This sample Obesity Prevention and Weight Management Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Introduction
Prevention of overweight and obesity is a critical public health challenge facing the world in the twenty-first century. Although the increase in overweight and obesity has been especially extreme in the United States over the past 30 years, similar increases have occurred in most wealthy countries and in urban populations of many developing countries. Trends of this magnitude and rapidity cannot be accounted for by changes in inherited genes or a worldwide decline in self-control. Rather, changes in the external (physical, economic, and social) environment, not changes in human nature, have transformed obesity and overweight into an international public health problem.
The real factors that underlie this epidemic have been changes in the availability, quantity, composition, price, and marketing of food, and decreases in the amount of physical activity needed for daily living. Humans did not evolve to live in a pastry shop. Our behavioral impulses are conditioned for times of food scarcity, not overabundance.
Being overweight/obese is linked to a myriad of diseases, chief among them hypertension, cardiovascular disease, certain types of cancers, type 2 diabetes, and gallbladder disease. Unfortunately, overweight/obesity is not very amenable to treatment; therefore, prevention is key, especially primary prevention that keeps people from ever becoming overweight to begin with.
Measuring Adiposity Using Body Mass Index
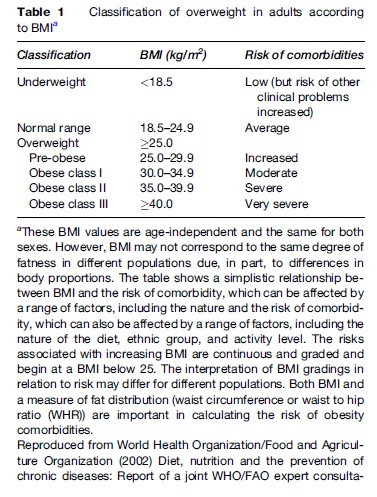
Body mass index (BMI), a measure of excess weight for height, has increasingly become the standard for measuring adiposity. BMI is calculated as weight in kilograms divided by height in meters squared. Individuals with a BMI of 25 or greater are considered overweight and those with a BMI of at least 30 are considered obese (Table 1). BMI is often used over other measures of adiposity because it is easy to calculate and removes the effect of height on weight. BMI effectively captures adiposity in the general population, although it works less well in certain groups (such as professional athletes and the elderly) who have either a very high or very low degree of muscle mass for their size.
Trends In Overweight/Obesity
In the United States, as in most other countries, the prevalence of adult overweight/obesity has risen steadily in recent decades, chiefly due to marked increases in obesity. Based on the National Health and Nutrition Examination Survey (NHANES) data, the age-adjusted prevalence of overweight among adults ages 20–74 years increased from 47.4% in 1976–80 to 66.0% in 2001–04. During the same period, the equivalent obesity rate rose from 15.1% to 32.1%. Women are more likely to be obese than men and rates of obesity are especially high among African-American and Mexican-American women. The prevalence of overweight has also been increasing among children and adolescents in the United States (National Center for Health Statistics, 2006).
The prevalence of overweight/obesity has been increasing around the world, in developing as well as developed countries. In developing countries, obesity often occurs alongside undernutrition. While there are significant variations in the rates of overweight and obesity between countries, even those within the same region, obesity rates are expected to continue to increase in most countries around the world.
Causes Of Overweight/Obesity
Genetic Makeup
Genetic makeup determines susceptibility to overweight/ obesity. Family studies by the National Institutes of Health (NIH) and the National Heart, Lung, and Blood Institute (NHLBI) have found that genetics may account for 25–40% of the difference in body mass, although twin studies suggest that the genetic contribution may be as high as 70% (NIH/ NHLBI, 1998). Many genes are likely to interact in complex ways in determining a person’s weight.
Heritable genes contribute to variations in adiposity observed within populations, but cannot account for large temporal variations that occur over a short time period. The proportionate contribution of inherited genes, as opposed to environmental factors, depends on the amount of variation in food availability and physical activity level.
