This sample Obstructive Sleep Apnea Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Introduction
Obstructive sleep apnea syndrome (OSAS) is a common disorder that is characterized by instability of the upper airway during sleep resulting in markedly reduced (hypopnea) or absent (apnea) airflow at the nose and mouth. These episodes are usually accompanied by oxyhemoglobin desaturation, and are typically terminated by brief arousals, which result in marked sleep fragmentation and diminished amounts of slow wave and rapid-eye-movement (REM) sleep. Patients typically present with loud habitual snoring, witnessed apneas, and excessive daytime sleepiness. The prevalence among the adult population is high at about 4% in males and 2% in females. However, the condition is largely unrecognized and undiagnosed, as patients frequently see their symptoms as normal variants. Unfortunately, many patients who do seek medical attention are dismissed as having no significant illness without any formal assessment. The failure to recognize clinically significant OSAS is of particular importance because the disease is associated with significant morbidity and mortality. The excessive daytime sleepiness leads to significant impairments in quality of life, cognitive performance, and social functioning. Furthermore, the disorder is associated with a three to sevenfold increase in the rate of road traffic accidents. Moreover, OSAS is an independent risk factor for the development of cardiovascular diseases such as hypertension, coronary artery disease, congestive cardiac failure, and stroke. Nasal continuous positive airway pressure (nCPAP) is the treatment of choice in most cases and since its first description in 1981 has transformed the lives of many patients.
Pathophysiology
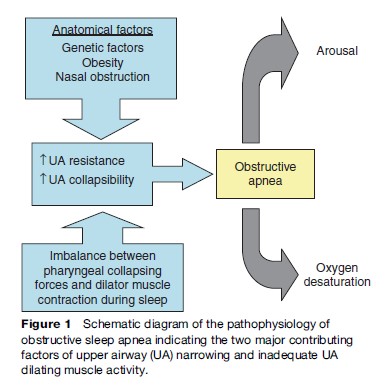
OSAS is characterized by recurring episodes of partial or complete upper airway (UA) obstruction during sleep. The underlying pathophysiology of this obstruction is complex and not yet fully understood. The UA is subjected to collapse when the negative airway pressure generated by inspiratory activity of the diaphragm and intercostal muscles exceeds the force produced by these muscles for a given cross-sectional area of the UA (Remmers et al., 1978). The patency of the UA is maintained by the product of the intrinsic anatomy and collapsibility determined by the activity of the oropharyngeal dilator and abductor muscles. A narrowed UA is more commonly seen among sleep apnea patients than controls, and studies suggest a difference in airway shape, in addition to size (Schwab et al., 1995). The observed variability in airway size is probably due to a combination of genetic influences and acquired factors such as obesity which results in UA narrowing by increased fat deposition in the pharyngeal walls and possibly also by external compression from superficially located fat masses.
UA narrowing requires an increase in pharyngeal dilator muscle contraction to maintain airway patency, and there is evidence that patients with OSAS have more forceful contraction of these muscles during wakefulness than normal subjects but show a larger decrement in contraction during sleep, thus contributing to the development of obstructive apneas (Mezzanotte et al., 1996). However, OSAS patients still show at least as forceful pharyngeal dilator muscle contraction during sleep as normals, which reinforces the fact that an imbalance between pharyngeal collapsing forces and dilator muscle contraction is responsible for obstruction rather than a primary deficiency in muscle contraction. However, the sustained increase in dilator muscle contraction in OSAS may predispose to fatigue of these muscles, which might aggravate the tendency to pharyngeal occlusion. Additional factors contributing to the pathogenesis of OSAS are instability of respiratory control leading to periodic breathing and defect of local UA neuromuscular reflexes with impairment of UA patency (Figure 1).
