This sample Rheumatic Fever and Rheumatic Heart Disease Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Introduction
Rheumatic fever (RF) is an inflammatory disease of connective tissues, which primarily affects the heart, major joints, and brain. It occurs secondary to a poorly adapted autoimmune response to group A streptococcal (GAS) pharyngitis and often results in chronic inflammatory damage of heart valves, i.e., rheumatic heart disease (RHD). Though RF is a noncommunicable disease, it occurs secondary to communicable streptococcal infection, and hence GAS pharyngitis treatment is important in the management of RF.
Epidemiology
Currently RF and RHD are primarily restricted to developing countries and some poor, indigenous populations of developed countries. With the improvement in socioeconomic conditions and access to medical care, the disease has become rare in developed countries except for few isolated outbreaks. According to the 2005 World Health Organization (WHO) report, at least 15.6 million people have RHD, and 0.3 million individuals with RHD are added every year to the existing burden. Two-thirds of them are from Southeast Asia and the Western Pacific. In developing countries, 60% of all cardiovascular diseases in children and young adults stem from RHD (WHO, 1994). Approximately 3 million have congestive heart failure (CHF) requiring repeated hospitalization, and 1 million are in need of corrective valvular surgery. RHD accounts for 12–65% of inpatient admissions among cardiac patients in developing countries. An estimated 6.6 million disability-adjusted life years (DALYs) are lost every year worldwide, with the range of 27.4 DALYs in the United States to 173.4 DALYs in the Southeast Asia region, per 100 000 population. The annual number of deaths from RHD is 332 000 worldwide, with the mortality rate varying from 0.5 in Denmark to 8.2 in China per 100 000 population. The disease has long-lasting adverse effects on lifestyle, employability, productivity, and healthcare costs of young people. Moreover, the burden of managing RF/RHD puts additional pressure on the health-care systems and economies of these countries, which otherwise also face the burden of epidemiological transition, i.e., a shift of a major cause of disability and death from nutritional and infectious etiologies to chronic degenerative diseases.
The prevalence of RHD varies widely among various countries. It is less than 0.5 per 1000 schoolchildren in developed countries to 5.7 in sub-Saharan Africa, 3.5 in the indigenous population of Australia, and 2.2 in southeast Asia (WHO, 2005). The available data of RF incidence are scarce. They are mainly derived from RF registries and surveys of schoolchildren. The incidence ranges from less than 1 in developed countries to more than 500 in the indigenous Australian population per 100 000 schoolchildren.
The epidemiological association between GAS pharyngitis and the subsequent development of acute RF is well established. In symptomatic children in the 5to 15-year-old age group, the cause of pharyngitis is viral in 80% and GAS in the remaining 15–20% of cases. The incidence of GAS infection can vary in different geographical areas, depending upon season, age group, socioeconomic conditions, environmental factors, and quality of health care. The true GAS infection in patients with symptomatic pharyngitis has been reported to be 13.5% from Northern India (Nandi et al., 2001), to 44.7% in Zagreb, Croatia (Begovac et al., 1993). It is estimated that each child of the susceptible age group has at least one episode of pharyngitis every year. The presence of GAS in the upper respiratory tract does not mean an active infection, because asymptomatic carriers also exist. These carriers do not show rising antistreptolysin antibody (ASO) titers and are less likely to transmit the infection to others. On the other hand, the individual with true active infection as evidenced by rising ASO titers is susceptible to RF and also capable of transmitting the infection in the community. The carrier rate of GAS in healthy schoolchildren 6–10 years of age has been reported as high as 50%; similarly the ASO titer over 200 Todd units (significant value) has been reported as high as 70% in schoolchildren from tropical countries (WHO, 1988).