Environmental Factors
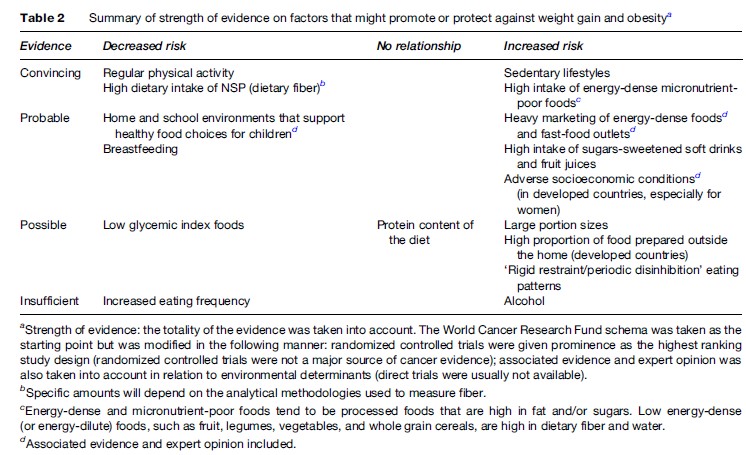
The environment also plays a critical role in this process by influencing which susceptible individuals will go on to become overweight and obese. The importance of environmental factors in the development of overweight/obesity can be seen by the rapid rise in obesity throughout the world in the last few decades. In addition, it is well known that population groups who migrate from less developed to more developed countries tend to change their lifestyle habits, as well as become more prone to obesity and other chronic diseases, within a couple of generations. Environmental factors will explain most of the difference in body weight between two populations that differ widely on food availability (e.g., famine conditions vs. American fast-food customers), but a much smaller proportion if the external environments are similar. Lifestyle factors, including diet and physical activity, are important, modifiable causes of overweight/obesity (Table 2). A recent World Health Organization (WHO) and Food and Agricultural Organization (FAO) joint technical report concluded that there was convincing evidence that a diet rich in energy-dense, nutrient-poor foods was a cause of obesity (WHO/FAO, 2002). These foods contribute to excessive caloric intake, which in turn leads to weight gain.
A sedentary lifestyle has also been implicated as a cause of obesity (WHO/FAO, 2002). Less physically active individuals are more likely to gain weight over time. Many factors contribute to a sedentary lifestyle. It is increasingly common for people to have desk jobs that require minimal physical activity. People often drive to work, rather than walk or bicycle. Watching television and playing on the computer are prevalent leisure-time activities.
The role of the larger social environment in promoting obesity cannot be ignored. Individuals do not exist in a vacuum. Choices are shaped by social, cultural, and economic forces. Urbanization, globalization, and technological advancement are major trends that have spread around the world, leading to radical changes in the food supply, work, leisure-time activities, and transport. It has become cheap and easy to produce an abundance of highly processed foods that can be quickly distributed. These foods tend to be high in energy density and low in nutrient density. Their consumption is reinforced by often intensive media campaigns by food companies and fast-food restaurants. Daily life has become increasingly mechanized. Work often involves sitting at a computer all day. Watching television, playing video games, and surfing the Internet are popular leisure-time activities. Cars make it easy for people to commute to work and school, even over long distances, with minimal energy expenditure.
There is increasing evidence that the media plays an important role in promoting obesity. It has been hypothesized that the positive association between television watching and obesity in children is at least partly mediated through advertising of high-energy, nutrientpoor foods that targets children (WHO/FAO, 2002). A recent study (Wiecha et al., 2006) of over 500 school-aged children supports this hypothesis. The study found that each additional hour of television viewing per day increased energy intake by 167 calories per day. Unhealthy snack foods that are commonly advertised on television, such as candy, fast foods, sugar-sweetened beverages, and other sweet and salty snacks, were shown to mediate the association between television viewing and energy intake.
