This sample History of Poliomyelitis Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
The Disease
Poliomyelitis (polio) is a highly infectious disease caused by a virus. Although polio paralysis is the most visible sign of polio infection, fewer than 1% of polio infections ever result in paralysis. Poliovirus can spread widely before cases of paralysis are seen. As most people infected with poliovirus have no signs of illness, they are never aware of having been infected. After initial infection with poliovirus, the virus is shed intermittently in feces for several weeks. During that time, polio can spread rapidly through the community.
The virus enters the body through the mouth and multiplies in the intestine. Initial symptoms are fever, fatigue, headache, vomiting, stiffness in the neck, and pain in the limbs. Once established in the intestines, poliovirus can enter the bloodstream and invade the central nervous system and can cause severe paralysis in a matter of hours. As it multiplies, the virus destroys nerve cells (motor neurons) which activate muscles. These nerve cells cannot be regenerated, and the affected muscles no longer function. The muscles of the legs are affected more often than the arm muscles. The limb becomes floppy and lifeless – a condition known as acute flaccid paralysis (AFP). More extensive paralysis, involving the arms, legs and muscles of the thorax and abdomen, can result in quadriplegia. In the most severe cases (bulbar polio), poliovirus attacks the motor neurons of the brainstem – reducing breathing capacity and causing difficulty in swallowing and speaking. Without respiratory support, bulbar polio can result in death.
Poliomyelitis, once called a childhood disease, can strike at any age but affects mainly children under three, although the average age of infection has moved to higher ages in the postvaccination era. One in 200 infections leads to irreversible paralysis (usually of the legs). Among those paralyzed, 5–10% die when their breathing muscles become affected.
The First Large Epidemics
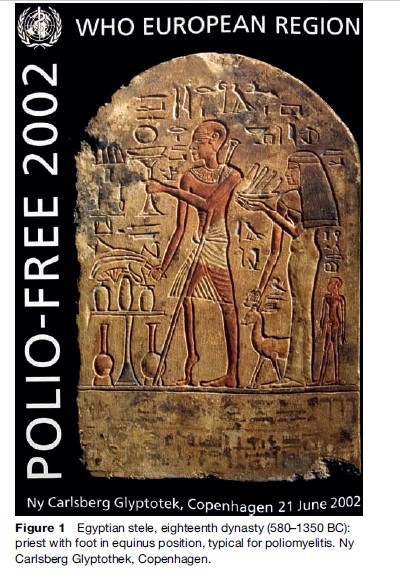
Discussion of the history of poliomyelitis is traditionally introduced with the often-reproduced illustration of the Egyptian stele from the eighteenth dynasty (580–1350BC) which is now exhibited at the Ny Carlsberg Glyptothek in Copenhagen. This stele shows a young priest with the foot in equinus position as is typical for poliomyelitis (Figure 1).
Poliomyelitis viruses probably have been prevalent as infectious agents of humans from the time that humans gathered together in villages and groups large and dense enough to facilitate the person-to-person spread of infectious agents. Paralytic disease, however, was not recognized to be a significant problem until late in the nineteenth century, when epidemics began to appear in Northern Europe. In 1840 Heine provided one of the first descriptions of the clinical disease as we now know it (Heine, 1840).
A revealing study in the 1950s showed an inverse relationship between infant mortality rates and the incidence of paralytic poliomyelitis; places with high infant mortality rates (Egypt, Algeria, and Mexico, for example) had minimal rates of poliomyelitis, while places with low infant mortality rates (Sweden, Australia, the United States, for example) had a high incidence of poliomyelitis (Payne, 1955). Widespread infections (of many kinds) in infancy resulted in high mortality but also in immunity for the survivors; the sanitary regimes of the West preserved far more infants but left them more vulnerable to poliomyelitis infections later in life.
The disease poliomyelitis – also called polio or infantile paralysis – became a reality in the lives of Europeans and North Americans in the late nineteenth century, beginning with isolated outbreaks in rural towns in Norway, Sweden, France, and the New England states.
The first city experiencing an epidemic was Stockholm, the Swedish capital, where 44 cases were reported in 1887. In 1905 Sweden reported over 1000 cases of poliomyelitis, and in 1907 New York experienced its first polio epidemic. Its epidemic appearance in the late nineteenth century, we now believe, was an unintended byproduct of improved sanitation in ‘advanced’ countries of North America and Europe, where children were raised in relatively ‘germ-free’ surroundings and thus only contracted the poliomyelitis virus after infancy, when they might have been more susceptible to serious symptoms. By the twentieth century greater numbers of older children and even young adults were involved.
