This sample Nutrition and HIV Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Introduction
The human immunodeficiency virus (HIV) seems to have originated from simian immunodeficiency virus (SIV) among monkeys in Central Africa, where SIV crossed the species barrier and caused infection in humans exposed when hunting monkeys for meat. When first described in Africa, the advanced stage of HIV infection – acquired immune deficiency syndrome, or AIDS – was called ‘slim disease,’ due to the pronounced wasting that is a cardinal manifestation, especially in individuals with poor dietary intake before and after being infected.
Sub-Saharan Africa remains the hardest hit part of the world, particularly Southern Africa. Of, the 33.2 million individuals living with HIV infection in 2007, 22.5 million (67%) live in Sub-Saharan Africa. Of a global total of 2.1 million AIDS deaths and 2.5 million new HIV infections in 2007, sub-Saharan Africa accounted for 1.6 million and 1.7 million, respectively.
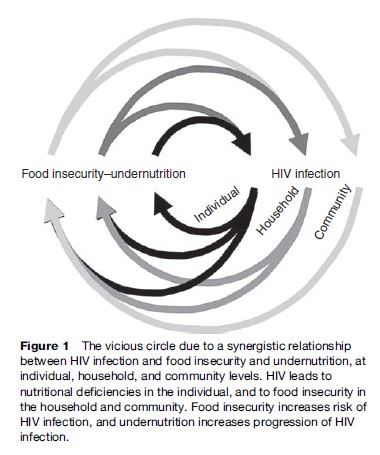
In low-income populations, nutrition and HIV infection are closely linked, at the level of the individual, the household, and the community. Thus, food insecurity and undernutrition may be determinants as well as consequences of HIV infection (Figure 1).
Even in high-income populations, with well-functioning health systems and access to antiretroviral (ARV) treatment (ART), some patients may not have a diet meeting the nutritional requirements. This could be because the health system fails to provide nutritional advice to the patient, and the patient lacks knowledge or resources to obtain an adequate diet. Many organizations and Internet sites provide information on the importance of diet, and people living with HIV often take nutritional supplements, herbs, or other complementary food-based therapies, although the evidence for efficacy and safety is lacking.
Nutrition And Infections
Adequate intake of energy and nutrients is necessary to maintain health. The macronutrients (i.e., carbohydrates, protein, and fat) provide energy and the micronutrients (i.e., vitamins and minerals) are essential for general and specific metabolic functions. A diet that is inadequate in energy and nutrients fails to sustain optimal growth of children and maintain weight and body composition of adults, and impairs specific body functions.
In low-income populations, the typical diet is based on a starch-rich staple, such as cereals, tubers, or legumes, with few vegetables and fruits, and little, if any, animal foods. Such a diet has a low energy and nutrient density. The bulkiness of the diet renders it difficult to meet the energy and nutrient requirements, even if the amount of food is adequate. In addition, the quality of the diet is often low. Vitamin A, for example, is rarely available as preformed vitamin A, found in animal foods, but mainly as so-called provitamin carotenoids from plant foods. The conversion of provitamin A carotenoids to vitamin A in the body is less efficient than previously believed, and further impaired by deficiency of other nutrients. Iron is mainly available as the poorly absorbable nonheme iron from plant sources, and rarely as heme iron from animal foods. Furthermore, the staple foods contain high levels of phytic acid and other antinutrients, which bind essential minerals like zinc and iron and prevent their absorption. In addition to the low intake and bioavailability of micronutrients, a high burden of infectious diseases increases the requirements and considerably contributes to the high prevalence of deficiencies.
Women and children are particularly vulnerable to nutritional deficiencies. Since women often have inadequate dietary intake before and during pregnancy, fetal growth will be retarded and the child born with low weight and inadequate nutrient stores. Although exclusive breast-feeding up to 6 months of age is recommended by the World Health Organization (WHO), most children receive water, tea, cows’ milk, porridge, and so on, from the first few weeks of life. The combination of early nutritional deficiencies and contaminated liquid and solid foods increases the risk of diarrhea and pneumonia, which further impairs the nutritional status of the child.
