This sample Personality Disorders Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Personality disorders are a heterogeneous group of conditions which are characterized by relatively stable patterns of interpersonal and intrapsychic functioning that are associated with personal distress and impaired social functioning. People with personality disorder (PD) have an ‘‘enduring pattern of inner experience and behavior that deviates markedly from the expectations of the individual’s culture’’ (American Psychiatric Association, 1994: 633–634). These patterns of thinking and behaving are central to a person’s sense of self. Indeed, personality disorders can be considered disturbances of the self, of the way a person sees and experiences themselves.
Personality disorders become apparent in childhood and adolescence. In adulthood, they are characterized by long-standing emotional problems and difficulties in relationships with others. Emotional problems may include feelings of anxiety, sadness, and obsessive thoughts that are seen in people with neuroses. However, emotional states among people with PD tend to show greater short-term variation. Some people with PD experience major fluctuations in mood and feelings of emptiness, despair, and suicidal thoughts. Difficulties in relationships with others include weariness of others, a desire to avoid other people, disregard for others’ welfare, feeling dependent on others, and fears of rejection by other people.
The diagnosis of personality disorder is controversial and critics have argued that it is simply a means of labeling socially unacceptable behavior (Lewis and Appleby, 1988). Like ‘normal’ personality, personality disorders are long lasting and traditional treatments used to manage mental disorders are less effective in reducing mental distress among people with PD. Indeed some people who have been labeled as having a personality disorder complain that they are given this diagnosis as a result of their not responding to treatment for other mental disorders. This concern is supported by surveys of healthcare professionals which have shown that some use the term to refer to people they feel are untreatable. The term has also been used pejoratively to refer to people who are seen as attention-seeking, annoying, and less deserving of care (Lewis and Appleby, 1988). Such views have been challenged by research findings that have demonstrated that many personality-related problems diminish over time (Zanarini et al., 2003) and that psychological treatments can improve the mental health and social functioning of people with these problems.
Classification
Population-based studies indicate that there are aspects of personality called traits that can be reliably measured and are generally stable over time (McGlashan et al., 2005). The most enduring of these traits are extraversion/introversion (the tendency to like or to shun the company of others) and neuroticism (the tendency to worry). However, such characteristics are normally distributed in the population and there are numerous other traits that make a dimensional approach to describing personality in clinical contexts unsatisfactory. As a result, formal systems for classifying personality disorder use operationalized definitions based on clusters of traits associated with different personality types and dichotomize these as being either present or absent according to whether a cut-off point of causing significant personal distress or social problems has been reached.
Types of personality disorder used in the two main systems of classification are illustrated in Table 1. Factor analysis of personality traits in community samples suggest that these distinct categories of PD are artificial constructs and a looser system of three broad bands of PD are preferred by some. This system combines personality disorders into three clusters: cluster A (characterized by social distance and eccentricity); cluster B (characterized by flamboyance and emotional instability), and cluster C (characterized by anxiety and a tendency to worry).
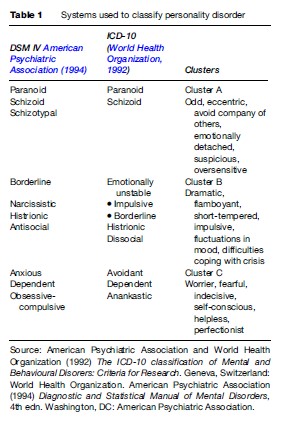
An alternative approach to the diagnosis of personality disorder has been suggested by Tyrer and Johnson (1996), based on severity of PD. Abnormal traits that do not cause enduring personal distress are labeled personality difficulty, significant problems associated with disturbance in only one cluster are referred to as simple personality disorder, those with disturbance in more than one cluster as having ‘diffuse PD’, and those with diffuse PD where there is severe disruption, both to the individual and to others, have severe PD.
It seems likely that the current system of classification will be subject to further change, but it does at least have the merit of providing diagnostic labels which relate to patterns of behavior that are familiar to clinicians and have provided a basis for research into the etiology and management of PD.
Prevalence And Outcome
Cross-sectional surveys conducted in Europe and North America indicate that between 5 and 10% of the population have a PD (Coid et al., 2006). The prevalence of PD in resource-poor nations is unknown. Within Western nations, the prevalence of personality disorder tends to be higher in inner-city areas where levels as high as 15% have been reported. Most forms of PD are more prevalent among men, especially antisocial PD, which is five times more common in men than in women. Emotional and interpersonal problems associated with PD mean that the prevalence of personality disorder is generally higher in health-care settings than in the general population. Approximately 15% of people treated by family practitioners and 40% of people treated by mental health services have a PD. Levels of PD are also higher among people in contact with criminal justice services – it is estimated that as many as 80% of people in prison have PD (Singleton et al., 1998).