Prevention Of Overweight/Obesity
There are several different types of prevention that are applicable to overweight/obesity. Primary prevention involves either maintaining a healthy weight or reaching and then maintaining a healthy weight. The first is preferable, because it is much easier to do. Prevention also includes blocking further weight gain in people who are overweight or obese (NIH/NHBLI, 1998). Primary prevention is especially important given that weight regain occurs in a majority of people who lose weight (U.S. Department of Health and Human Services [USDHHS], 2000).
Individual-Level Interventions
Prevention efforts should start early in life and span the life course. Overweight children are at an increased risk of being overweight in adolescence and adulthood (WHO/ FAO, 2002). Furthermore, many lifestyle habits that affect obesity risk, such as diet, physical activity, and television viewing, are set early in life. Prevention in adulthood and later in life becomes increasingly important as life expectancy increases.
Guidelines For Diet And Exercise
At the simplest level, energy balance is the key to the prevention of overweight/obesity. Energy intake should not exceed energy expenditure. Eating a healthy diet and getting adequate physical activity help keep weight in check.
The Dietary Guidelines for Americans (USDHHS and U.S. Department of Agriculture [USDA], 2005) recommend eating a balanced diet that provides sufficient levels of necessary nutrients and does not exceed energy needs. People are encouraged to choose nutrient-dense foods that have a high vitamin and mineral content relative to their number of calories. Nutrient-dense foods include whole grains, fruits, and vegetables. Consumption of foods with a low nutrient density should be restricted. These foods, which include saturated and trans fats, added sugars, and alcohol, provide few vitamins and minerals for their level of calories.
Keeping portion sizes in check is an issue in today’s supersize culture. The Dietary Guidelines for Americans (USDHHS/USDA, 2005) recommend that people pay attention to how their portion sizes stack up against serving sizes given that overly large portions can contribute to the consumption of excess calories.
There is general agreement that for weight management it is the total number of calories that count, not their distribution. The NHLBI guidelines (NIH/NHLBI, 1998) make the point that lowering the amount of fat in the diet can help to reduce overall calories; however, reducing fat without reducing total calories, for example, by substituting carbohydrates for fat, is not effective for weight management.
Willett (2002) reviews the evidence on the relationship between dietary fat and obesity. Lower fat diets were associated with modest weight loss in the short term. However, in the longer term (1 year or more), differences in percentage of calories from fat in the 18–40% range did not significantly affect weight. It was also noted that the explosion in the obesity epidemic in the United States and other industrialized countries over the last few decades has occurred as the percentage of calories from fat in the diet has fallen.
Recent results from the Women’s Health Initiative Dietary Modification Trial (Howard et al., 2006), a large randomized controlled trial of 48 835 postmenopausal women lasting over 7 years, are consistent with dietary fat having little impact on overweight/obesity. Women randomized to the intervention group went to counseling sessions in which they were encouraged to maintain their total calorie intake but to reduce the percentage of calories from fat to 20%, mainly through isocaloric substitution of fat with carbohydrates. Women randomized to the control group were given written diet and health information. The difference in the change in body weight between the two groups was 1.9 kg after 1 year but only 0.4 kg after 7.5 years.
Being able to follow a healthy diet over the long term is important to weight management. The NHLBI guidelines (NIH/NHLBI, 1998) recommend taking into account food preferences. A recent randomized trial (McManus et al., 2001) found that a balanced, moderate-fat diet that allows a variety of foods to be eaten may be easier to adhere to over the long run, and thus more effective for weight management, than a more restrictive, low-fat diet. Individuals were randomized to either a moderate-fat, Mediterranean-style diet or a low-fat diet. Both groups had the same total energy goals but the low-fat group was instructed to have 20% of calories from fat and the moderate-fat group 35% of calories from fat. Both groups also received the same intensity counseling sessions. Adherence to the dietary program and mean weight loss were both higher in the moderate-fat group compared to the low-fat group. Interestingly, individuals in the moderate-fat group also commented on how they enjoyed many of their food options and found the diet to taste better and to be less restrictive than previous diets they had tried.