Predisposing Factors
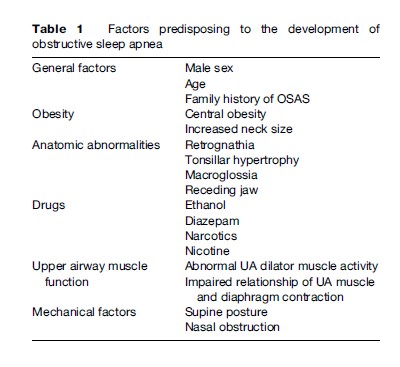
Factors predisposing to OSAS are summarized in Table 1. As outlined previously, anatomical abnormalities predisposing to a narrowed and more collapsible airway are important in the development of OSAS, with obesity as the most common factor. Furthermore, the supine position predisposes to OSAS by gravitational forces that result in posterior displacement of the tongue. Ethanol ingestion is well known to increase the frequency and duration of apneas. This effect results from the combination of a reduction in UA dilating muscle activity and a depressant effect on the reticular activating system, which impairs arousal.
Epidemiology
Many epidemiological studies over the past 15 years have demonstrated that OSAS is a common disorder. However, differences in the criteria used to define OSAS and different measurement techniques have contributed to considerable variation in reported prevalence. One of the most comprehensive studies of OSAS prevalence to date is the Wisconsin cohort study, which studied employed men and women between 30 and 60 years by means of full polysomnography (Young et al., 1993). Although 9% of women and 24% of men were found to have an apnea index (AI) greater than 5 per hour, this estimate of prevalence fell to 2% of women and 4% of men when an AI > 5 was combined with symptomatic daytime sleepiness. Higher prevalence has been found in Far Eastern and African populations, which might be explained by differences in craniofacial shape.
The male to female ratio of OSAS is about two to one. This greater prevalence in males is still poorly understood. However, gender-specific hormones may play a role, with androgens promoting upper airway collapsibility whereas progesterone in contrast seems to lead to an augmented ventilatory response. It has long been recognized that sleep apnea is very common in the elderly, but the clinical significance of this finding remains unclear. Although many of these subjects are otherwise asymptomatic for OSAS, there is evidence that sleep apnea in the elderly has an adverse prognosis. Children may develop a sleep apnea syndrome similar to that seen in adults, and several epidemiological reports suggest a relatively high prevalence, although somewhat less than in adults. The etiology of OSAS in children differs from adults in that adenotonsillar hypertrophy is the most common cause of the disorder, although the increasing prevalence of obesity among children in recent years represents an important contributing factor in many cases. Many children with OSAS can be helped by tonsillectomy.
Clinical Presentation
Symptoms
The clinical features of OSAS are summarized in Table 2. Patients typically present with a history of loud snoring, which is reported by up to 95%. However, snoring is so common in the general population that this symptom is a poor predictor of the disease. Loud intrusive snoring affects the bed partner, family, and occasionally neighbors. Noise pollution and the resulting social disharmony, which may be so severe as to jeopardize marital relationships, is an important reason that the patient, often pressurized by the partner, seeks medical help. Apneas are frequently witnessed by the bed partner and are a strong predictor of the disease. These episodes usually last only for a few seconds but can cause considerable distress both to the patient and partner. Patients themselves are frequently unaware of these episodes, so when obtaining a history it is highly desirable to also interview the partner who can usually provide important additional information based on direct observation of the patient while asleep. Many patients with OSAS report waking at night with a choking sensation, which can be quite frightening and presumably reflects an episode of outright wakening during an obstructive apnea. The choking almost invariably passes within a few seconds of wakening.
