This sample Nutrition and The Elderly Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Definition
Nutrition is the process by which living organisms obtain food and use it for growth, metabolism, and repair. The elderly may be defined as those persons aged 60 years and above (WHO, 2003), and for this group the most important purpose of nutrition is not growth, but support of the metabolism and repair capacity, thus delaying aging-related processes. Functioning of every nutrition stage, such as ingestion, digestion, absorption, transport, assimilation, and excretion, is transformed with aging. That makes some nutritional requirements in the elderly different from younger adults.
History Of The Subject
Based on the average human life span (see Figure 1), the elderly’s nutritional status emerged as a problem in the twentieth century.
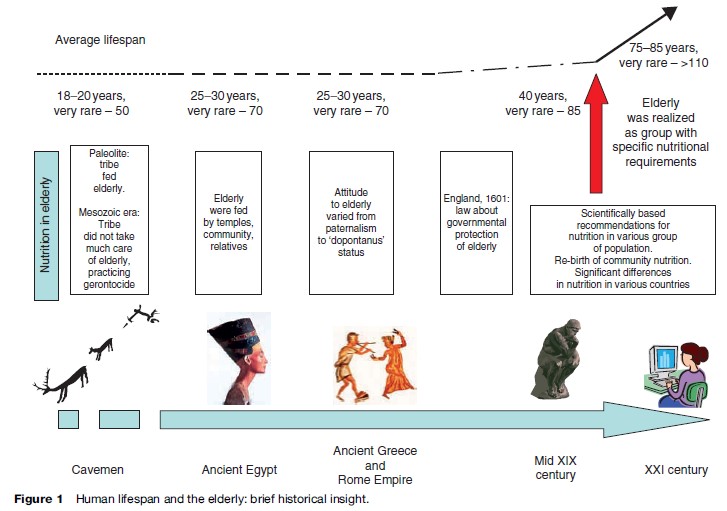
In the Paleolithic period, the existence of a large number of large herd animals made hunting effective, and a settled lifestyle resulted in a respectful attitude to old tribe members and consequently care for them. In the Mesozoic era, nomadic tribes hunted mostly small animals and they could not feed their elderly, and went as far as practicing geronticide.
The desirable Thoth-blessed life span in Ancient Egypt was 100 years: Egyptians regarded the attainment of old age as evidence of special divine favor and the reward for blameless behavior; old people were respected for their experience and wisdom and fed by temples, the community, and working family members. In Ancient Babylon, the government gave food to support elderly family members (e.g., the family was given flour instead of seeds to make it easier to cook for their elderly). Ancient Incans who reached age 60 no longer worked: Their fields were cultivated by younger members of the community just after the temples’ fields and before their own fields. In Ancient Rome, the power of the pater over the younger generations was absolute, and working family members took care of them. The elderly who had no family practiced adoption of former slaves or poor persons, who had to take care of them, including feeding. At the same time, dopontanuses existed (persons older than 60 who were used as sacrifices).
Urbanization of European society in the Middle Ages destroyed the community system and that made it difficult for old people to survive, making them completely dependent on their children. In 1601 in England, the first law was declared that government protected the elderly. In the nineteenth century, mobile kitchens were set up to feed the poor, the disabled, and old people.
In the twentieth century, quantitative dietary guidelines appeared, such as one by Cathcart and Murray in 1931, the League of Nations in 1935, and in 1944 the Proceedings of the Nutrition Society were published. It was important for elderly nutrition that the optimum of essential dietary components was recognized, replacing the term deficiency, meaning that the excess of micronutrients may be dangerous, especially in older adults. At the end of the twentieth century and the beginning of the twenty-first century, nutrition as a public health concern and community nutrition has been reborn.
How Aging Influences Nutrition
- Diseases influence absorption: Atrophic gastritis, celiac disease, lactose deficiency.
- Diseases increase metabolism: Cardiac failure, chronic obstructive pulmonary disease, Parkinson’s disease, hyperthyroidism, pheochromocytoma.
- Aging affects micronutrients:
- Decreases with aging: Vitamin A intake, 1.25-dixydroxyvitamin D, vitamin B1, erythrocyte glutathione reductase activity (associated with vitamin B2), vitamin B3 (probably), pyridoxal phosphate (associated with vitamin B6), vitamin B12, vitamin C, chromium, copper (in saliva, hair, and heart), fluoride (after age 60 in the skeleton), manganese (in kidney and heart), selenium;
- Increases with aging: Copper (in serum), iodine (in serum after age 45), nickel (in lung);
- No changes with aging: Cobalt, manganese (in serum) ( Joshi, Morley, 2006).
