerships would increase the effectiveness of public expenditures on public health.
Delegation Of Service Delivery
Currently health services are too dispersed to be monitored effectively from a central remote point, especially when managerial abilities in health departments remain in question. Delegation of service delivery to local governments is critical for improving accountability and responsiveness of health services. Health workers potentially would be more accountable to the needs of the public if they had greater access to local politicians who could in turn exert more pressure on the local functionaries of health departments. Concerted efforts are needed to improve the managerial and leadership capacity at the central and other levels of health services, and local governments need to take greater responsibility for providing stewardship to the public health service provision.
Separation Of Preventive And Curative Health
In this region, the work of preventive public health is organized under two departments: the public health engineering department and the health department. The public health engineering department, contrary to what the name suggests, mostly supplies drinking water. The municipalities and other local bodies are engaged in sewer and solid waste management. Most of the other preventive public health work is done by the health departments. In almost all cases, there is no clear separation of preventive and curative health functions in these departments. The health workers have a tendency to gravitate toward dispensing more curative health services, due to incentives provided by curative care seekers in the form of unregulated yet widely prevalent out-of-pocket payments (private practice). Curative care is clearly a ‘private’ good and generally of an urgent nature, which compels the care seeker to pay for the services.
Preventive health services, in contrast, are generally a ‘public’ good and less likely to lead to private practice or out-of-pocket payments. Thus, the preventive public health functions are undermined by a permissive environment of rampant, unregulated private practice. Preventive public health services get less scrutiny at the local level because of the largely ‘public good’ nature of the work. Also, the significance of preventive public health in largely illiterate, rural areas remains unclear.
Regulation Of The Private Health Sector
The failure of the public health sector to provide quality, reliable, and predictable services has compelled the populations of South Asian countries to seek care from the private health sector mainly using out-of-pocket payments. Over the years, this sector has become the dominant provider of health services in the region, unlike any other part of the world, even surpassing the most market-oriented countries. To cater to such a wide range of population groups with varying abilities to pay out-of-pocket, a highly heterogeneous private health sector has emerged in these countries ranging from the most informal, unqualified private practitioners to highly sophisticated modern health-care workers at a level of quality equivalent to that in developed countries.
The lower end of the spectrum of the private health sector includes over-the-counter dispensation of drugs by pharmacists without prescriptions for common symptomatic illnesses, untrained or minimally trained health workers, or traditional healers indulging in unchecked use of allopathic drugs. Another distinctive feature of the private health sector in South Asia is the blurred distinction between the public and private health sectors themselves. Depending on the level of governance and managerial effectiveness, public health workers indulge in private practice during official working hours using public health facilities. Demand for out-of-pocket unregulated payments by public health workers providing curative services, especially involving invasive procedures or inpatient care, has created greater barriers for the poor to access public health care in the region.
The largely unregulated mushrooming of the private health sector has led to a number of challenges. Questions abound concerning the quality of care and the repercussions of care provided by the ‘informal’ sector. Also, as stated previously, there is much concern over the emergence of various public health risks, such as drug resistance due to rampant over-the-counter dispensation of medicines without prescriptions and irresponsible use of medicines. This has led to a call for government regulation of the private health sector, which remains challenging given the weak capabilities of the governments. Hence, solutions for private health sector regulation should also be explored in quasi-government or nongovernment institutional frameworks. Accreditation, peer reviews by private health sector associations under the overall stewardship of national, provincial, and autonomous districts are some of the methods that could be explored.