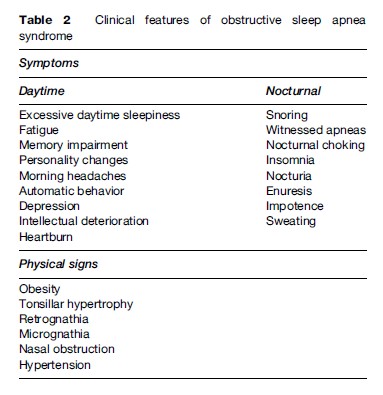
Excessive daytime sleepiness (EDS) is present in about 70% of patients and represents the most common daytime symptom. EDS is probably the result of sleep fragmentation associated with the frequent micro-arousals that typically terminate episodes of apnea. However, EDS is not a specific predictor of OSAS, since sleepiness may be a feature of many other disorders. True sleepiness needs to be distinguished from other symptoms, such as lethargy, fatigue, or exhaustion. Patients themselves may underestimate their level of sleepiness, either because they are not aware of it or because they deny it due to work-related pressures. Several tools have been developed to measure sleepiness. The most common is the Epworth Sleepiness Scale (ESS), which seeks subjective ratings of recent sleepiness. Several tests to measure sleepiness objectively have been developed but are time and labor intensive and may not reflect everyday activity. OSAS is reported to be associated with many daytime symptoms other than EDS such as fatigue, memory impairment, personality changes, automatic behavior, and depression. Although these features may be important in assessing the impact of OSAS on a patient and the effectiveness of therapy, there has been no systematic study of the capacity of these features to predict the presence or absence of OSAS.
Physical Characteristics/Examination
Obesity is an important risk factor for OSAS, and the prevalence among OSAS patients is approximately 70%. Location of fat deposition, especially anterolateral to the upper airway, is particularly important, and neck circumference is a strong predictor of OSAS (Davies and Stradling, 1990). Anatomical factors that predispose to UA narrowing should be sought in the physical examination of a patient suspected of having OSAS. These include retrognathia, micrognathia, tonsillar hypertrophy, macroglossia, and inferior displacement of the hyoid bone. However, the most common physical finding in patients with OSAS is a nonspecific narrowing of the oropharyngeal airway, with or without an increase in soft tissue deposition. Hypertension is frequently found in OSAS, and the finding of hypertension in a snoring patient significantly increases the likelihood of an associated OSAS. However, in practice, the clinical suspicion of OSAS is based on a combination of supportive features, but it is generally not possible to predict the severity of the disorder based on clinical features, except at the extremes of the clinical spectrum. Thus, some form of objective monitoring during sleep is necessary to confirm and grade the severity of the disorder.
Diagnosis
The diagnosis of OSAS depends on the presence of characteristic symptoms together with the objective demonstration of sleep-disordered breathing. A Working Group of the American Academy of Sleep Medicine laid out the clinical criteria necessary for the diagnosis of a clinically significant sleep apnea/hypopnea syndrome and also proposed a grading of severity. In the report, a diagnosis of OSAS requires that the individual must fulfill criterion 1 or 2, plus criterion 3.
- Excessive daytime sleepiness that is not better explained by other factors
- Two or more of the following that are not better explained by other factors: choking or gasping during sleep recurrent awakenings from sleep unrefreshing sleep daytime fatigue impaired concentration
- Overnight monitoring demonstrates five or more obstructed breathing events per hour during sleep. These events may include any combination of obstructive apneas, hypopneas, or respiratory-effort-related arousals.