The epidemic of 1905 in Scandinavia reached the staggering figure of 1031 cases. It was by far the largest one that had occurred up to that time anywhere in the world. In 1907 Ivar Wickman recognized the seasonal occurrence of the disease in Sweden in the late summer and early fall with a dramatic peak of about 370 cases in August, and emphasized the large percentage of abortive and nonparalytic cases and their relevance for the spread of infection by direct contact from person to person (Wickman, 1907). Before Wickman, the thesis of poliovirus infection by direct contact had been highly controversial.
Only 3 years later the discovery of poliovirus was announced in 1908, in Vienna, by Landsteiner and Popper (1908). With the discovery of the etiological agent came the possibility of isolating the virus for diagnostic purposes and measuring immune reactions resulting from infection, with the hope of immunization as well.
In the summer of 1916 a major epidemic of poliomyelitis occurred in the United States. Between June and October of 1916 New York suffered 8900 cases and 2400 deaths. Most of the victims in New York City were young children. The 1916 epidemic initiated a period of 40 years when American obsession with poliomyelitis made it the shock disease of the century, the one around which fear gathered and against which a new scale of private philanthropy was mobilized in the search for remedies or preventive vaccines.
This outbreak generated widespread consternation; draconian measures, triggered by assumed etiologies of poliomyelitis, were initiated to protect children. In these attempts at enforcement of isolation and quarantine measures, Italian immigrants became the first scapegoats, although no cases had been noticed among immigrants and no records of epidemics in Italy were available. A complete exodus of children of the well-to-do from the city New York was the result. Cats and dogs suspected of being carriers of the disease were brought to the police by small poor boys for a bonus, to be destroyed at a rate of 300 to 400 animals a day. All this and much more was part of a collective hysteria engendered by the epidemic.
It may be called the world’s first major poliomyelitis epidemic, and it came at a time when Western medical science had made strong, and widely accepted, claims of mastery of disease. The epidemic spread despite those efforts. Medicine’s relative powerlessness in the face of the 1916 epidemic was therefore particularly disturbing, and the reactions (medical, political, and popular) of Americans revealed important social and intellectual prejudices and tensions.
The American city governments and their public health officials reacted to the epidemic in ways that reflected their beliefs in ‘dirt’ and ‘germs’ as a cause, and the housefly as an agent of transmission.
During the years 1909–15 the maximum annual rate of reported cases in the United States had never exceeded 7.9 per 100 000 population, but in 1916, within the epidemic area, it suddenly leapt to an all-time high of 28.5. Hardly had the epidemic begun when orders were given that all premises housing a case of poliomyelitis should be placarded and the family quarantined; the windows were to be screened, the bed linen disinfected, nurses were to change their clothing immediately after tending any patient, and even household pets were not allowed in any patient’s room, as they, too, were considered suspect. Besides all these restrictions, on July 14 a new order went out, one that caused much adverse public comment. This was the decision to restrict travel, limiting movement out of the epidemic area and requiring the issuance of so-called ‘health certificates,’ which amounted to travelers’ identification cards. All children under 16 years of age were placed in the restricted category and were not permitted to leave New York City from July 18 until October 3, 1916, unless a certificate was produced indicating that the premises they occupied were free from poliomyelitis.
Perhaps most important to the public was the general ineffectiveness of the therapies offered for poliomyelitis. What actually was learned from this most extensive epidemic? For one thing the various quarantine restrictions enforced at the time were proved to be ineffective and subsequently shown to be not worth enforcing. The idea that domestic animals had anything to do directly with the spread of poliomyelitis to man was disproved and finally laid to rest. The truth of the matter was that the infection was simply too widespread, too hidden for any such measures to be effective.
The summary of the final Public Health Service’s report was (Lavinder et al., 1918):
- That poliomyelitis is, in nature, exclusively a human infection, transmitted from person to person without the necessary intervention of a lower animal or insect host.
- That the infection is far more prevalent than is apparent from the incidence of clinically recognized cases, since a large majority of persons infected became ‘carriers’ without clinical manifestations.
- That the most important actors in disseminating the infection are the unrecognized carriers and perhaps mild abortive cases ordinarily escaping recognition.