Deficiencies of vitamin A, iron, and zinc, as well as other micronutrients, are widespread in low-income populations. Lack of micronutrients may impair specific body functions, such as cognitive functions, vision, production of red blood cells, as well as immune functions. Some micronutrients have antioxidant (e.g., vitamins C and E, and selenium) or prooxidant (e.g., iron) properties, which means that they are able to either counteract or generate, respectively, harmful oxidative stress. Cheap and feasible public health interventions exist, whereby the intake of micronutrients, in contrast to macronutrients, can be increased in populations. These include dietary diversification, food fortification, food modification, and supplementation. In addition, interventions to prevent and treat common infections serve to prevent further increases in requirements.
Immune Functions And Resistance To Infections
Immune suppression caused by lack of nutrients has been called nutritionally acquired immunodeficiency syndrome, or NAIDS. Lack of zinc, of which only about 1 mg is needed every day to replace losses, leads to virtual disappearance of the thymus, a key immunological organ. Thus micronutrient deficiencies often increase risk and severity of infectious diseases. Since infections also impair nutritional status, then we have a synergistic two-way relationship or a vicious circle (see Figure 1). Nevertheless, even if a specific nutritional deficiency impairs immunity, administration – especially if unphysiological doses or routes are used – of that nutrient may favor the pathogen more than the host, and hence increase the risk and severity of infectious diseases. For example, parenteral and even oral administration of iron may stimulate growth of bacteria or parasites and lead to increased morbidity. Vitamin A, for example, is essential to a range of immune functions, and large randomized trials have found that periodic administration of vitamin A capsules to children under 5 years reduces mortality by 23–30%. Vitamin A supplementation, given in large doses two or three times per year, is therefore recommended by the WHO. Given the considerable effect of vitamin A on mortality, the adequacy of dosing only a couple of times per year, often in combination with national immunization days, and the low price per capsule, makes vitamin A supplementation one of the most cost-effective health interventions.
Zinc supplementation may prevent diarrhea and pneumonia in populations with an inadequate zinc intake, and has also been shown to reduce the duration and severity of diarrhea when given therapeutically. In contrast to vitamin A, zinc has to be taken frequently if not daily, since there are no body stores. Thus, zinc supplementation may be feasible in the treatment of children hospitalized or attending health facilities due to diarrhea but is not a feasible intervention in the prevention of diarrhea and pneumonia, even though these diseases account for a large proportion of the 10 million child deaths each year.
Nutrition And HIV Infection
The biological two-way relationship between nutrition and HIV infection is complex.
HIV Infection Impairs Nutritional Status
HIV infection has direct effects on nutritional status, in addition to the effects on food security described later. HIV infection increases nutritional requirements by reducing absorption and increasing utilization and loss of nutrients, and resting energy expenditure. Yet, the intake of nutrients and energy may be reduced, due to loss of appetite. Depending on the dietary intake of nutrients and energy, micronutrient status may be impaired and fat and particularly lean body mass lost even at early stages of the infection. With more advanced HIV infection, when opportunistic and other infections occur, resting energy expenditure is further increased, whereas food intake may be further reduced, due to painful sores and infections in the mouth and esophagus.
If the additional energy requirements are not met, then weight will be lost, unless physical activity is reduced, which may impair household food security (see Figure 1).
If the additional nutrient requirements are not met, then specific deficiencies will eventually occur, or existing deficiencies will become exacerbated, which will impair important body functions, including maintenance of lean body mass and immune functions. An exception is iron. Although absorption of iron may be impaired, even early HIV infection results in anemia of infection, which is due to suppression of the production of red blood cells in the bone marrow. But red blood cells will continue to age, and eventually be engulfed by white blood cells and taken to the stores, where iron will accumulate as it is now longer incorporated into new red blood cells.
Energy requirements are estimated to be 10% higher during asymptomatic HIV infection, to maintain body weight and physical activity, and they are 30% higher during symptomatic HIV infection (WHO, 2003). In contrast, protein requirements do not seem to be increased. The requirements for most vitamins and minerals are increased, and it is recommended that patients with HIV eat a healthy diet. In practice, many patients are advised to take a daily supplement containing one recommended dietary allowance (RDA) of the essential vitamins and minerals, except iron.