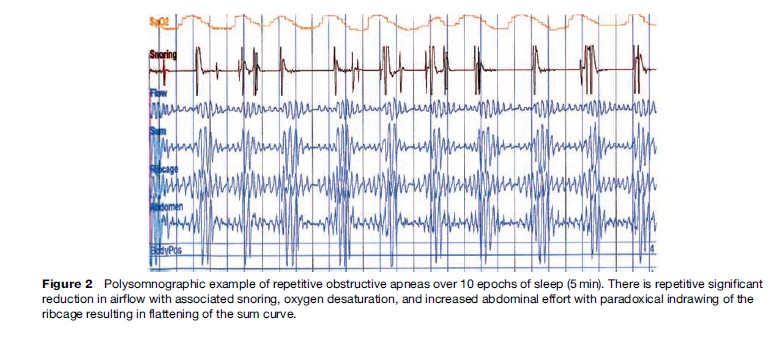
The gold standard for the overnight monitoring of a patient with suspected OSAS is full polysomnography (PSG), which provides detailed information on sleep staging, respiratory and gas exchange abnormalities, and a range of other variables including body position, heart rate and rhythm, and muscle tone and contraction. An example of an obstructive apnea is given in Figure 2. However, these studies are resource intensive, since they generally require the facilities of a full sleep laboratory and a trained technician. Thus, the prevalence figures for OSAS make it necessary to consider other simplified approaches to the diagnosis. A variety of limited diagnostic systems are available. They typically include the measurement of oronasal airflow, chest wall and abdominal effort, electrocardiography (ECG), and oxygen saturation. The potential advantages of these systems are that they are cheaper, less labor and time intensive, and technically less challenging. The main disadvantage is that the lack of sleep recording leads to uncertainty when deciding whether respiratory events, particularly periods of normal respiration, occur during wakefulness or sleep. Use of overnight oximetry in screening for OSAS is controversial. Although repetitive desaturation in the appropriate clinical context is highly specific for OSAS, the sensitivity of this tool for detection of more subtle disease ranges only from 50 to 70%. As a result, a negative oximetry recording generally needs a follow-up sleep study when OSAS is suspected on clinical grounds.
Morbidity And Mortality Related To OSAS
It has long been suggested that OSAS is associated with a significant morbidity and mortality and that it presents a major public health burden. Excessive daytime sleepiness is the most common daytime symptom of OSAS and leads to a variety of potentially serious sequelae. Patients with OSAS have significantly impaired quality of life and social functioning, as well as a higher rate of minor psychiatric illnesses such as anxiety and depression (Engleman and Douglas, 2004). Furthermore, various studies utilizing objective assessments identified significantly reduced cognitive performance in OSAS patients in comparison to controls. As a further consequence, the rate of road traffic, as well as work-related accidents, is three to seven times higher (Stoohs et al., 1995). However, the EDS and associated consequences of OSAS are reversible with effective continuous positive airway pressure (CPAP) treatment.
The principal physical morbidity and mortality of OSAS, however, relates to the cardiovascular system. The association is particularly strong with systemic hypertension, and large population-based studies have yielded convincing evidence of a modest but definite association, independent of possible confounding factors such as age, sex, or obesity. The Sleep Heart Health Study, which included over 6000 subjects undergoing in-home polysomnography (PSG), identified a modest association (odds ratio (OR) 1.37) increasing with greater severity of the disease (Nieto et al., 2000). The Wisconsin Sleep Cohort study employing 1069 subjects with in-lab PSG identified an even stronger correlation with an OR of 3.1. Moreover, a prospective follow-up of this population demonstrated that subjects with an AHI of 0–4.9, 5–14.9, and over 15 events/hour of sleep had ORs of developing systemic hypertension over the next 4-year period of 1.42, 2.03, and 2.89, respectively, compared with matched control subjects without OSAS (Young and Peppard, 2000). Data linking OSAS to other cardiovascular diseases are not as persuasive, but the evidence of an association is growing. Indeed, in the Sleep Heart Health Study cohort, OSAS emerged as an independent risk factor for congestive cardiac failure (CCF) (OR 2.2), cerebrovascular disease (OR 1.58), and coronary artery disease (CAD) (OR 1.27) (Shahar et al., 2001). Furthermore, effective CPAP therapy decreases cardiovascular morbidity and mortality, as demonstrated in large long-term cardiovascular outcome studies (Doherty et al., 2005; Marin et al., 2005).