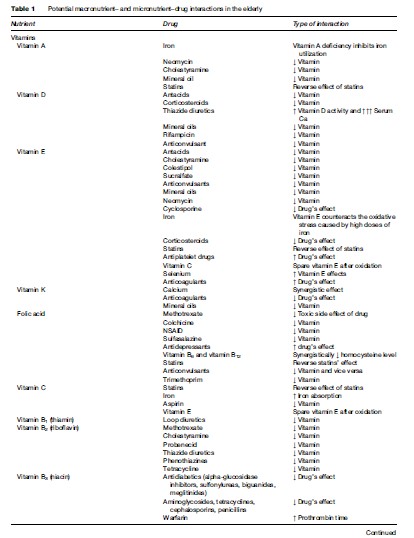
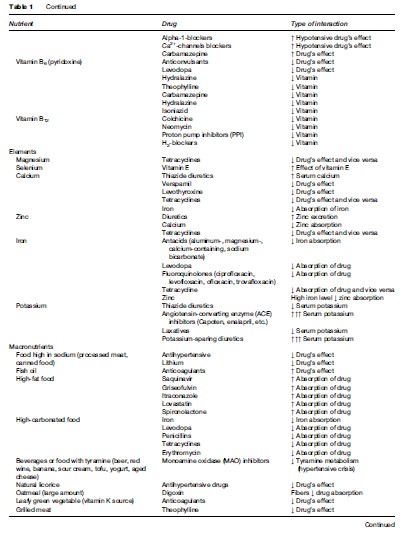
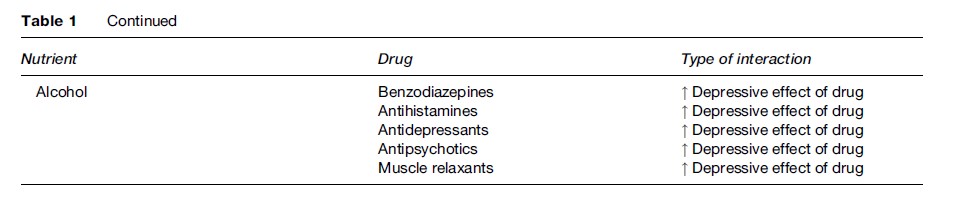
- Drug–nutrient interactions: Old people usually take one or more prescribed or over-the-counter medications (mean number of drugs prescribed for the elderly in nursing homes is 2.3–7.0 per person). It is important to take this into account when analyzing macroand micronutrient intake (see Table 1).
Old people have other problems that influence their nutrition:
- Problems swallowing (esophageal candidiasis, denture problems, tremor, stroke) and chewing (gum and dental diseases, neurological disorders).
- Changes or loss of taste and smell of food: Age-dependent changes in sense organs, adverse effect of some medications.
- Anorexia: Medication side effects (digoxin, theophylline, H2-blockers, L-thyroxine, nonsteroidal anti-inflammatory drugs, fluoxetine, lithium, phenothiazine), chronic and recurrent infections, malignancy, hyperthyroidism, hyperparathyroidism, hypoadrenalism, depression, loneliness.
- Dehydration due to both reduced fluid intake and increased fluid loss: Infection, altered level of consciousness, cognitive impairment, diuretics intake.
- Gastrointestinal problems: Meteorism, diarrhea, constipation.
- Mental and psychotic disorders: Dementia, postbereavement depression, paranoia, mania.
- Socialization: Poverty, social isolation, ignorance, problems with cooking, difficulties or inability to shop, lack of religious/ethnic food preferences in institutional settings.
How Nutrition Influences Aging
Diet is a classic risk factor of cardiovascular disease (CVD): Eight of nine risk/cardioprotective CVD factors are influenced by diet (De Caterina et al., 2006). An observed risk of atherosclerotic disease among older women was approximately 30% less in women who ate 5–10 servings of fruits and vegetables per day compared with those who ate 2–5 servings per day (WHO, 2003). A sufficient amount of vitamin C helps prevent CVD and senile cataract (Nyssonen et al., 1997).