Greater amounts of physical activity can increase energy expenditure, the other component of the energy balance equation. To promote general health and wellbeing, the general consensus is that 30 min of moderate intensity physical activity on most days of the week is required. To prevent weight gain, however, it is likely that 45–60 min of moderate-intensity physical activity on most days of the week is needed. For people who are trying to keep off weight that they have lost, 60–90 min of physical activity per day is helpful (WHO/ FAO, 2002).
The NHLBI guidelines (NIH/NHLBI, 1998) review the evidence for the relationship between physical activity and overweight/obesity. Physical activity is associated with modest weight loss. Purely in terms of weight loss, diet alone may be more effective than physical activity alone. However, diet and physical activity complement each other, with the combination of diet and physical activity more effective than either intervention alone. Perhaps most importantly, physical activity may play a crucial role in weight management over time. Cross-sectional studies have found that physically active people have a lower body weight and gain less weight as they age. Longitudinal studies lasting up to 10 years have shown that physically active people do not gain as much weight over time.
There are many strategies that individuals can take to incorporate more physical activity into their lives (NIH/ NHLBI, 1998). When starting to exercise, people should slowly increase the length and intensity of their workouts. People should also work to lead less sedentary lifestyles in general. For example, instead of automatically taking the elevator, they should consider taking the stairs. Being open to trying a variety of different activities is also helpful. These can range from team sports to gardening. Finally, individuals should make a concentrated effort to schedule physical activity into their busy lives.
The Role Of Health-Care Providers
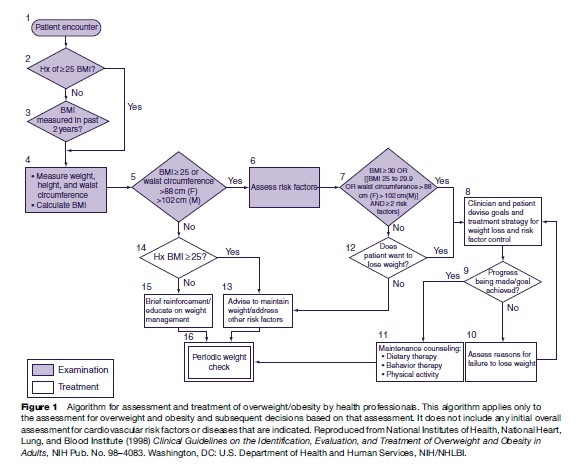
Health professionals play an important role in weight management (Figure 1). Primary care providers are in a position to assess and monitor the BMI of their patients. They can also counsel on weight loss and management, including diet, physical activity, and behavior therapy. Other specialists, such as nutritionists, exercise physiologists, and psychologists, also have a role in this process (NIH/NHLBI, 1998).
The Role Of Counseling
Behavior therapy helps people to more effectively change their diet and physical activity habits, promoting long-term weight management (NIH/NHLBI, 1998). Behavior therapy comes in many forms. People can self-monitor their progress by keeping diaries on their food intake and activities, manage stress through deep breathing and meditation, practice stimulus control by not buying junk food at the grocery store, reward themselves for accomplishing certain goals, and enlist the social support of friends and family to help them in their quest for lifestyle change.
The most effective weight management programs are those that combine diet, physical activity, and behavior therapy. A state-of-the-art diabetes prevention trial (Diabetes Prevention Program Research Group, 2002) shows that combination lifestyle therapy is highly effective in weight management and prevention of type 2 diabetes. Participants in the trial included 3234 nondiabetic, overweight adults with elevated plasma glucose levels who were followed for an average of 2.8 years. They were randomized to one of three groups: placebo (twice daily), metformin (850 mg, twice daily), or lifestyle intervention. Individuals in the placebo and metformin groups also had a counseling session and received written materials on eating a healthy diet, increasing physical activity, and losing weight. Individuals in the lifestyle intervention group had a 7% weight loss as their goal. They were coached to follow a healthy diet low in both calories and fat and to engage in moderate physical activity for at least 150 min each week. They received 16 individualized counseling sessions covering diet, physical activity, and behavior change during the first 24 weeks. Subsequent individual and group counseling sessions reinforced what they had learned in the first 24 weeks. Participants in the lifestyle intervention group reduced total calories and increased physical activity levels more than those in either the metformin group or the placebo group. In turn, they also lost more weight and had a lower risk of type 2 diabetes.