But the extent to which the requirements are increased by HIV infection is still not clear, as it will be different for different micronutrients and depend on the stage of HIV infection. Nevertheless, recommendations should not only be based on which intakes are necessary to avoid deficiency, but on which intakes give optimal health, and prevent progression of HIV infection.
Nutrition Affects HIV Progression And Transmission
In HIV-infected individuals, micronutrient deficiencies and iron loading may accelerate progression of HIV infection, as shown in the conceptual framework in Figure 2. Deficiencies of antioxidant vitamins and minerals and accumulation of the prooxidant iron could lead to oxidative stress, which is known to activate a transcription factor that increases replication of HIV, which results in increased HIV progression. The iron accumulation may also result in flare-up of latent tuberculosis (TB) and possibly other infections, which stimulate HIV replication. Deficiencies of micronutrients essential to immune functions lead to NAIDS, which could contribute to the risk of coinfections, and to the decline in the number of CD4þ cells, that is, the cells infected and destroyed by HIV. Data from laboratory and clinical studies support this conceptual framework. Accordingly, it is likely that iron supplementation is harmful, as it may increase HIV progression. Yet, iron supplementation is given routinely to pregnant women seeking antenatal care, and occasionally to TB patients presenting with anemia, even in settings where HIV infection is prevalent. It should be a research priority to assess the effects and safety of iron supplementation to people with HIV infection.
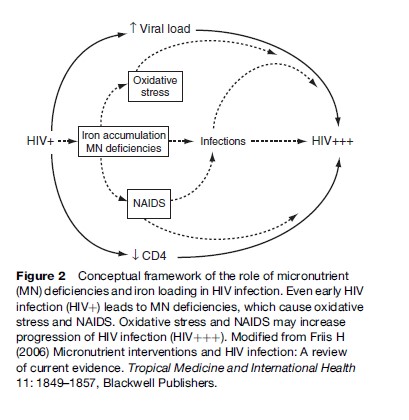
In contrast, data from randomized, placebo-controlled trials document a beneficial effect of micronutrient supplementation during HIV infection. For example, among HIV-infected pregnant women in Tanzania not receiving ART, a daily supplement containing high doses of vitamins B, C, and E was shown to increase CD4þ count and to reduce HIV load. After 2 years, those receiving the multivitamins had 29% lower risk of progression to or dying from AIDS (Fawzi et al., 2004). Similarly, a trial among adult Thai males and females with HIV infection found that a daily supplement containing approximately one RDA of a range of micronutrients reduced mortality ( Jiamton et al., 2003). A supplementation trial was also conducted among adult Tanzanian patients with pulmonary TB, of which almost half had HIV coinfection. Supplementation with zinc and other micronutrients in combination, but neither alone, during 8 months of TB treatment considerably increased weight gain and reduced mortality (Range et al., 2005).
This study demonstrates that treatment of an infection, in this case TB, does not eliminate the need for nutritional support, as it is often assumed. In fact, if the infection has resulted in a growth or weight deficit, then treatment, by allowing a growth spurt or weight gain, considerably increases nutritional requirements. If these requirements are not met, then it is likely that the weight gain will result in fat rather than lean body mass. It is also likely that it may exacerbate NAIDS, and potentially worsen the outcome of the infection being treated or of coinfections, such as HIV. Thus, nutritional support providing multiples of the RDA may be needed to meet the requirements during the initial phase of the treatment. Currently, nutritional assessment, advice, and support are rarely integrated in the management of HIV infection and TB in low-income countries.
To the extent nutritional deficiency contributes to progression of HIV and increase in HIV load, then it is also likely to be a determinant of infectiousness, and hence, of mother-to-child or sexual transmission. As such, the supplement containing vitamins B, C, and E, mentioned previously, was also found to reduce mother-to-child HIV transmission, although only among women with signs of poor health. Despite initial observational data suggesting that vitamin A supplementation might reduce mother-to-child HIV transmission, later data from randomized, controlled trials found no effect of vitamin A supplementation in two trials, and increased transmission in a third. The vitamin A supplement contained both preformed vitamin A and provitamin A carotenoids, and it is not clear which of these compounds caused the increase in transmission, and why it was not the case in one of the other trials using a similar intervention (Friis, 2006).