Approximately 20% of bone mass changes can be explained by nutritional factors. Approximately one-third of the vitamin D requirements can be obtained from the diet, which is especially important for the elderly who remain indoors, because of a lack of vitamin D synthesis in their skin from sunlight exposure and the fourfold reduction in the capacity of their skin to produce vitamin D (Lips, 2001). Vitamin D, calcium, as well as a sufficient amount of protein, vitamin K, vitamin A, fluoride, phosphorus, and zinc help improve bone health in the elderly.
To support memory function in the elderly, their diet should include some solid chewable food, because diet predominantly consisting of soft ingredients suppresses the activity of the hippocampus, a brain region important to memory and learning function (Aoki et al., 2005).
Macro and Micronutrients: How Much Do The Elderly Need?
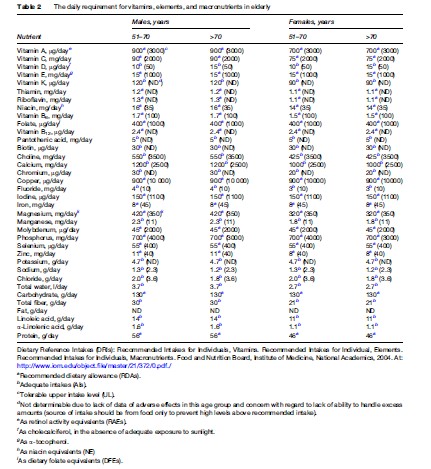
Table 2 presents the daily requirement for micro and macronutrients in the elderly.
How Nutrition In The Elderly Differs From Nutrition In Adults
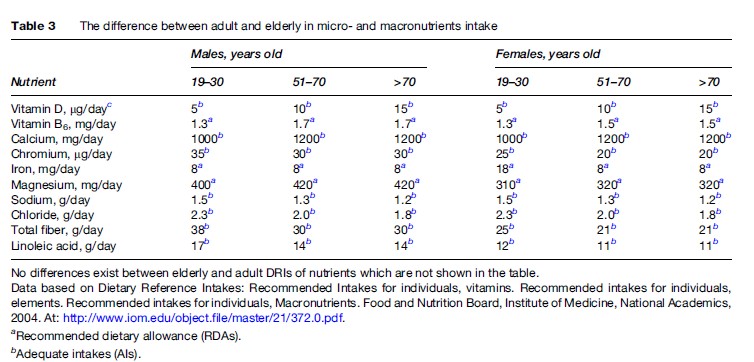
Population-based nutritional surveys show a gradual decline in energy intake in the elderly, accompanied by an increase in energy from carbohydrates and a decrease in energy from fat (van Staveren and de Groot, 2006). The decrease in protein and fat intake in the elderly is associated with mortality, while carbohydrates show a threshold effect on frail elderly patients (Frisoni et al., 1995). The association between BMI and mortality in older adults follows a J-shaped curve, unlike the U-shaped curve in younger adults. The lowest mortality occurred in 60to 90-year-olds at progressively increasing body weight, and higher mortality occurred with lower body weight (Hajjar et al., 2004). Recommended intake for some nutrients in the elderly differs from amounts recommended in adults (see Table 3).
How many calories per day a person over 50 needs depends on his or her level of activity, and it differs by gender: For women, 1600 calories for low level of physical activity, 18000 calories for moderate activity, and 2000–22000 calories for an active lifestyle; for men, 2000 calories, 2200–2400 calories, and 2400–2800 calories, respectively (National Institutes of Health, 2005).
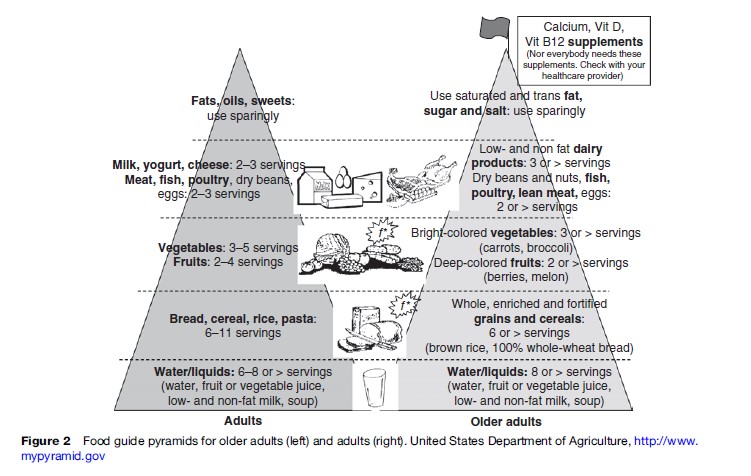
Since 1992, Food Pyramids for different groups of the population and for different cultures and countries have been created, including a specialized pyramid for older adults. Several points are stressed in the Food Pyramid for the elderly (see Figure 2). For the elderly, special considerations are calcium, vitamin D, vitamin B12, salt control (especially for persons with hypertension), lactose-free dairy products (or lactose added to milk in case of enzyme deficiency), lean meat and skinless poultry, high-fiber food (helps to promote stool regularity, of great importance for the elderly), and a sufficient amount of fluids to prevent dehydration.