- That an epidemic of one to three recognized cases per 1000, or even fewer, immunized the general population to such an extent that the epidemic declines spontaneously, due to the exhaustion or thinning out of infectable material.
Polio, A Major Public Health Problem In The Western World
Most Americans of the period between 1945 and 1955 regarded poliomyelitis as the epidemic of the time. The 1916 epidemic began a period of over 40 years when poliomyelitis was never far from the center of American concerns about disease. The peak of the U.S. epidemic occurred in 1952: almost 57 000 cases, more than 21 000 paralytic. Similar epidemic trends were occurring all over the Western world. Panicking people started to avoid public places, especially in the summer, when outbreaks occurred more often.
In 1921, Franklin D. Roosevelt, a former assistant secretary of the Navy and vice-president candidate for the Democratic Party, contracted polio and was left paralyzed in the legs when he was 39 years old. In 1927, Roosevelt founded the Georgia Warm Springs Foundation for the treatment of those with polio. Five years later, he was elected president. In 1938, he helped create the National Foundation for Infantile Paralysis. The foundation used Hollywood celebrities to promote fund drives. The polio crusade ‘March of Dimes’ started in 1928.With the money flowing, the National Foundation began spending – setting up programs to assist those already affected by polio and funding research to vanquish the disease.
A relatively new social phenomenon – a privately funded philanthropic pressure group – generated some of the popular pictures of the epidemic of poliomyelitis. The National Foundation for Infantile Paralysis played important roles in both the (social) awareness of the epidemic in public opinion and in the direction of the research mustered against it.
Prior to the 1930s, polio cases occurred mainly in young children, except in small isolated communities where older children, adolescents, and even adults were only sometimes affected. Beginning in the 1930s, however, an epidemiological shift was observed as polio was striking many more older children and adolescents, first in Scandinavia and the United States, and then elsewhere in Europe.
In the 1950s the phenomenon ‘provocation poliomyelitis’ was identified: poliomyelitis following muscle injury, physical exertion, or prophylactic intramuscular inoculations concomitant with poliovirus infection. Risk of provocation was much reduced by giving DPT vaccinations (diphtheria, pertussis, and tetanus) in winter when circulation of poliovirus was minimal.
Doctors were helpless in caring for severely paralyzed patients, those who suffered from difficulties in breathing, until the 1920s. Then a discovery was made that hardly could be called curative but which revolutionized the treatment of this most serious form of the disease: the so-called ‘Drinker respirator’ (Drinker, 1929) (Figure 2). This life-saving apparatus was put to immediate use for patients who were unfortunate enough to be incapacitated because of difficulties resulting from paralysis of the muscles necessary for breathing, such as the intercostals and the diaphragm. Another and much more serious kind of respiratory difficulty often is the result of what is known as the bulbar form of the disease, in which there are lesions in that part of the brain (the bulb) that is adjacent to and leads into the spinal cord. Damage in this area is apt to involve the nervous centers that govern respiration, swallowing, and coughing. Patients with problems in these functions have a particularly poor prognosis. The Drinker respirator consisted of a rigid cylinder into which a patient could be placed, and at short regular intervals negative and positive pressure could be applied within the apparatus. It was promptly dubbed the ‘iron lung,’ a name which immediately caught on with all of its gruesome implications.
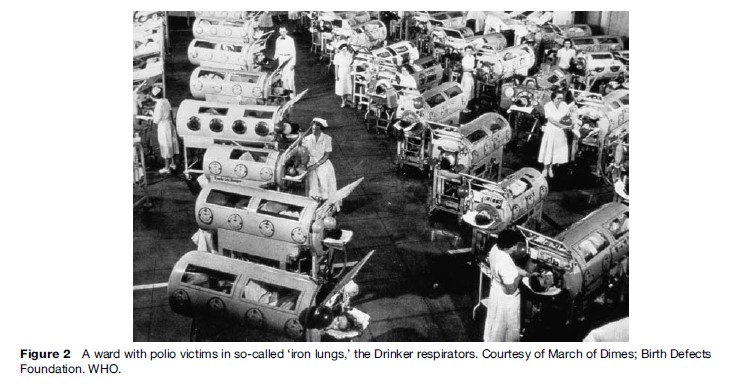
Other countries, faced with similar problems in handling patients with respiratory complications, developed similar approaches. In 1952, Copenhagen was struck by a severe epidemic of poliomyelitis that included a large number of cases of bulbar polio resulting in respiratory paralysis. During the period from August to December, about 3000 patients with polio were admitted mainly to one infectious disease hospital, the Blegdam Hospital, and of these, about 1250 had some type of paralysis. Some 345 patients had bulbar polio affecting the respiratory and swallowing muscles. For several weeks, 30 to 50 patients with bulbar symptoms were admitted daily and 6 to 12 of these were desperately ill. The epidemic resulted in enormous challenges. The hospital lacked ventilators. The stunningly innovative solution was to use manual positive pressure administered by repeated manual squeezing of a rubber bag attached to a tracheostomy tube. It was immediately apparent that support of respiration by bag ventilation required the assistance of what were described as ‘well-trained personnel all around the clock.’ The ‘well-trained personnel’ were 200 medical students per day who, following a roster, ventilated 40 to 70 patients 24 h a day for several weeks. They were risking their lives. The device served as a life-saving measure for many of the more than 1000 paralytic cases during the extensive epidemic in Denmark in 1952 (Lassen, 1956).