Pathogenesis Of Rheumatic Fever
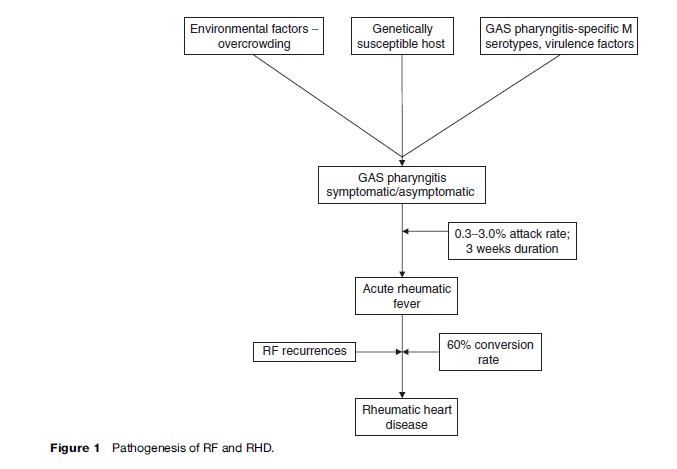
The exact mechanism of GAS pharyngitis causing RF is still unexplained. It may be an exaggerated autoimmune response of the host to GAS pharyngitis. The clinical manifestation and severity of RF/RHD in an individual depends on the virulence of the infecting organism, host susceptibility, and environmental factors (Figure 1).
The Organism (Group A Streptococcus Pyogenes)
Among the GAS, not all strains cause RF; it is believed that there are only a few virulent strains with rheumatogenic potential. The specific strains are usually heavily encapsulated and form large mucoid colonies rich in M-protein, which enhances the GAS ability to adhere to tissue and resist phagocytosis. The streptococcal M protein shares the homology with cardiac myosin and tropomyosin, connective tissue keratin and laminin, and therefore results in autoimmune response against the heart, brain, and joints. Only the 1, 3, 5, 6, 14, 18, 19 and 24 M protein serotypes are associated with RF. The role of other GAS antigens such as streptococcal erythrogenic toxin, streptococcal fibronectin binding protein 1 (sfb1), and streptococcal C5a peptidase (SCPA) have also been demonstrated in the pathogenesis of streptococcal infection.
The Host
It is consistently observed that only 0.3–3.0% of individuals with acute GAS pharyngitis develop RF, because of different genetically determined autoimmune responses and susceptibility to infection. Various genetically determined risk factors such as major histocompatible antigens, potential tissue-specific antigens, and antibody and T cell response to streptococcal infection play an important role in the pathogenesis of RF/RHD. Various studies have demonstrated the association of HLA class II alleles with RF/RHD, although the particular alleles are different in different populations: For example, HLA-DR4 is more frequent in Caucasians, HLA-DR2 in African-American populations, HLA-DR1 and DRw6 in South Africa, HLADQW2 in Asians, and HLA-DR3 in India. Association is also being described with high concentrations of mannosebinding lectin and polymorphisms of transforming growth factor-b1 and immunoglobulin genes. A B cell alloantigen D8/17 has also been found to be associated with susceptibility of acute RF (Kemeny et al., 1994). According to observations worldwide, this alloantigen expression is strongly associated with RF. Further investigations are needed before the particular alloantigen can be widely used to identify individuals at risk for RF/RHD.
Environmental Factors
The secular trends of RF/RHD over the years in developed and developing countries suggest that environmental factors such as poor living conditions, overcrowding, malnutrition and poor hygiene, and poor health-care access are the significant determinants of the disease burden and distribution. Crowded living conditions contribute to rapid spread and persistence of virulent strains in the community. Seasonal variations in the incidence of RF are more pronounced in temperate than in tropical climates.