There have been few long-term follow-up studies of people with PD, but available evidence suggests that psychological and behavioral manifestations of cluster B personality disorders such as impulsivity tend to become less frequent over time (Zanarini et al., 2003). In contrast, personality traits such as suspiciousness, eccentricity, and rigidity that are encountered most frequently among people with cluster A and cluster C PD seem less likely to diminish with advancing age (Seivewright et al., 2002).
Public Health Consequences Of Personality Disorder
Much of the research conducted to date has focused on the relationship between personality disorder and mental health-related problems such as depression, suicide, and substance misuse. However, people with PD also have higher rates of physical health problems and premature mortality. The standardized mortality rate for people with PD is estimated to be 184 (95% CI ¼ 140–236). People with PD have higher rates of death from infections and neoplasms as well and suicide and other forms of violent death (Harris and Barraclough, 1998). Levels of social problems such as unemployment are higher, and it is estimated that over one-fifth of homeless people have a PD.
The relationship between PD and other mental disorders is complex, not least because similar problems are experienced by people with mental and personality disorder. For instance, features of cluster A PD have much in common with the prodromal symptoms of schizophrenia and paranoid psychosis, and emotional distress experienced by people with cluster C PD has features that are also seen in those with anxiety neurosis and obsessivecompulsive disorder. Nonetheless, people with personality disorder and especially borderline PD have rates of depression and other mental disorders which are far higher than that among the general population (Zanarini et al., 1998).
Data from psychological autopsy studies indicate that as many as 40% of people who commit suicide have evidence of PD. The relationship between personality disorder and suicide is particularly strong among those with cluster B PDs such as antisocial and borderline PD among whom impulsivity and levels of affective disturbance are high. Rates of substance misuse are also high among people with PD, especially cluster B PD. This association may be attributable to the difficulties that such people have in coping with intense emotions, for which alcohol and other drugs may provide some temporary relief. However, such drugs may cause disinhibition and this in combination with personality traits such as impulsiveness further increases the risk of suicidal behavior or violence toward others.
Given that impulsivity and disregard for others are the hallmarks of antisocial personality disorder (ASPD), it is not surprising that levels of offending are increased among people with ASPD. It is estimated that, in Britain, one-quarter of violent incidents that result in injury are committed by people with ASPD (Coid et al., 2006); in contrast, hazardous drinking is implicated in over half of all such incidents. One of the traits apparent in some people with ASPD is psychopathy, which is characterized by shallow emotions, a lack of empathy or sense of guilt, and a history of lying, deceit, and criminality. This cluster of personality traits is less prevalent than ASPD, but its association with subsequent violence is far stronger. Attempts to define people who have PD and pose high risks to the public have been made, but past behavior rather than the presence or absence of certain personality traits provides a better guide to the likelihood of future violence in community settings.
Etiology Of Personality Disorder
Knowledge of factors that give rise to PD is only partial, but evidence from twin studies suggests that both constitutional and environmental factors are more important. The hereditability of personality disorder is estimated to be 0.6, with narcissistic and anankastic personality disorder having the highest hereditability (Torgersen et al., 2000). Efforts to identify genetic markers for personality disorders have not generated consistent findings, but associations between impulsivity and genes responsible for variations in serotonin receptors have been reported.
High levels of cluster A PD in relatives of people with schizophrenia have led to the suggestion that these may be part of a spectrum of disorders characterized by emotional distance from others, unusual behaviors, and odd beliefs.
More is known about the etiology of borderline PD than that of other groups. As many as two-thirds of people with borderline PD report childhood physical or sexual abuse, and other forms of childhood adversity such as parental mental illness and separation from parents are more frequent than among the general population (Bandelow et al., 2005). These strong associations have led to the view that borderline PD may be the result of deficits in a person’s sense of self resulting from disorganized parental relationships. While such risk factors appear to be important in the etiology of personality disorders, they are neither necessary nor sufficient to result in PD.
Intervention
Primary Prevention
Strong links between environmental factors and the development of PD suggest that primary prevention of PD may be possible (Coid, 2003). Such strategies could include whole-population initiatives aimed at improving the family and educational environment of all children or specific interventions aimed at families where children show early indicators of interpersonal problems such as conduct disorder. Few such programs have been evaluated, but emerging evidence suggests that if interventions are delivered early in life they may be effective. For instance, Raine and colleagues (2003) evaluated the impact of a 2-year enrichment program for 3-year-old children on the island of Mauritius. The program combined educational and nutritional interventions with a program of structured physical activity and was delivered over a 2-year period. The team were able to follow up 75 (90%) of 83 children who completed the program and 288 (81%) of 355 matched controls, demonstrating lower levels of personality-related problems and criminal behavior 20 years later. The generalizability of such findings to resource-rich settings have not been explored, but they support the notion that improving the early-childhood environment can impact on adult personality status.