Vaccines Against Polio: Salk And Sabin
Today, the word ‘polio’ is linked to a vaccine to be taken, not to a disease to be feared. The history of the poliomyelitis vaccines, as we now know it, is very much the history of two eminent scientists Jonas Salk (1914–95) and Albert Sabin (1906–93), both from Russian-Jewish immigrant families in the United States and both chemists.
In 1931 Sir Macfarlane Burnet and Dame Jean MacNamara identified several types of poliovirus, known as types 1, 2, and 3 (Burnet and MacNamara, 1931). Implications of this finding were the need to include all three antigens in any effective vaccine. In 1948 Thomas Weller and Frederick Robbins (Enders, 1949) succeeded in growing poliovirus in live cells, which laid the foundation for the development of any vaccines against polio. Six years later they received the Nobel Prize for their work.
Before the introduction of vaccines, William McDowal Hammon and colleagues provided the first evidence that antibodies to poliovirus could prevent the disease in humans (Hammon et al., 1952). Passive immunization was a major breakthrough in prevention of the disease. In 1953 Jonas Salk injected an inactivated vaccine (IPV) into over 100 children, and in the following year the vaccine was given to 400 000 children in an elaborate field trial involving 1.8 million children. The effort was successful, but a slightly different vaccine was finally licensed (Francis et al., 1957).
Factors that contributed mightily to the efforts to immunize against poliomyelitis were the advances in tissue culture made possible in part by the availability of antibiotics, the separation of the poliovirus family into its three respective types, and of course the discovery by 1952 that viremia occurs with regularity in the early stages of poliovirus infection, indicating that even low levels of antibody were sufficient to protect. Salk had chosen the right moment to conduct his immunization studies, considering the technical improvements since the early 1940s and the financial support that was now available. It is not accurate to call him the discoverer of the formalinized poliovirus vaccine, however, since a similar approach had been used by Brodie in 1935 (Brodie and Park, 1935); it is more correct to say that Salk perfected its use for mass immunization in man and cleared the way for its wholesale adoption.
More than 1 800 000 children throughout the length and breadth of the land had participated in the great ‘experiment’ in 1954, and all were anxious and eager about the results. More than 200 000 children were vaccinated without serious accidents, and the protective rate had proved to be more than 50%. In the United States, from April 12 to May 7, approximately 4 million doses of poliomyelitis vaccine manufactured by five different commercial laboratories were administered to children without anything untoward happening. The decline in attack rates for naturally acquired paralytic cases had been from two to more than five times greater among vaccinated children than among unvaccinated in the same age group. But the triumphant announcement made on April 12, 1955 was followed by a serious setback: certain lots of vaccine (produced by Cutter Laboratories of Berkeley, California) had contained live poliovirus. A total of 204 vaccine-associated cases occurred. Of these, 79 were among vaccinated children, 105 among family contacts of vaccinated children, and 20 among community contacts. Approximately three-fourths of the cases were paralytic. There were 11 deaths, making a case fatality rate of 5%. During a brief period, the confidence of the nation was sadly shaken. Cutter produced the smallest amount of vaccine of any of the manufacturers, and the products of the other companies proved to be safe. One important outcome of the so-called ‘Cutter incident’ was the creation of the surveillance unit at the Centers for Disease Control (CDC). Manufacture and safety testing of the Salk vaccine were tightened but at the cost of reduced antigenicity. In the 1980s a purified and more antigenetic IPV was produced that required two doses instead of three to produce lasting immunity. Innovations by French and Dutch researchers led to markedly reduced cost of production of this highly purified and potent vaccine (Wezel, 1984). It could be combined with diphtheriapertussis-tetanus (DPT) vaccine.