Weight Control And Smoking Cessation
Smoking cessation is a major challenge for weight control. Getting smokers to quit is clearly a top public health priority. Unfortunately, quitting smoking often leads to weight gain. About one-third of this weight gain can be attributed to a reduced metabolic rate, which in turn lowers energy expenditure. The rest can be accounted for by increases in energy intake that often accompanies smoking cessation. About 80% of people gain weight as they quit smoking. Weight gain during smoking cessation usually ranges between 4.5 and 7 pounds but can be much more substantial in a minority of cases. The prospect of weight gain can be an issue in getting people, especially women, to quit smoking (NIH/NHLBI, 1998).
Preventing weight gain following smoking cessation can be very difficult. Using drug therapy, such as nicotine replacement, delays, but does not stop, weight gain from happening. NHLBI guidelines (NIH/NHLBI, 1998) recommend using diet and physical activity to prevent weight gain when quitting smoking. Results from one large prospective cohort study highlight the importance of physical activity in mitigating weight gain following smoking cessation (Kawachi et al., 1996). Four groups of women were compared in this study over a 2-year follow-up period: women who continued to smoke throughout the study and who had little change in their physical activity habits during follow-up, women who quit smoking but did not change their physical activity habits, women who quit smoking and increased their physical activity by 8–16 metabolic units above resting (MET) hours per week, and women who quit smoking and increased their physical activity levels by 16 or more MET-hours per week. Overall, women who quit smoking gained 2.4 pounds more during the follow-up period than women who continued to smoke; however, women who became more physically active when they quit smoking tended to gain less weight.
Population-Level Interventions
To stem the burgeoning obesity epidemic and to effectively prevent obesity on a large scale, a population-based strategy is needed. Rose (1985) discusses two approaches to prevention: the high-risk strategy and the populationbased strategy. The high-risk strategy targets individuals who are most at risk of the disease, those in the tail of the population distribution. The population-based strategy, in contrast, focuses on lowering the risk of disease for averagerisk individuals, by shifting the entire population distribution downward. The population-based strategy yields greater benefits to the community; however, in what is known as the ‘prevention paradox,’ this approach that brings large support to the community offers only small benefits to each participating individual. It follows that these individuals will not easily be induced to make drastic changes in how they choose to lead their everyday lives without a radical restructuring of the social environment.
The concepts in the Rose (1985) paper are very applicable to the prevention of obesity and its associated diseases. A population-based strategy would focus on preventing weight gain in the general population, including individuals of normal weight and those who are only somewhat overweight. It can be difficult to motivate these individuals to change deeply entrenched diet and physical activity habits. It is not enough to encourage them to eat healthier and to be more physically active. To shift the distribution of obesity and its related diseases downward, it is necessary to change the social environment that shapes and reinforces the choices that individuals make.
The Richmond model for health policy (Atwood et al., 1997) provides a useful framework for addressing the challenge of obesity prevention. It is first necessary to have a knowledge base, which includes not only scientific knowledge about the issue at hand but also how the science can be translated into public health practice. The second component of the model is political will. Both people in the population at large, on the demand side, and politicians, on the supply side, must be committed to the issue and invested in developing and supporting public health programs. The final component is the social strategy. It is the application of the knowledge base and political will to a concrete framework for implementing public health policy. Social strategy should be comprehensive and include health-care providers, government and industry, and local community engagement. Healthy People 2010 (USDHHS, 2000), to be discussed further with respect to obesity, is an example of a social strategy. It tracks leading health indicators in the United States and derives specific goals to achieve to improve health.