Clinical Features And Diagnosis Of RF/RHD
The clinical features suggestive of RF were first established in 1944 by T. Ducket Jones ( Jones, 1944), and thereafter updated and modified occasionally to increase the specificity for diagnosis of RF (Table 1). Carditis is the single most important manifestation of the RF and its presence determines the course of disease, its duration, and the intensity of prophylaxis. The diagnosis of carditis is based on clinical examination, i.e., presence of significant regurgitant murmur, pericardial rub, or cardiomegaly with congestive heart failure. In case of recurrence of RF, a new murmur or a change in the character of a previously documented murmur, pericardial rub, or an increase in cardiac size with demonstration of valvular damage or involvement is required. The physician’s clinical judgment is of prime importance in diagnosis of carditis, and it can be confirmed by echocardiography, if facilities are available. Echocardiography can provide early evidence of valve involvement and confirms the rheumatic or nonrheumatic causes of murmur or valvular regurgitation. It has the definite advantage of diagnosing valvulitis in an otherwise clinically normal heart, and helps in deciding on duration of secondary prophylaxis. According to a recent study of RHD prevalence in southeast Asia and sub-Saharan Africa, the comprehensive echocardiographic screening identified approximately ten times as many children with RHD as were identified by the traditional strategy of clinical screening followed by echocardiographic confirmation (Marijion et al., 2007). This observation has an important implication for case findings, delivery of effective primary and secondary prevention, and appropriate planning for scarce health resource utilization. There is a logistic problem of routine use of echocardiography in RF diagnosis because of overdiagnosis of physiologic valvular regurgitation as pathological, the inability to diagnose subclinical carditis in patients with RF recurrence, and the lack of an echocardiography facility, affordability, or expertise at the community level. As the sizable percentage of children who have subclinical carditis are at risk for RF recurrence and progression to RHD, it is not acceptable to leave them without further management in view of nonavailability of echocardiographic screening. Further research is needed to define models of echocardiographic screening that are practical, affordable, and widely applicable in developing countries.
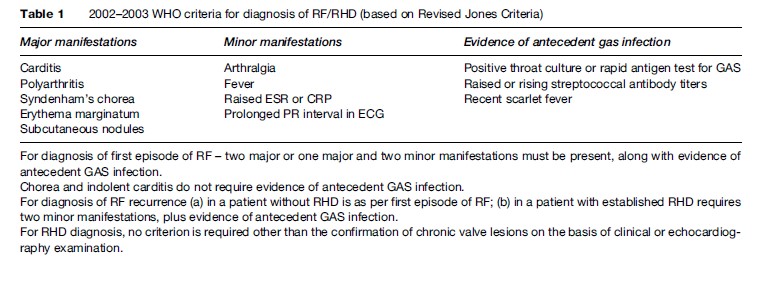
Evidence of antecedent GAS infection is required for the confirmation of an RF episode (Table 1). Only 11% of acute RF patients are found to have positive throat swab culture for GAS, as the rest of patients’ immune systems eradicate GAS during the latent period between pharyngitis and RF (Dajani, 1991). The commercially available rapid antigen test for diagnosing GAS pharyngitis has a high specificity, up to 99%, but sensitivity is only 66% in the clinical setting, requiring a backup throat swab culture in patients with negative rapid antigen test (Limbergen et al., 2006). Both positive throat swab culture and rapid antigen test do not differentiate between the recent infections leading to RF and the chronic carrier state of the organism. On the other hand, the elevated or rising ASO titers are more informative and reliable for recent GAS infection.
Treatment
Treatment of acute RF includes antibiotics, anti-inflammatory drugs, and supportive treatment. Benzathine penicillin G, 1.2 million units in a single intramuscular injection or oral penicillin V/erythromycin for 10 days must be given for GAS infection empirically. Anti-inflammatory drugs include aspirin for severe arthralgia or arthritis and steroids for significant carditis must be added. Supportive treatment includes bed rest, anti-heart failure and antipyretic drugs. Depending upon type and severity of the valvular lesion, RHD patients require long-term treatment for heart failure, atrial fibrillation, thromboembolism, and infective endocarditis as well as RF recurrence prophylaxis and interventions such as valvuloplasty or valve replacement surgery.
Prevention Of RF
Primary Prevention
The aim of primary prevention is to prevent the first attack of RF by identifying and treating all the suspected or proven streptococcal pharyngitis cases in children aged 3–15 years age. Antibiotic treatment should preferably be started within 9 days of a sore throat for effective prevention of RF development. In endemic areas, all symptomatic sore throat cases with clinical suspicion of GAS infection should be treated with antibiotics. Throat swab culture or rapid antigen test for GAS should be done if laboratory services are available; however, in the absence of these services, the antibiotics should not be delayed or avoided. Table 2 describes the antibiotic treatment for GAS throat infection. The rheumatic vaccine in the near future might be a tool for prevention of streptococcal pharyngitis and RF recurrence. Progress is continuing in development of a vaccine against M serotypes, streptococcal fibronectin binding protein-1 (sfb1), and streptococcal C5a peptidase (SCPA). However, there are practical problems in developing a vaccine such as rapid and complete change of GAS serotypes in the community, presence of asymptomatic GAS carriers, ability of streptococci to infect the host after a prior infection by a different M serotype strain, cross-reactivity of M protein vaccine with human tissues, and the cost effectiveness of the vaccine, especially in developing countries with high prevalence of GAS pharyngitis and carrier rates.