Once the painful episode of the Cutter incident had subsided, the triumph of the Salk-type vaccine became even more manifest. In the United States the incidence of paralytic poliomyelitis fell from 13.9 per 100 000 in 1954 to 0.5 in 1961. Not only was the incidence reduced but also the epidemiological picture was altered so that outbreaks appeared largely in localized, urban, unvaccinated groups. The spectacular decline in incidence that had taken place first in the United States, Canada, and Denmark spread to many parts of the world by 1960. In Sweden, which was once a country with a most evil reputation regarding poliomyelitis, the disease virtually ceased to exist in 1962 as a result of the use of the inactivated vaccine. In developing countries, however, logistical problems of adequate distribution and administration have remained almost insurmountable for the use of the Salktype vaccine. Until about the early 1980s IPV continued to be made the way Salk had prescribed.
In the 1950s A. B. Sabin produced an oral polio vaccine (OPV), which has since been used extensively throughout the world (Sabin, 1955). The principle of a live attenuated virus vaccine was not new. Such vaccines had been used in the veterinary field for some time, and in man a live virus vaccine had been in effect for the prevention of smallpox for 150 years and of yellow fever for nearly 20 years. Of great importance was Sabin’s discovery by quantitative studies than the central nervous system of lower primates (rhesus and cynomolgus monkeys) was more susceptible to polioviruses than that of higher primates (chimpanzees) – and by epidemiologic analogy, man. The reverse was true for the alimentary tract, particularly in rhesus monkeys; the susceptible human intestinal tract was readily infected by doses of virus that were ineffective in monkeys. So the major task was to find or produce a strain of each type with the least neurotropism but which would multiply extensively in the human alimentary tract.
The widespread acceptance of the Salk vaccine made it very difficult for Sabin to conduct large trials of his own vaccine in the United States. He therefore chose the unusual strategy of collaborating with Soviet investigators to immunize millions of children in Eastern Europe with his live attenuated oral poliovirus vaccine. After several years, Yale University’s Dorothy Horstmann was sent with a group from the World Health Organization (WHO) to review the results of these studies, and she returned with a favorable report.
By 1958–59 a total of 20 field trials using oral vaccines (given to more than 115 million people) had been conducted in no fewer than 15 countries. In 1962 all three of the attenuated poliovirus strains were licensed and released for manufacture in the United States.
A new and rather disconcerting discovery was reported at the 1960 conference on live virus vaccines. This was the demonstration of a hitherto unrecognized contaminating virus in the tissue-culture substrate that was being used for production of live virus vaccines. The virus, named SV-40 (Simian Virus-40), induced malignant tumors when injected into hamsters. Here was a new cause for alarm. Not only did the problem exist with respect to live virus vaccines, but it was discovered that the level of formalin being used for the manufacture of Salk-type vaccine was insufficient to inactivate SV-40 virus. Once the presence of the contaminating virus was recognized, proper measures were taken to ensure its exclusion from the vaccine. From epidemiological studies it seems highly unlikely that SV-40 is carcinogenic or otherwise pathogenic for humans. However, the experience with SV-40 has clearly demonstrated one of the problems associated with the use of primary cell cultures to produce vaccines and biologics for use in humans.
Meanwhile, during the period of 1960–61, the idea of an oral vaccine for poliomyelitis was receiving remarkable and increasing support. By the end of 1960, Sabin OPV, given to more than 115 million people in Russia and Eastern Europe, had almost completely eliminated polio there. Gradually, opinion swung toward the routine use of the OPV instead of IPV, although Scandinavia and the Netherlands continued to use IPV. By August 1962 the estimated use of oral vaccine in the United States had reached more than 21 million doses for type I, 7 million for type II, and 14 million for type III. The expectation had been that this product would be spared the tragedy which had beset the Salk-type vaccine when it was first launched (the Cutter incident). But not so, for gradually evidence came to light that there had been a number of cases of poliomyelitis which had followed within 30 days of immunization with live attenuated virus. The cases were largely in adults, and the majority was associated with the type III strain. This slight risk was far greater for adults than for children. In contrast to insufficient inactivation of certain lots of polio vaccines in the time of the Cutter incident, the risk of vaccine-associated paralytic polio (VAPP) was inherent to the live attenuated vaccine.