An effective population-level obesity prevention strategy recognizes the importance of the social environment in individual choices. It requires government policy makers to work together with health-care providers, schools, the private sector, the media, and communities to make the social environment more conducive to eating healthy and being physically active.
Assessment and counseling by health-care providers must be reinforced by other changes in the physical, social, and economic environment. A WHO report (WHO/FAO, 2002) calls for governments to facilitate healthy diets by ensuring access to nutritious foods, especially in low-income areas, enacting food-pricing policies that support nutritious food choices, and requiring nutrition labels on food to foster consumer awareness. The same report urges policy makers to work with urban planners to promote the feasibility and safety of walking and bicycling in communities.
The increase in bicycling in western Germany that occurred between the 1970s and 1990s is a prime example of the impact that public policy can have in changing human behavior on a population-wide level (Pucher, 1997). During this time, communities enacted various policies that encouraged bicycling; for example, separate bike paths were constructed, some roads were restricted to automobiles, speed limits were reduced for cars, and bikes were given the right-of-way at intersections. At the same time, public policies directed at discouraging automobile use were implemented. These included increasing barriers in roadways to make driving more inconvenient, decreasing supply of parking spaces, increasing parking prices, and increasing taxes on roadway use and gasoline. The net result of these public policies was to increase the share of trips made by bicycle and decrease the share made by automobile in cities in western Germany.
Interventions in schools and workplaces have the potential to reach large groups of people where they spend much of their time. Many Healthy People 2010 goals specifically target schools and worksites (USDHHS, 2000). Goals for schools include improving nutrition, both by making more nutritious foods available and by educating school-aged children about sound nutrition practices, and increasing the prevalence of daily physical education for all students in schools. Goals for worksites include making employee-sponsored nutrition counseling and fitness programs more readily available. These can be either on-site or in partnership with other community groups.
The media also plays a powerful role in overweight/ obesity prevention, especially for children. Watching television involves little energy expenditure. Furthermore, television marketing of junk foods is extensive and there is evidence that junk food intake at least partially mediates the association between television watching and weight gain in children (Wiecha et al., 2006). Reducing television watching in children and restricting television marketing of junk food are potential interventions for overweight/obesity prevention (WHO/FAO, 2002).
Lessons From Tobacco Control
Lessons from tobacco control are relevant to the prevention of overweight/obesity, as discussed in the paper by Mercer et al. (2003). Since the mid-1960s, tobacco use has declined substantially in the United States and many other developed countries as comprehensive anti-tobacco programs have been put into place that target not only individuals but also the larger social environment. Guidelines have been established to guide physicians and other health professionals in smoking cessation counseling. Educational interventions, including anti-smoking campaigns in schools and in the media, have been effective at reducing the prevalence of tobacco use. Regulations have been enacted, including those that prohibit tobacco sales to minors and that restrict smoking in public places. Economic approaches, especially taxes, have effectively raised the prices of tobacco products, in turn lowering their consumption. Tobacco control has been so successful because of its comprehensive approach. Strategies used by health professionals, schools, communities, the media, and the government have acted synergistically.
Overweight/obesity has increased dramatically in recent decades and a comprehensive approach, like that used against tobacco, is critical to its control. It is important for health-care providers to counsel their patients about effective weight management; however, this message must be reinforced by the larger physical and social environment. Educational interventions in schools have the potential to improve nutrition and increase physical activity. The media is also a crucial component in controlling overweight/obesity, especially in children. Increased television watching in children is associated with increased weight. Currently, the media encourages children to choose junk foods through its heavy advertising of these foods. Regulations of the food industry can have a widespread impact. School lunches affect what large numbers of children eat every day and food labeling plays a role in consumer food choices. Schools can also choose to outlaw sales of soft drinks to their students. Economic policies could also influence food choices; for example, schools and worksites have increased vegetable and fruit consumption by lowering their prices through subsidies (Mercer et al., 2003).