Assessment Of Nutritional Status
Malnutrition is a common but a frequently underdiagnosed condition among the elderly. Consequently, in European countries and in the U.S. nearly 25–60% of hospitalized old people and 10–85% of nursing home residents have malnutrition of varying severity. Profound malnutrition and serious illness often present concurrently, accelerating each other. Malnutrition has been used to refer to a wide range of deficiencies, including protein energy, vitamins, fiber, water, as well as their excesses (obesity, hypervitaminosis). Detection of malnutrition is based on the patient’s history, physical examination, and laboratory evaluation.
Clinical manifestation: Delayed wound healing, development of pressure ulcers, susceptibility to focal and systemic infections, cognitive decline, delayed recovery from acute illness.
- History: Patient’s food diary (simple questionnaire) includes information about risk factors for deficient nutrition intake.
- Physical exam: General body habitus, body weight and height, presence of any sign of nutritional deficiency in the skin, hair, nails, eyes, mouth, and muscles. Involuntary weight loss of 5% or more in 1 month or 10% or more in 6 months is a sign of malnutrition in old age (Dempsey et al., 1998). The desired BMI for older people is 24–29 kg/m2 (compared with 20–24 kg/m2 in younger persons), and BMI under 24 kg/m2 is an indicator of malnutrition. However, BMI may not be as informative in the elderly as at younger ages because an older person’s stature often cannot be measured accurately be- cause of increased prevalence of spinal curvature; for these individuals estimation of stature from knee height is better for providing accurate information. Calf circumference is a more sensitive measure of the loss of muscle mass in the elderly compared with other circumferences and skin-fold thickness (Hajjar et al., 2004).
- Laboratory evaluation: Serum albumin levels under 3.5 g/dl are suggestive of protein energy malnutrition, albumin level under 3.2 g/dl is a predictor of mortality and morbidity in the elderly. Total lymphocyte count (TLC) less than 800 cells/mm indicates severe malnutrition.
However, no single physical or laboratory finding is a sufficient determinant of malnutrition. This is why several tools have been developed to evaluate malnutrition:
- The Instant Nutritional Assessment (INA, includes TLC, albumin, and weight change);
- The Subjective Global Assessment (SGA, combines information from the patient’s history, physical examination, and the clinician’s judgment);
- The DETERMINE checklist (developed as a screening and public awareness tool);
- The malnutrition risk scale (SCALES, was developed as an outpatient screening tool; it includes sadness, cholesterol, albumin, weight loss, eating problems, and shopping);
- The Mini-Nutritional Assessment (MNA, a screening tool of choice for many geriatricians, it includes anthropometric, general, dietary, and self-assessment parameters and does not require laboratory tests);
- The Department of Veterans Affairs defines malnutrition as meeting two of the following four criteria (weight–height ratio <90% of normal, mid-arm muscle circumference <90% of normal, albumin <3.5 g/ dl, transferring <200 mg/dl) (for detailed information about these tools, see Committee on Nutrition Services, 2000; Hajjar et al., 2004).
Dietary Supplements For The Elderly
Vitamin and mineral deficiencies often occur in elderly persons and are exacerbated during hospitalization, hypermetabolic states, alcohol use, liver disease, diuretic use, and laxative abuse, and deficiencies in this group should be corrected by food and dietary supplements. Randomized control trials do not support use of vitamin and mineral supplements by well-nourished individuals ( Joshi and Morley, 2006). Consequently, at present there is no significant proof that large doses of antioxidants can prevent chronic diseases associated with aging (such as CVD, diabetes mellitus, and cataracts). Results of nine placebo-controlled double-blind studies of multiple nutrients in the elderly, as well as 12 placebo-controlled studies with a single nutrient intervention, showed a trend of improvement in the nutritional status of the elderly, i.e., serum vitamin levels and some biochemical parameters (van Staveren and de Groot, 2006). It is acceptable for old persons to supplement with vitamin B12, calcium, vitamin D, iron (extra for postmenopausal women who are using hormone replacement therapy) and vitamin B6.