Polio was previously thought to have been of very low incidence in developing countries. However, in the 1970s lameness surveys demonstrated that polio is widespread in many developing countries, leading to the introduction of routine immunization with OPV in almost all national immunization programs.
After 1962 the Sabin-type vaccine became the vaccine of choice in the United States. In the era of a strongly reduced risk of naturally acquired polio infection as a result of widespread effective vaccination programs, the risk of VAPP (estimated to be 2 per 1 000 000 primovaccinations) became unacceptable. After 1980, almost every case of polio in the United States (about a dozen per year) would be attributed to the Sabin vaccine. Finally in 1996 the United States reversed its stand and went back to IPV. Wild poliovirus, the cause of so much misery in the past, had been effectively eliminated.
Countries such as the Netherlands and the Scandinavian states have relied completely on IPV throughout the years in their successful fight against polio. In the pre-vaccination era, poliomyelitis was endemic in the Netherlands. Major epidemics were reported with sometimes more than 2000 cases (1956), representing an incidence of as high as 20.3 cases per 100 000 population. Routine immunization against poliomyelitis was started in 1957. In a catch-up program IPV was offered to all birth cohorts from 1945 onward. Even after licensing in the United States of the much cheaper OPV in 1960, the vaccine choice of IPV was not changed. As elsewhere, the incidence of poliomyelitis declined sharply. In the 1960s and early 1970s localized outbreaks still occurred in communities that rejected vaccination for religious reasons. In 1978 and in 1992–93 a large outbreak occurred in the same community that was highly susceptible to wild poliovirus. The mean age of the patients had risen to 18 years, as adolescents and adults had never been in contact with the virus. No cases occurred outside the socio-geographically closely knit network of the concerned religious groups who objected to vaccination; those outside this group that were susceptible appeared to be protected by herd-immunity, resulting from the years of consistently high vaccination coverage in the general population. The epidemic virus spread from the Netherlands to similar minority groups in Canada (1978 and 1992–93) and the United States (1978). These events prove that imported poliovirus still constitutes a threat wherever immunity against polio at a local and regional level is low.
Recent History: Eradication And Post-Polio Syndrome
Increased knowledge and awareness about the disease in the 1960s and 1970s had shown that polio was no longer a rich man’s disease but that millions of children all over the world were suffering from polio. Bad surveillance practices in poor and population-dense countries permitted only estimations of the number of cases. Most likely more than 300 000 cases occurred yearly.
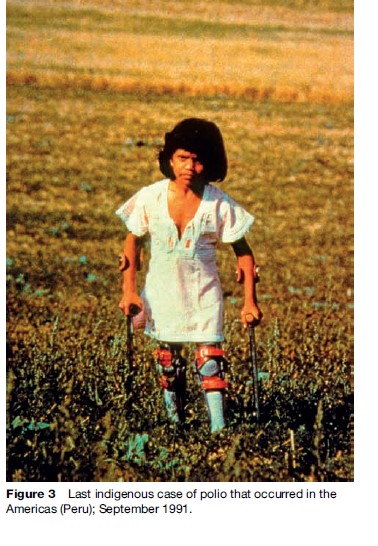
At the 1984 International Symposium on Poliomyelitis Control, it was concluded that, whereas global eradication of poliomyelitis was probably technically feasible, a realistic goal for the near future should be the control of paralytic disease, with eradication in certain countries or regions. In spite of the difficulties that were anticipated, the Pan-American Health Organization in 1985 began a major campaign to eradicate poliovirus from the Western Hemisphere. Support from the countries of the region has been remarkably strong, and various organizations have contributed resources. The last indigenous case of polio occurred in the Americas (Peru) in September 1991 (Figure 3).