The Situation In Developing Countries
Overweight/obesity is increasing in the developing, not just the developed world. Its spread corresponds to radical changes in diet and physical activity patterns that are in turn the result of globalization, urbanization, and mechanization. People in developing countries increasingly eat highly processed foods. Fast-food restaurants, such as McDonald’s, are endemic. Interestingly, the Republic of Korea, which has maintained its traditional high-vegetable diet, has lower rates of obesity and its concomitant chronic diseases than other similarly developed countries (WHO/ FAO, 2002). Sedentary jobs, mechanized transport, and television have also spread to developing countries. Many developing countries face a ‘double burden’ of disease, in which obesity and chronic diseases are occurring alongside undernutrition and infectious diseases (WHO/FAO, 2002), a situation that will further tax already struggling economies and health-care systems. This discussion is highly relevant for both developed and developing countries.
Conclusions
Overweight/obesity is increasing around the world, in developing as well as developed countries. Eating a healthy diet without exceeding calorie needs and getting adequate physical activity are essential to preventing overweight/obesity in individuals. Effective population-level prevention requires changes in the physical, social, and economic environment that support individual choices. Health-care providers, schools, workplaces, government policy makers, communities, and the media all play an important role in this process.
Bibliography:
- Atwood K, Colditz GA, and Kawachi I (1997) From public health science to prevention policy: Placing science in its social and political contexts. American Journal of Public Health 87: 1603–1606.
- Diabetes Prevention Research Group (2002) Reduction in the incidence of type 2 diabetes with lifestyle interventions or Metformin. The New England Journal of Medicine 346: 393–403.
- Howard BW, Manson JE, Stefanick ML, et al. (2006) Low-fat dietary pattern and weight change over 7 years: The Women’s Health Initiative Dietary Modification Trial. Journal of the American Medical Association 295: 39–49.
- Kawachi I, Troisi RJ, Rotnitzky AG, et al. (1996) Can physical activity minimize weight gain in women after smoking cessation? American Journal of Public Health 86: 999–1004.
- McManus K, Antinoro L, and Sacks F (2001) A randomized controlled trial of a moderate-fat, low-energy diet compared with a low fat, lowenergy diet for weight loss in overweight adults. International Journal of Obesity 25: 1503–1511.
- Mercer SL, Green LW, Rosenthal AC, et al. (2003) Possible lessons from the tobacco experience for obesity control. The American Journal of Clinical Nutrition 77: 1073S–1082S.
- National Center for Health Statistics (2006) Health, United States, 2006. With Chartbook on Trends in the Health of Americans. Hyattsville, MD: National Center for Health Statistics.
- National Institutes of Health, National Heart, Lung, and Blood Institute (1998) Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. NIH Pub. No. 98–4083. Washington, DC: U.S. Department of Health and Human Services, NIH/NHLBI.
- Pucher J (1997) Bicycling boom in Germany: A revival engineered by public policy. Transportation Quarterly 51: 31–46.
- Rose G (1985) Sick individuals and sick populations. International Journal of Epidemiology 14: 32–38.
- S. Department of Health and Human Services (2000) Healthy People 2010: Understanding and Improving Health. 2nd edn. Washington, DC: U.S. Government Printing Office.
- S. Department of Health and Human Services and U.S. Department of Agriculture (2005) Dietary Guidelines for Americans, 2005. 6th edn. Washington, DC: U.S. Government Printing Office.
- Wiecha JL, Peterson KE, and Ludwig DS (2006) When children eat what they watch: Impact of television viewing on dietary intake in youth. Archives of Pediatrics and Adolescent Medicine 160: 436–442.
- Willett WC (2002) Dietary fat plays a major role in obesity: No. Obesity Reviews 3: 59–68.
- World Health Organization/Food and Agriculture Organization (2002) Diet, nutrition and the prevention of chronic diseases: Report of a joint WHO/FAO expert consultation, Geneva, 28 January–1 February 2002. WHO Technical Report Series 916. Geneva, Switzerland: WHO/FAO.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