Service Provision
Compared to services for people with mental illness, the development of services for people with PD has been slow. A variety of reasons have been suggested for this. It has been argued that uncertainty about the validity of diagnoses has made it difficult to develop an evidence base for services. Others have pointed to the impact that interpersonal problems associated with PD have on the relationship between therapists and patients. Personality traits such as impulsivity, excessive dependence on others and disregard for others certainly present challenges to health-care professionals working with people with PD. People with PD may also project painful emotions onto health-care workers, especially doctors and others whose position of power and authority may mirror difficult or abusive relationships people experienced at the hands of other authority figures during childhood.
Research among service users who have been given a diagnosis of PD has shown that many feel dissatisfied with the quality of care they receive. In a survey of service users with PD in Britain, a greater proportion believed that they had been harmed, rather than helped by local mental health services (Ramon, 2001).
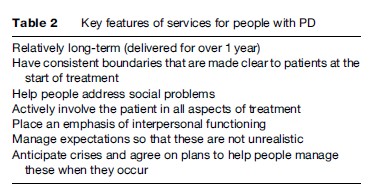
Despite these problems, specialist services for people with personality disorder have been developed. While the structure and organization of such services varies, there is a good deal of consensus about key features of services for people with PD, which are listed in Table 2.
Specific Treatments
A variety of psychosocial interventions have been developed for people with PD, but only a limited number of experimental evaluations have been conducted. Most of the randomized evaluations of interventions for people with personality disorder that have been conducted have focused on people with borderline PD. A systematic review of such studies by Binks and colleagues (2006), concluded that studies have been ‘‘too few and too small to allow any definitive statement to be made about their effectiveness.’’
Some of the earliest studies explored the effectiveness of therapeutic communities. Therapeutic communities aim to facilitate group learning and peer support and place an emphasis on self-efficacy and responsibility. Democratic therapeutic communities do this by flattening the traditional hierarchy that exists between patients and treatment staff and encouraging people to become actively involved in their treatment by involving them in the running of the community. Observational studies comparing the outcome of people with PD who are treated in residential therapeutic communities suggest they are less likely to self-harm and have lower levels of subsequent service utilization that those who are not.
Dialectical behavior therapy is a form of psychotherapy specifically developed for people with borderline PD (Linehan, 1993). It incorporates elements of cognitive therapy and skills training and places specific emphasis on helping patients identify and overcome obstacles to change. Randomized trials of dialectic behavior therapy have demonstrated improved mental health and reduced self-harming behavior among women with borderline PD, including those with comorbid substance misuse.
In recent years, modified forms of psychoanalytical and cognitive therapy have been demonstrated to improve mental health and social function of people with borderline, avoidant, and other personality disorders. In contrast, very little is known about what, if anything, can be done to reduce the likelihood of offending among people with antisocial personality disorder.
Pharmacological interventions have only a limited role in the management of PD. Exceptions to this are low-dose antipsychotic medication that may benefit people with schizotypal personality disorder, and reduce the psychoticlike symptoms that can emerge among people with borderline PD at times of crisis. Antidepressant medication may be of value in treating mood disturbance among people with PD, but response to treatment is generally less marked than among those with depression in the absence of PD. Long-term use of medication in people with cluster B and C PD is not indicated and patients may instead need help in coming off tranquilizers and antidepressants that were started at times of crisis and do not provide long-term benefit.
For patients to benefit from any intervention, they need to be sufficiently motivated to use it. Many people with PD are ambivalent about receiving interventions and a substantial proportion may not want to try to change. Under these circumstances, it has been suggested that a better approach to helping people with PD is to focus on modifying their social circumstances to create a better fit between the person’s personality and their environment. Exploratory studies examining the impact of such interventions suggest they can improve patient satisfaction and social functioning (Tyrer et al., 2003). Assessment and support with tackling social problems is an important part of the management of all people with PD.
Conclusion
In summary, personality disorders are important conditions that have negative consequences for the individual and society. While there is only partial understanding of their etiology and debate continues about the most appropriate system for their classification, poor health and social outcomes experienced by people with personality disorder highlight their public health importance. Interpersonal problems inherent in personality disorder mean that providing services for people with these conditions is not straightforward. However, clear links with childhood adversity provide a basis for the development of primary prevention strategies and an evidence base is beginning to emerge that suggests that many forms of personality disorder may be amenable to psychosocial intervention.