Use Of Traditional Or Indigenous Systems Of Medicine
South Asian countries are also characterized by the use of formal indigenous systems of medicine, which strengthen primary health-care systems; the most important of these include Ayurveda, Siddha, Unani, and homeopathy. In India, there are more than 120 undergraduate colleges, mostly in the public sector, training more than 4000 doctors each year in the Ayurveda system. The practitioners of traditional systems of medicine make up an important part of the private health sector in South Asia. Due to the lack of clear recognition and commitment by the government, and distrust among health workers trained in traditional medicine and in the allopathic system, the potential of traditional medicine systems to strengthen primary health care, especially in rural areas, has not been fully exploited. However, experimentation with using traditional medical practitioners in several primary health-care settings in South and East Asia has demonstrated that they are much more willing to work in these settings in rural areas – and thus are able to act as a link between the local population and the health systems – than the allopathic practitioners, who seek higher specialization and prefer urban locations. Training of traditional medical practitioners in basic concepts of primary health care and integrating them with the primary health-care system in the country can improve primary health-care delivery.
Improving The Public Health Sector
The problems of improving the efficiency and effectiveness of the public health sector are too deep-rooted for any quick-fix solutions. Institutional and governance reforms are essential. One of the most critical tasks is to build a strong core of managers and groom future public health leaders. Supervision, incentive structures, and motivational aspects need to be carefully addressed to ensure greater accountability and responsiveness from the health functionaries. Critical gaps relating to human resources and infrastructure also need to be addressed. Because there is a vibrant and strong private health sector, the governments should explore options for private provision through public financing. The unbundling of preventive and curative services and contracting out of services through competitive processes to competent private health sector groups could achieve efficiency and effectiveness.
Because South Asia’s health systems are characterized by unregulated out-of-pocket expenditures, there is growing evidence that catastrophic illnesses are leading to debt traps and further impoverishment. There is certainly a need for the creation of ‘sickness funds,’ especially for the poor, which could be managed by local governments or autonomous bodies who could then negotiate with local providers for services. Other steps to introduce ‘risk pooling,’ including social and health insurance, are also critical. Other challenges include preparing these health systems for eminent and ongoing epidemiological transition from communicable to noncommunicable diseases.
Conclusion
South Asia has made impressive gains in health outcomes in the past few decades. However, the public health systems have not kept pace with the demand, leading to unregulated growth of the private health sector. The public health systems are plagued with fundamental weaknesses coupled with a low level of investments. Without improving the institutional and governance framework of the health systems in the region, the effectiveness of further investments will remain questionable. Alternative options may include private provision of services with public financing. In the absence of controls to enable the poor access to needed health care, the gap between the rich and poor in access to overall health care is going to expand unless the public health sector starts delivering better services to and thus better outcomes for the poor. These differentials in access to health care can lead to resentment and social disorder. Poor health will be a barrier to higher labor productivity. As epidemiological transition grows, noncommunicable diseases costly to treat will be catastrophic to many households in the region.
The governments in South Asia should introduce risk pooling to mitigate these catastrophic health expenditures. In all, the South Asia health systems need greater attention by genuine, concerted efforts from their governments.
Bibliography:
- Berman P (ed.) (1995) Health Sector Reforms: Making Health Development Sustainable. Boston, MA: Harvard University Press.
- Peters DH, Yazbeck AS, Sharma RR, Ramana GNV, Pritchett LH, and Wagstaff A (2002) Better Health Systems for India’s Poor: Findings, Analysis, and Options. Washington, DC: World Bank.
- Rhode J and Vishwanathan H (1995) The Rural Private Practitioner. New Delhi, India: Oxford University Press.
- Wang J, Jamison DT, Bos E, Preker AS, and Peadody J (1999) Measuring Country Performance in Health: Selected Indicators for 115 Countries. Health, Nutrition and Population Series. Washington, DC: World Bank.
- World Bank (1993) World Development Report 1993: Investing in Health. New York: Oxford University Press.
- World Bank (2004) World Development Report 2004: Making Services Work for Poor People (World Development Report). Washington, DC: World Bank.
- World Health Organization (2000) World Health Report 2000 – Health Systems: Improving Performance. Geneva, Switzerland: World Health Organization.
- World Health Organization (2007) Statistical Information System. Geneva, Switzerland: WHO.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