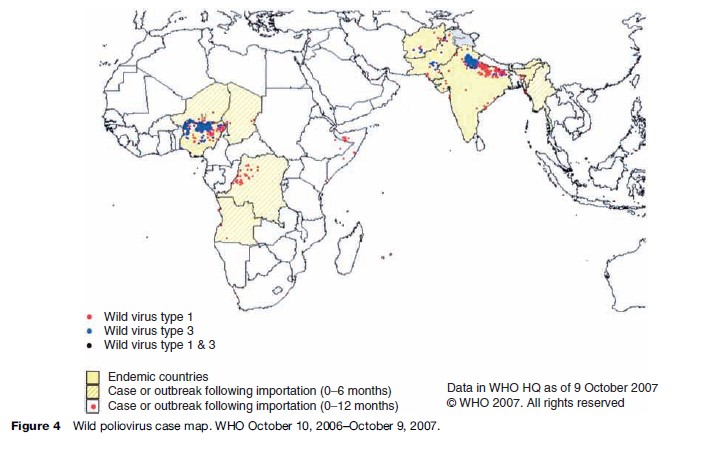
Four years later, in 1988, the World Health Assembly (WHA), the annual meeting of the ministers of health of all member states of the World Health Organization, voted to launch a global goal to eradicate polio. As a result of the Global Polio Eradication Initiative – the largest public health effort to date – at the end of 2007 indigenous polio has been eliminated from all but four countries of the world, the lowest-ever number. By then, only Nigeria, India, Pakistan, and Afghanistan were still polio-endemic. Approximately 90% of the polio cases were found in just three countries: Nigeria, India, and Pakistan. In 1988, the year the Global Polio Eradication Initiative was launched; more than 125 countries were endemic. Type 2 wild poliovirus has not been isolated since October 1999.
The global eradication policy is based on four points:
- Routine immunizations to ensure high infant coverage in the first year of life. Regions in which eradication has been achieved must continue high levels of immunization to prevent the reestablishment of poliovirus circulation after import.
- Mass immunization campaigns. During ‘mass immunization days’, routine immunization is supplemented by the provision of at least two further doses of oral vaccine to all children under 5 years old.
- Continuous surveillance of all cases of acute flaccid paralysis regardless of the underlying cause. A global network of 150 WHO-accredited laboratories aims to identify polioviruses in stool samples of all these patients, and characterizes all poliovirus isolates by antigenic and molecular methods according to standard protocols.
- Mopping up campaigns are used in countries where the final pockets of poliovirus transmission have been identified. These campaigns involve door-to-door immunization in high-risk districts where the virus is still thought to be circulating. These activities are concentrated particularly where access to health care is difficult and there is high population density and mobility, poor sanitation, and low routine immunization coverage.
The polio eradication goal has had to face many unexpected challenges. Most striking was the situation in the Northern Nigeria state of Kano, a largely Muslim area, where local politicians halted the immunization programs by claiming that the oral polio vaccine was purposely tainted to cause infertility and AIDS. Not only did new polio cases rise dramatically in Nigeria in 2004, but the disease spread to countries which had been listed as polio free (Figure 4).
Now polio-free nations are phasing out the Sabin live attenuated virus vaccine in favor of the Salk inactivated, killed virus vaccine, noting that the continued use of OPV for routine immunization could compromise the goal of eradicating all paralytic disease because of circulating polio vaccine-derived viruses. These feral vaccine viruses have caused epidemics in countries were vaccination levels had lowered to less than 50%. Prolonged infection of vaccine viruses in immuno-compromised persons can result in an accumulation of mutations in the viral genome that restores neurovirulence and the ability of these viruses to spread. The first epidemic caused by a circulating vaccine-derived poliovirus was detected in the Dominicon Republic and Haiti in 2000. Since then, other epidemics have been described at a frequency of about one per year, all in countries where vaccination coverage was lower than 50% (Kew, 2002).
The WHO global polio eradication initiative is close to success. Much has been achieved. Millions of children have been prevented from getting a severe disease. In the past, patients died and many were handicapped for the rest of their lives, which severely limited their chances in later life. In the euphoria about the success of the eradication activities, the polio survivors should not be forgotten; for many of them the polio history is not over once global eradication is achieved. Following years of surgery, rehabilitation, and exercise, polio survivors came to regard their condition as stable. They saw polio as a static disease, unlikely to return or to worsen with age. But this comforting assumption was challenged in the 1980s, as polio survivors began to experience health problems eerily reminiscent of their earlier ordeal. In the past two decades, researchers have studied this post-polio syndrome at some length. Most believe that the fatigue and muscle weakness experienced by so many polio survivors are due to wear and tear on existing nerve cells. Although no conclusive diagnostic test yet exists for post-polio syndrome, the percentage of polio survivors suffering from progressive muscle weakness and extreme fatigue is estimated to be as high as 50%. Moreover, those who endured the severest cases of polio and made the greatest functional recovery are the most likely to be affected.