Due to the importance of various nutrients to epithelial integrity and mucosal immunity, it is likely that deficiencies may also affect susceptibility to infection, when exposed to HIV. However, there are currently no data to confirm this.
Nutrition And ART
With access to ART, also for HIV-infected individuals in low-income countries, the role of nutrition–drug interactions becomes increasingly important. According to current treatment guidelines, an HIV-infected individual is only eligible for ART when CD4þ counts are below 350. Since poor nutritional status is widespread even in uninfected individuals, and deteriorates with progression of HIV infection, it is obvious that an HIV-infected individual is in a poor nutritional status at the start of treatment. It is likely that nutritional deficiencies will affect absorption and metabolization of one or more of the two to three different drugs given, and hence affect either efficacy or toxicity of the drugs. Indeed, among patients on ART, low body mass index at the start of treatment has been found to be a predictor of mortality (Paton et al., 2006). Furthermore, it is known from Western countries that some of the ARV drugs affect lipid metabolism, and cause maldistribution of fat (i.e., lipodystrophia) and metabolic syndrome with a high risk of coronary heart disease and diabetes. It is unknown to what extent prior undernutrition and inadequate diet during treatment affect the risk of lipodystrophia and metabolic syndrome.
Breast-Feeding And HIV Infection
Breast-feeding is the healthiest infant feeding practice (Figure 3). The WHO recommends that infants are exclusively breast-fed, that is, given breast milk and nothing else, for the first 6 months of life. Infants should then continue breast-feeding, while also receiving complementary foods, into the second year of life. These recommendations are based on the greater survival of breast-fed, compared with non-breast-fed, infants, in low-income countries (WHO Collaborative Study Team, 2000), but there is also evidence from industrialized countries of improved health. HIV can be transmitted from mother to child through breast milk, but there are data suggesting that early exclusive breast-feeding is associated with a lower risk than mixed feeding (Coutsoudis et al., 2001).
The WHO therefore recommends HIV-infected mothers exclusively breast-feed their infants ‘‘for the first six months of life unless replacement feeding is acceptable, feasible, affordable, sustainable and safe’’ (WHO, 2007: 1). It is emphasized that the risk of HIV infection must be balanced with the risks associated with artificial feeding, and this must be done for each HIV infected woman on an individual basis.
With the increasing availability of perinatal ART in Africa, breast-feeding is becoming the major mode of mother-to-child HIV transmission (Figure 4). The WHO recommendation presents a major challenge because one feeding practice is not universally recommended. Healthcare staff and mothers have to balance the risk of transmitting HIV through breast milk with the risk of infants dying from other infections associated with not breast-feeding.
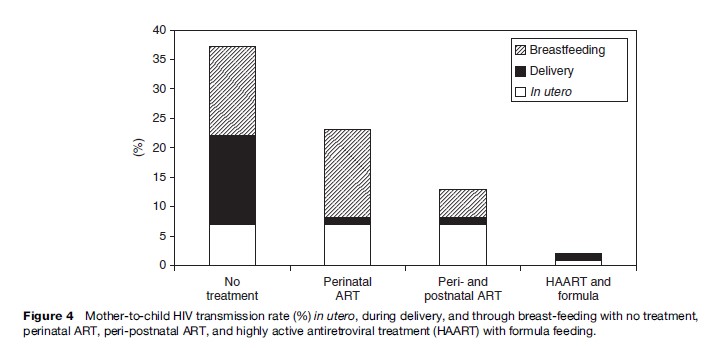
Several approaches to make breast-feeding by HIV-infected women safer have been investigated but their potential for being scaled up to larger programs is not yet known. One type of approach involves heat or antiviral treatment of expressed breast milk to destroy the virus without destroying nutrients or immune factors in the milk (Israel-Ballard et al., 2005). Another type of approach is to provide ART for the mother or infant during several months of lactation and then cease breast-feeding early, around 6 months (Thior et al., 2006).
Although there have been concerns that breast-feeding may have adverse effects on the health of the mother, possibly as a result of the nutritional stress of lactation, in general, research has not borne this out. As for all lactating women, HIV-infected women who choose to breast-feed should receive appropriate nutritional, medical, and psychosocial support.