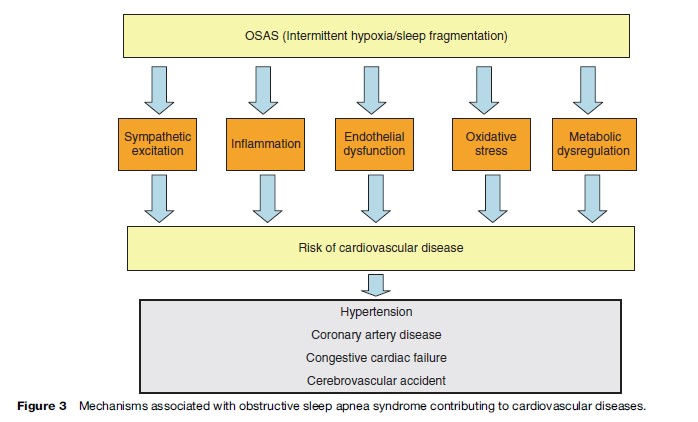
The mechanisms by which OSAS predisposes to cardiovascular disease are not fully understood but is likely to include sympathetic excitation, inflammation, and endothelial dysfunction in addition to metabolic dysregulation (Figure 3). The typical cyclical pattern of intermittent hypoxia and reoxygenation associated with OSAS probably plays a significant role in the pathophysiology as it selectively activates inflammatory over adaptive pathways with the downstream consequence of the production of proinflammatory cytokines such as tumor necrosis factor alpha (TNFa), which has been demonstrated to be involved in the pathogenesis of atherosclerosis (Ryan et al., 2005).
Management
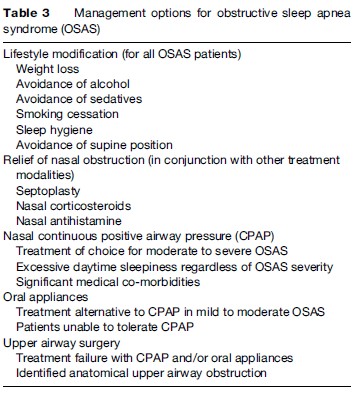
Management options for OSAS are outlined in Table 3. The most widespread and effective treatment modality is CPAP, but milder cases of OSAS can often be managed by conservative measures. These include weight loss (where appropriate), sleep hygiene, alcohol avoidance, relief of nasal congestion, and measures to keep the patient off his or her back (since most cases of sleep apnea tend to be worse when the patient is supine). Only a minority of adult cases has a correctable anatomical lesion obstructing the upper airway, but the majority of children with OSAS have enlarged tonsils and adenoids, and surgical removal of these tissues can resolve the condition in many cases.
Conservative Management
Weight Loss
As mentioned previously, approximately 70% of OSAS patients are obese, that is, exhibiting a body mass index (BMI) of more than 30 kg/m2. Weight loss has definite beneficial effects and results in improvement, or occasionally disappearance, of sleep-related breathing disorders in many patients. Weight loss is difficult to achieve but more particularly to maintain. However, in all cases, weight loss should be encouraged in obese OSAS patients. Weight loss also has beneficial effects on snoring.
Avoidance Of Alcohol And Other Respiratory Depressants
Ethanol suppresses upper airway dilator muscle activity, which predisposes to obstructive apneas and also prolongs the duration of apneas and enhances the associated oxygen desaturations. Similar effects have been reported with other respiratory depressants such as diazepam. Patients with OSAS should therefore be counseled to avoid alcohol, particularly within 3–4 h of retiring to bed, and also sedative medications.
Smoking Cessation
Smoking is a risk factor for OSAS, probably secondary to the increased upper airway resistance as a consequence of nasal mucosal inflammation. Therefore, current smokers who have been diagnosed with OSAS should be advised to quit. However, the weight gain that frequently follows smoking cessation should be actively avoided.
Sleep Hygiene
Sleep fragmentation and sleep deprivation could exacerbate OSAS, as they reduce ventilatory responses to hypoxia and increase upper airway collapsibility. However, controlled trials specifically targeting the impact of sleep hygiene on OSAS are lacking. Nonetheless, it is reasonable to advise patients of the possible interaction between poor sleep hygiene and OSAS. Avoidance of caffeine, a regular sleep–wake cycle, measures to optimize sleep environment, and avoidance of daytime napping are among the general recommendations to improve sleep hygiene.