However, the doses of micronutrients should not exceed the recommended daily intakes, because adverse events associated with dietary supplements have been reported, with symptom severity increasing with age (Palmer et al., 2003).
Problem Of Food Safety In The Elderly
Old people may have problems identifying tastes and smells, and this makes food freshness control more difficult. To avoid this problem, old people should fully cook eggs, pork, fish, shellfish, and poultry and should avoid deli meats and nonpasteurized food, including dairy products.
How The Elderly Can Reduce Some Aging- Associated Problems With Nutrition
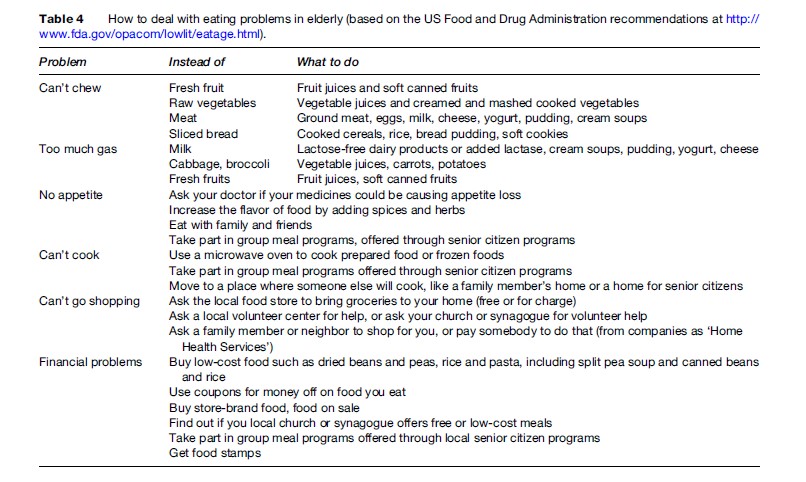
See Table 4 on how to avoid eating problems in the elderly.
Perspective Of Nutrition In The Elderly
The effect of caloric restriction on delaying aging process and prolonging the lifespan, proven in rodents, has not yet been fully explored in humans (Bengmark, 2006), so other approaches may be effective. Nutrition is a promising approach to modulating the risk of aging-related diseases by the effects of certain nutrients on gene expression. One of the most practical applications of nutritional modulation of chronic disease associated with aging may be nutrients that regulate the expression of inflammatory genes (Kornman, 2006). The anti-inflammatory molecules such as polyphenols may be effective in delaying of aging-related disease (Bengmark, 2006).
Recent studies show a positive effect of dietary sources that stimulate bone morphogenetic protein (BMP) promoter, which stimulates bone formation and thus improves bone mass in the elderly with osteoporosis. Flavonoids and statins occur naturally in food products and can promote bone formation. It may be possible to influence peak bone mass by dietary means and thus decrease the risk of osteoporosis in later life (Mundy, 2006).
New therapeutic and supplementation standards for the elderly to maintain their cognitive function and to reduce the cost of dementia can be obtained from the Nutrition, Aging, and Memory in Elders (NAME) Study of micronutrients and cognitive function in elderly (Scott et al., 2006).
Nutrigenomics is associated with the issue of personalized nutrition, since claims are being made that differences in genotype should result in differences in the diet and health relationship (e.g., folate metabolism, when a common polymorphism exists for the gene that encodes methylenetetrahydrofolate reductase). Many, possibly thousands, of other gene polymorphisms might result in minor deviations in nutritional biochemistry, where only marginal or additive effects would result from these deviations.
Summary
In summary, nutritional requirements in macro and micronutrients in the elderly differ from adults because of aging-associated effects on nutrient ingestion, digestion, absorption, and metabolism. Aging-related diseases, the effects of aging on nutrients, drug–nutrient interactions, and social problems should be taken into account when analyzing the nutritional status of the older person. Future studies will help to understand how to manipulate nutrition to alter the aging process in humans.
Bibliography:
- Aoki HM, Kimoto K, Hori N, et al. (2005) Cell proliferation in the dentate gyrus of rat hippocampus is inhibited by soft diet feeding. Gerontology 51(6): 369–374.