The infant feeding advice for HIV-infected women is dependent on the woman’s environment and individual circumstances. Even within a health district there may be differences in the ability of individual women to purchase and safely prepare formula or other replacement foods. The recommended advice also changes fairly rapidly with time as new drugs become available and new strategies are shown to be effective. Health practitioners need to understand and be able to explain the issues associated with both breast-feeding and replacement feeding well enough to guide women in making individual informed choices. For some women, ‘‘acceptable, feasible, affordable, sustainable, and safe’’ infant foods may be available from birth, for others from 6 months, and for women in the poorest, most remote areas, not until even later, if at all. Communicating this advice is challenging and time consuming, especially in a busy maternal and child health clinic. In practice, HIV-infected women in wealthy industrialized countries are recommended to formula-feed, women in the poor rural areas of Africa are recommended to exclusively breast-feed and women in middle-income communities receive variable guidance, depending on the particular health worker and how busy she is at the time, concerning a very difficult choice.
Food Security And HIV Infection
Agriculture is the mainstay of the livelihoods of the majority of people affected by HIV globally. HIV is significantly impacting agriculture, but the interactions go two ways (see Figure 1). The structure of rural communities, the way they govern themselves, the livelihoods on which their households depend, all affect the risks of being exposed to HIV.
The risks people face of contracting HIV will be governed partly by the nature of the livelihood system on which they depend. After HIV has entered a community, the type and severity of its impacts on assets and institutions is then governed by the vulnerability of the system. These impacts will in turn determine the responses that households and communities adopt to deal with this threat. Responses lead to certain outcomes (nutrition and food security being among them) that themselves condition future susceptibility and vulnerability. And so the circle turns.
Food Insecurity Increases Risk Of HIV Infection
Inequalities with respect to gender, socioeconomic status, class, caste, and religion are central to the risks people face. Gender inequity shapes power relations, sexual relations, and access to resources, opportunities, and assets including land. It thus also shapes the relative risks and vulnerabilities that women face. Such socioeconomic vulnerability may lead a woman to exchange sex for food or cash, drastically increasing her risk of becoming infected.
Mobility is another risk factor. Many of the points of intersection between households and services represent conduits for the spread of infection into or out of communities. Migration, an important consequence of unequal socioeconomic development between urban and rural areas, is an important factor in HIV transmission. Consider an agricultural commercialization policy: while any contributions toward reducing poverty and poverty induced migration to find work may reduce exposure to
HIV, additional cash and the stimulus to travel further afield to market produce could result in increased exposure. Hence activities associated with promoting the marketing of agricultural products need to be carefully designed to ensure they play a role in arresting, rather than hastening, the spread of HIV in rural communities.
HIV Infection Impairs Food Security
Many studies in sub-Saharan Africa have shown the vulnerability of subsistence agriculture to the various downstream impacts of HIV. The characteristics of livelihood and farming systems will determine levels and types of vulnerability. Farming systems that exhibit a high degree of seasonality of labor demand, significant specialization by age and sex, high interdependence of labor inputs, increasing returns to scale of labor, and low substitutability of labor for capital tend to be particularly vulnerable. Studies have shown significant and enduring impacts. Labor loss occurs not only as a result of sickness and premature adult death, but also due to reallocation of labor to nurse the ill, and siphoning off of working capital to pay medical bills.
HIV has also profoundly impacted commercial agriculture, and there is increasing evidence of so-called burdenshifting as companies shift the costs being incurred, such as replacement worker costs, paid sick leave, lost wages, and productivity losses, to employees. Agriculture extension is being hit hard too, both in terms of death and sick leave of extension agents, who may be at particular risk due to their mobility, as well as declining time being allocated to extension work by current workers.
As affected households face increased labor shortages, widespread reductions in household incomes and increased cash constraints may also depress labor and nontradable demand in rural communities with high HIV incidence. Reductions in family labor may lead to a shift out of more labor-demanding cash crops. There is some evidence that multiplier effects of this depressed demand could cause reductions in labor demand to the extent that wages also fall, posing serious problems even for poor households not directly affected by HIV and AIDS. For poorer, smallholder households, land and cash may be the primary constraints on rural productivity and livelihoods, not specifically labor. AIDS is likely to progressively decapitalize highly afflicted rural communities, meaning a loss of savings, cattle assets, farming equipment, and other assets.