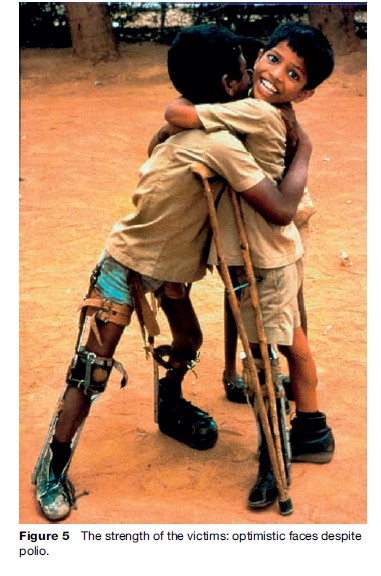
After the successful eradication of smallpox, the world can hope to start soon writing the history book on a life-threatening disease: poliomyelitis (Figure 5). Although we are not yet at that point, we have never been so close. We hope that everybody in the world takes the responsibility to finish the job.
Bibliography:
- Brodie M and Park WH (1935) Active immunization against poliomyelitis. Journal of the American Medical Association 105: 9.
- Burnet MF and MacNamara J (1931) Immunological differences between strains of poliomyelitis virus. British Journal of Experimental Pathology 12: 57–61.
- Drinker PM (1929) The use of a new apparatus for the prolonged administration of artificial respiration; a fatal case of poliomyelitis. Journal of the American Medical Association 92: 1658.
- Enders JF, Weller TH, and Robbins FC (1949) Cultivation of the Lansing strain of poliomyelitis virus in cultures of various human embryonic tissues. Science 109: 85.
- Francis T, Napier JA, and Voight RB (1957) Evaluation of the 1954 Field Trials of Poliomyelitis Vaccine: Final Report. Ann Arbor, MI: Poliomyelitis Vaccine Evaluation Center, Department of Epidemiology, School of Public Health, University of Michigan.
- Hammon WM, Coriell LI, and Stokes J (1952) Evaluation of Red Cross gamma globulin as a prophylactic agent for poliomyelitis. I. Plan of controlled field tests and results of 1951 pilot study in Utah. Journal of the American Medical Association 150: 139.
- Heine J (1840) Beobachtungen u¨ ber La¨ hmungszuta¨ nde der unteren Extremita¨ ten und deren Behandlung. Stuttyant, Germany: Ko¨ hler.
- Kew O, Morris-Glasgow V, Landaverde M, et al. (2002) Outbreak of poliomyelitis in Hispaniola associated with circulating type 1 vaccinederived poliovirus. Science 296: 356–359.
- Landsteiner K and Popper E (1908) Mikroscopische Preparate von einem menschligen und zwei Affenruckenmarken. Wiener Klinische Wochenschrift 21: 1830.
- Lassen HCA (1956) Management of Life-Threatening Poliomyelitis, Copenhagen 1952–1956; with a Survey of Autopsy-Findings in 115 Cases. Edinburgh: Livingstone.
- Lavinder CH, Freeman AW, and Frost WH (1918) Epidemiologic studies of poliomyelitis in New York City and the Northeastern United States during the year 1916. Public Health Bulletin (Washington) 91.
- Payne AM-M (1955) Poliomyelitis as a world problem. Poliomyelitis: Papers and Discussions Presented at the Third International Poliomyelitis Conference, pp. 391–400.
- Philadelphia, PA: Lippincott. Sabin AB (1955) Immunization of chimpanzees and human beings with avirulent strains of poliomyelitis virus. Annals of the New York Academy of Science 61: 1050.
- Wezel AL van, Steenis G van, Marel P van der, and Osterhaus AD (1984) Inactivated poliovirus vaccine: current production methods and new developments. Review of Infectious Diseases 6(Suppl 2): S335–S340.
- Wickman I (1907) Beitra¨ge zur Kennis der Heine-Medinschen Krankheit (Poliomyelits acuta und verwander Erkrankungen). Berlin: Kager.
- Gould T (1995) A Summer Plague: Polio and Its Survivors. New Haven, CT: Yale University Press.
- Oshinsky DM (2005) Polio: An American Story. New York: Oxford University Press.
- Paul JR (1971) A History of Poliomyelitis. New Haven, CT: Yale University Press.
- Rogers N (1992) Dirt and Disease: Polio before FDR. New Brunswick, NJ: Rutgers University Press.
- Wilson DJ (2005) Living with Polio: The Epidemic and Its Survivors. Chicago, IL: University of Chicago Press.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