Sleep Position
It has been long recognized that snoring patients do so most loudly in the supine position. Similarly, it has been demonstrated that a large proportion of unselected patients with a diagnosis of OSAS demonstrate a lower rate of apneic events in the lateral compared to the supine position. A tennis ball sewn into the pyjama top at the midthoracic level was one of the first means used to prevent sleep in the supine position. Two other strategies have been used, namely sleep position training using a posture alarm device and a tongue-retaining device in order to prevent tongue retrolapse when the patient sleeps in a supine position.
Relief Of Nasal Obstruction
Nasal obstruction due to anatomical abnormalities or chronic congestion is a common complaint among patients with OSAS and predisposes to UA occlusion during sleep. However, treatment modalities to relieve nasal obstruction have failed so far to demonstrate a clear benefit. In selected patients, relief of nasal obstruction by surgery, nasal steroids, or antihistamines may improve symptoms and should be considered as treatment options.
Continuous Positive Airway Pressure Therapy (CPAP)
The current management of moderate to severe OSAS is largely dependent on nasal CPAP (nCPAP), which acts to splint the upper airway open during sleep, and thus counteracts the negative suction pressure during inspiration, which promotes upper airway collapse in these patients. Nasal CPAP completely controls the condition and has a dramatic effect on the patient’s awake performance because of the normalized sleep pattern. CPAP improves quality of life, neurocognitive function, and driving performance (Jenkinson et al., 1999). Moreover, long-term cardiovascular outcome studies have demonstrated significantly fewer cardiac events in CPAP-treated patients in comparison to nontreated subjects. Although nCPAP is highly effective in controlling OSAS, the device is cumbersome, and compliance data show only moderately satisfactory results. Compliance relates positively to the severity of OSAS and level of daytime sleepiness.
Oral Appliances
Oral appliances are an alternative to CPAP therapy in patients who have failed or refused this treatment modality and also as initial therapy in patients with milder disease. The goal of therapy with oral appliances is to modify the position of UA structures in order to enlarge the airway, reduce resistance, and presumably reduce UA collapsibility. The effects on UA muscle function may also be important due to the changes in direction of muscle fibers. Although randomized studies have demonstrated benefit in improving objective and subjective sleep parameters, CPAP is significantly more effective. However, patients generally prefer oral appliances. More data are needed for neurocognitive and cardiovascular outcomes after treatment with oral appliances.
Uvulopalatopharyngoplasty
The objectives of uvulopalatopharyngoplasty (UPPP) are to enlarge the oropharyngeal airway and reduce the collapsibility of this particular segment of the UA. In OSAS patients, UPPP indications should be restricted to those with mild disease and evidence of retropalatal narrowing, and careful patient assessment and selection is very important. It should also be remembered that by increasing mouth leaks, UPPP might compromise CPAP therapy and reduce the maximal level of pressure that can be tolerated.
Conclusion
OSAS is a highly prevalent disorder that can have major adverse consequences on the health and quality of life of the affected patient. However, the disorder is eminently treatable, and successfully treated patients generally report a dramatic transformation in their quality of life.
Bibliography:
- Davies RJ and Stradling JR (1990) The relationship between neck circumference, radiographic pharyngeal anatomy, and the obstructive sleep apnoea syndrome. European Respiratory Journal 3: 509–514.
- Doherty LS, Kiely JL, Swan V, and McNicholas WT (2005) Long-term effects of nasal continuous positive airway pressure therapy on cardiovascular outcomes in sleep apnea syndrome. Chest 127: 2076–2084.