The impacts of HIV on agriculture and other sources of livelihood are hidden, potentially destructive processes. They are also context-specific, differing by community and by household. The nature and severity of impacts depends on a range of demographic, economic, and sociocultural factors and processes. Impacts may also be revealed in the responses made by people, and these too differ in effectiveness and sustainability. Some may be characterized as ‘coping,’ or demonstrating resilience; others are clearly taken under extreme duress and are not sustainable.
Conclusion
Undernutrition and food insecurity play a pivotal role in the global HIV/AIDS epidemic, affecting both risks of HIV transmission and the subsequent AIDS-related impacts. The response to the HIV/AIDS epidemic thus needs to be comprehensive in focusing on broad-based approaches to prevention, treatment and care, and mitigation, as well as interventions to improve nutritional status and food security globally.
Bibliography:
- Coutsoudis A, Pillay K, Kuhn L, Spooner E, and Coovadia HM (2001) Method of feeding and transmission of HIV-1 from mothers to children by 15 months of age: Prospective cohort study from Durban, South Africa. AIDS 15: 379–387.
- Fawzi WW, Msamanga GI, Spiegelman D, et al. (2004) A randomized trial of multivitamin supplements and HIV disease progression and mortality. New England Journal of Medicine 351: 23–32.
- Friis H (2006) Micronutrient interventions and HIV infection: A review of current evidence. Tropical Medicine and International Health 11: 1–9.
- Israel-Ballard K, Chantry C, Dewey K, et al. (2005) Viral, nutritional, and bacterial safety of flash-heated and Pretoria-pasteurised breast milk to prevent mother-to-child transmission of HIV in resource-poor countries. Journal of Acquired Immune Deficiency Syndromes 40: 175–181.
- Jiamton S, Pepin J, Suttent R, et al. (2003) A randomized trial of the impact of multiple micronutrient supplementation on mortality among HIV-infected individuals living in Bangkok. AIDS 17: 2461–2469.
- Paton NI, Sangreetha S, Earnest A, and Bellamy R (2006) The impact of malnutrition on survival and the CD4 count response in HIV-infected patients starting antiretroviral therapy. HIV Medicine 7: 323–330.
- Range N, Andersen AB, Magnussen P, Mugomela A, and Friis H (2005) The effect of micronutrient supplementation on treatment outcome in patients with pulmonary tuberculosis: A randomised controlled trial in Mwanza, Tanzania. Tropical Medicine and International Health 10: 826–832.
- Thior I, Lockman S, Smeaton LM, et al. (2006) Breast-feeding plus infant zidovudine prophylaxis for 6 months vs. formula feeding plus infant zidovudine for 1 month to reduce mother-to-child HIV transmission in Botswana; a randomized trial: The Mashi study. Journal of the American Medical Association 296: 794–805.
- WHO Collaborative Study Team on the Role of Breastfeeding on the Prevention of Infant Mortality (2000) Effect of breastfeeding on infant and child mortality due to infectious diseases in less developed countries: A pooled analysis. The Lancet 355: 451–455.
- World Health Organization (2003) Nutrient requirements for people living with HIV/AIDS. Report of a technical consultation. Geneva, Switzerland: WHO. http://www.who.int/nutrition/publications/ Content_nutrient_requirements.pdf (accessed December 2007).
- World Health Organization (2007) Briefing note – HIV and infant feeding. Conference on Retroviruses and Opportunistic Infections. Los Angeles, CA, USA, 25–28 February. http://www.who.int/hiv/ mediacentre/Infantfeedingbriefingnote.pdf (accessed April 2008).
- Gillespie SR (ed.) (2006) AIDS, Poverty, and Hunger: Challenges and Responses. Washington, DC: International Food Policy Research Institute.
- World Health Organization (2005) Consultation on Nutrition and HIV/AIDS in Africa. http://www.who.int/nutrition/topics/ consultation_nutrition_and_hivaids/en/index.html (accessed December 2007).
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