- Bengmark S (2006) Impact of nutrition on aging and disease. Current Opinion in Clinical Nutrition and Metabolic Care 9(1): 2–7.
- Committee on Nutrition Services for Medicare Beneficiaries (2000) The Role of Nutrition in Maintaining Health in the Nations elderly. Evaluating Coverage of Nutrition Services for the Medicate Population. Washington D.C, Food and Nutrition Board, Institute of Medicine, National Acodemy Press. http://www.nap.edu/books/0309068460/html/index.html.
- De Caterina R, Zampolli A, Del Turco S, et al. (2006) Nutritional mechanisms that influence cardiovascular disease. American Journal of Clinical Nutrition 83(2): 421S–426S.
- Dempsey DT, Mullen JL, and Buzby GP (1998) The link between nutritional status and clinical outcome: Can nutritional intervention modify it? The American Journal of Clinical Nutrition 47(supplement 2): 352–356.
- Frisoni GB, Franzoni S, Rozzini, et al. (1995) Food intake and mortality in the frail elderly. Journal of Gerontology 40: 203–210.
- Hajjar RR, Kamel HK, and Denson K (2004) Malnutrition in aging. The Internet Journal of Geriatrics and Gerontology 1(1).
- Joshi S and Morley JE (2006) Vitamins and minerals in the elderly. In: Pathy MSJ, Sinclair AJ, and Morley JE (eds.) Principles and Practice of Geriatric Medicine, 4th edn., pp. 329–346London: John Wiley & Sons.
- Kornman KS (2006) Interleukin-1 genetics, inflammatory mechanisms, and nutrigenetic opportunities to modulate diseases of aging. American Journal of Clinical Nutrition 83(2): 475S–483S.
- Lips P (2001) Vitamin D deficiency and secondary hyperparathyroidism in the elderly: Consequences for bone loss and fracture and therapeutic implications. Endocrine Reviews 22: 477–501.
- Mundy GR (2006) Nutritional modulators of bone remodeling during aging. American Journal of Clinical Nutrition 83(2): 427S–430S.
- National Institutes of Health National Institute on Aging (2005) AgePage. Good Nutrition: It’s a Way of Life. AgePage. http://www. niapublications.org/agepages/nutrition.asp (accessed September 2007).
- Nyssonen K, Parviaiinen MT, Salonen R, et al. (1997) Vitamin C deficiency and risk of myocardial infarction: Prospective population study of men from eastern Finland. British Medical Journal 314: 634–638.
- Palmer ME, Haller C, McKinncy PE, et al. (2003) Adverse events associated with dietary supplements; an observational study. Lancet 361: 101–106.
- Scott TM, Peter I, Tucke KL, et al. (2006) The Nutrition Aging, and Memory in Elders (NAME) study: Design and methods for a study of micronutrients and cognitive function in a homebound elderly population. International Journal of Geriatric Psychiatry 21(6): 519–528.
- Van Staveren WA and de Groot LCPGM (2006) Epidemiology of nutrition and aging. In: Pathy MSJ, Sinclair AJ, and Morley JE (eds.) Principles and Practice of Geriatric Medicine, 4th edn., pp. 279–290. London: John Wiley & Sons.
- WHO (2003) Diet, Nutrition and the Prevention of Chronic Diseases. Report of a Joint WHO/FAO Expert Consultation. Geneva, Switzerland: World Health Organization.
- http://www.niapublications.org/agepages/nutrition.asp – AgePage, National Institutes of Health. Good nutrition: it’s a way of life.
- http://www.nap.edu/books/0309068460/html/index.html – Committee on Nutrition Services for Medicare Beneficiaries (2000). The role of nutrition in maintaining health in the nation’s elderly. Evaluating coverage of nutrition services for the Medicare population. Food and Nutrition Board, Institute of Medicine, National Academy Press, Washington, DC.
- http://www.iom.edu – Dietary Reference Intakes: Recommended intakes of vitamins, elements and macronutrients (2004). Food and Nutrition Board, Institute of Medicine, National Academies.
- http://www.fiu.edu – National policy and resource Center on Nutrition and Aging (2004). Dietary Reference Intakes for Older Adults. Florida International University.
- http://www.nalusda.gov/fnic/pubs/bibs/gen/nutritionelderly.html –Nutrition and the elderly: a resource guide for community educators. Food and Nutrition Information Center, National Agriculture Library/ USDA.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