Bibliography:
- American Psychiatric Association (1994) Diagnostic and Statistical Manual of Mental Disorders, 4th edn. Washington, DC: American Psychiatric Association.
- Bandelow B, Krause J, Wedekind D, Broocks A, Hajak G, and Ru¨ ther E (2005) Early traumatic events, parental attitudes, family history and birth risk factors in patients with borderline personality disorder and healthy controls. Psychiatry Research 134: 169–179.
- Binks CA, Fenton M, McCarthy L, Lee T, Adams CE, and Duggan C (2006) Psychological therapies for people with borderline personality disorder. The Cochrane Database of Systematic Reviews, Issue 1.
- Coid J (2003) Epidemiology, public health and the problem of personality disorder. British Journal of Psychiatry 182(supplement 44): s3–s5.
- Coid J, Yang M, Tyrer P, Roberts A, and Ullrich S (2006) Prevalence and correlates of personality disorder in Great Britain. British Journal of Psychiatry 188: 423–431.
- Harris EC and Barraclough B (1998) Excess mortality of mental disorder. British Journal of Psychiatry 173: 11–53.
- Lewis G and Appleby L (1988) Personality disorder: The patients psychiatrists dislike. British Journal of Psychiatry 153: 44–49.
- Linehan MM (1993) Cognitive-Behavioural Treatment for Borderline Personality Disorder. New York: Guilford.
- McGlashan TH, Grilo CM, Sanislow CA, et al. (2005) Two-year prevalence and stability of individual dsm-iv criteria for schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders: Toward a hybrid model of axis II disorders. American Journal of Psychiatry 162: 883–889.
- Raine A, Mellingen K, Liu J, Venables P, and Mednick S (2003) Effects of environmental enrichment at ages 3–5 years on schizotypal personality and antisocial behavior at ages 17 and 23 years. American Journal of Psychiatry 160: 1627–1635.
- Ramon S, Castillo H, and Morant N (2001) Experiencing personality disorder: A participative research. International Journal of Social Psychiatry 47: 1–15.
- Seivewright H, Tyrer P, and Johnson T (2002) Change in personality status in neurotic disorders. The Lancet 359: 2253–2254.
- Singleton N, Meltzer H, and Gatward R (1998) Psychiatric Morbidity Among Prisoners in England and Wales. London: Stationary Office.
- Torgersen S, Lygren S, ien PA, et al. (2000) A twin study of personality disorders. Comprehensive Psychiatry 41: 416–425.
- Tyrer P and Johnston T (1996) Establishing the severity of personality disorder. American Journal of Psychiatry 153: 1593–1597.
- Tyrer P, Sensky T, and Mitchard S (2003) The principles of nidotherapy in the treatment of persistent mental and personality disorders. Psychotherapy and Psychosomatics 72: 350–356.
- World Health Organization (1992) The ICD-10 Classification of Mental and Behavioural Disorders: Criteria for Research. Geneva, Switzerland: World Health Organization.
- Zanarini MC, Frankenburg FR, Dubo ED, et al. (1998) Axis I comorbidity of borderline personality disorder. American Journal of Psychiatry 155: 1733–1739.
- Zanarini MC, Frankenburg FR, Hennen J, and Silk K (2003) The longitudinal course of borderline psychopathology: 6-year prospective follow-up of the phenomenology of borderline personality disorder. American Journal of Psychiatry 160: 274–283.
- Bateman AW and Fonagy P (2004) Psychotherapy for Borderline Personality Disorder: Mentalization Based Treatment. Oxford, UK: Oxford University Press.
- Holmes J (1999) Psychotherapeutic approaches to the management of severe personality disorder in general psychiatric settings. CPD Bulletin Psychiatry 2: 35–41.
- Livesley WJ, Jang KL, Jackson DN, and Vernon PA (1993) Genetic and environmental contributions to dimensions of personality disorder. American Journal of Psychiatry 150: 1826–1831.
- Moran P (1999) Antisocial Personality Disorder: An Epidemiological Perspective. London: Gaskell.
- Paris J (1996) Social Factors in the Personality Disorders: A Biopsychosocial Approach to Etiology and Treatment. New York: Cambridge University Press.
- Sampson M, McCubbin R, and Tyrer P (2006) Personality Disorder and Community Mental Health Teams: A Practitioner’s Guide. Chichester, UK: John Wiley and Sons.
- http://www.apa.org/topics/topicperson.html – American Psychology Association On-Line (Topic: personality disorders).
- http://www.personalitydisorder.org.uk/ – Department of Health, Home Office and Care Service Improvement Partnership. National Personality Disorder website.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