- Engleman HM and Douglas NJ (2004) Sleep, 4: Sleepiness, cognitive function, and quality of life in obstructive sleep apnoea/hypopnoea syndrome. Thorax 59: 618–622.
- Jenkinson C, Davies RJ, Mullins R, and Stradling JR (1999) Comparison of therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: A randomised prospective parallel trial. Lancet 353: 2100–2105.
- Marin JM, Carrizo SJ, Vicente E, and Agusti AG (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: An observational study. Lancet 365: 1046–1053.
- Mezzanotte WS, Tangel DJ, and White DP (1996) Influence of sleep onset on upper-airway muscle activity in apnea patients versus normal controls. American Journal of Respiratory Critical Care Medicine 153: 1880–1887.
- Nieto FJ, Young TB, Lind BK, et al. (2000) Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. Journal of the American Medical Association 283: 1829–1836.
- Remmers JE, deGroot WJ, Sauerland EK, and Anch AM (1978) Pathogenesis of upper airway occlusion during sleep. Journal of Applied Physiology 44: 931–938.
- Ryan S, Taylor CT, and McNicholas WT (2005) Selective activation of inflammatory pathways by intermittent hypoxia in obstructive sleep apnea syndrome. Circulation 112: 2660–2667.
- Schwab RJ, Gupta KB, Gefter WB, Metzger LJ, Hoffman EA, and Pack AI (1995) Upper airway and soft tissue anatomy in normal subjects and patients with sleep-disordered breathing. Significance of the lateral pharyngeal walls. American Journal of Respiratory Critical Care Medicine 152: 1673–1689.
- Shahar E, Whitney CW, Redline S, et al. (2001) Sleep-disordered breathing and cardiovascular disease: Cross-sectional results of the Sleep Heart Health Study. American Journal of Respiratory Critical Care Medicine 163: 19–25.
- Stoohs RA, Bingham LA, Itoi A, Guilleminault C, and Dement WC (1995) Sleep and sleep-disordered breathing in commercial long-haul truck drivers. Chest 107: 1275–1282.
- Young T, Palta M, Dempsey J, Skatrud J, Weber S, and Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. New England Journal of Medicine 328: 1230–1235.
- Young T and Peppard P (2000) Sleep-disordered breathing and cardiovascular disease: Epidemiologic evidence for a relationship. Sleep 23(supplement 4): S122–S126.
- American Academy of Sleep Medicine Task Force (1999) Sleep-related breathing disorders in adults: Recommendations for syndrome definition and measurement techniques in clinical research. Sleep 22(5): 667–689.
- Behn A and Ur E (2006) The obesity epidemic and its cardiovascular consequences. Current Opinions in Cardiology 21(4): 353–360.
- Krieger J, McNicholas WT, Levy P, et al. (2002) ERS Task Force, European Respiratory, Society Public health and medicolegal implications of sleep apnoea. European Respiratory Journal 20(6): 1594–1609.
- Malhotra A and White DP (2002) Obstructive sleep apnoea. Lancet 20: 360(9328): 237–245.
- McNicholas WT and Bonsigore MR (2007) Management Committee of EU COST ACTION B26 Sleep apnoea as an independent risk factor for cardiovascular disease: Current evidence, basic mechanisms and research priorities. European Respiratory Journal 2007: 29(3): 614.
- McNicholas WT and Phillipson EA (2002) Breathing Disorders in Sleep. London: Saunders.
- McNicholas WT and Ryan S (2006) Obstructive sleep apnoea syndrome: Translating science to clinical practice. Respirology 11: 136–144.
- Shamsuzzaman AS, Gersh BJ, and Somers VK (2003) Obstructive sleep apnea: Implications for cardiac and vascular disease. Journal of the American Medical Association 290(14): 1906–1914.
- Wolk R and Somers VK (2006) Obesity-related cardiovascular disease: Implications of obstructive sleep apnea. Diabetes, Obesity, and Metababolism 8(3): 250–260.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