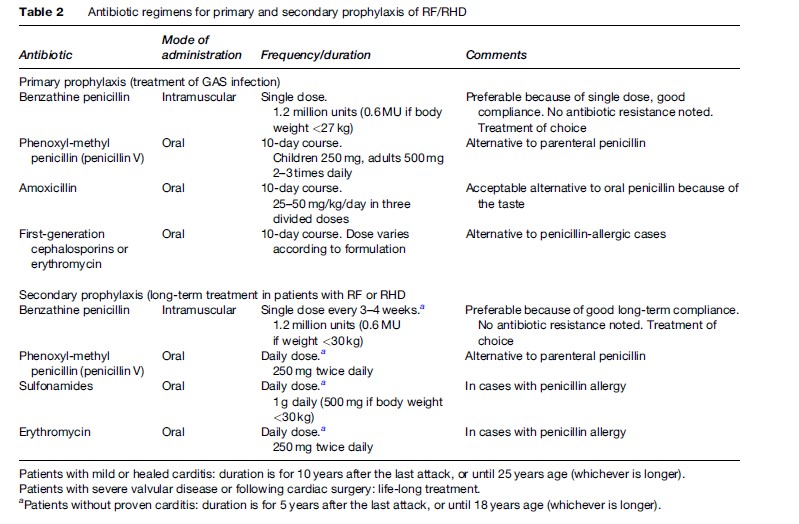
Secondary Prevention
The aim of secondary prevention is to prevent the recurrence of RF and further damage of cardiac valves in proven cases of RF/RHD. The individual who has suffered from a prior RF episode is more prone to have GAS pharyngitis and RF recurrences. The secondary prevention strategy is more practical and cost-effective than the primary prevention, especially in developing countries with limited health resources. Table 2 describes the treatment regimen for secondary prevention. Infective endocarditis is another complication with significant morbidity and mortality in patients with RHD or prosthetic valves. The routine infective endocarditis prophylaxis prior to any surgical or dental procedure is recommended in all patients with RHD.
Community-Based Measures For Prevention Of RF/RHD
Despite the appropriate primary and secondary preventive measures available for decades, the disease could not be controlled, especially in developing countries, because of social determinants such as housing, education, and poverty; health-care determinants such as access to primary health care, the scarcity of trained health-care workers, the logistics of drug supply and cost of medical treatment, and the availability of sophisticated cardiology and cardiac surgery services. It is important that the prevention and control programs to be started in the community should be cost-effective, integrated, and applicable with limited available health resources. The national programs should be planned with their objectives and approach adapted to local needs and circumstances, and they should be implemented through the existing infrastructure of the health-care and education system. There is also a need for regular surveillance of acute RF, RHD, and GAS pharyngitis in the community to provide useful information on the epidemiological trends of the disease. The national program should constitute the activities related with primary and secondary prevention, health education, and training of health-care workers.
Primary Prevention Activities
The primary prevention program is not cost-effective, particularly in endemic states, because only 10–20% of symptomatic sore throat is from GAS, one-third of all RF cases follow mild or almost asymptomatic pharyngitis, which might be missed, only less than 3% of these GAS pharyngitis evolve into RF, and approximately 60% of these RF cases continue to evolve to RHD. Also, because of limited health resources, the lack of penicillin, and populations unlikely to seek and adhere to treatment for sore throat, an alternative cost-effective strategy would be to intervene with high-risk groups. There is also a need for adequate microbiology laboratory support at peripheral, intermediate, and tertiary care levels for GAS infection identification, M subtyping, and serological investigations.
Secondary Prevention Activities
Secondary prevention is based on finding cases, referral, registration, active and passive surveillance, follow-up, and regular secondary prophylaxis of RHD patients. A local center in endemic areas should be established for referral and registration of RF/RHD patients, should be adequately equipped for laboratory tests related to RF and streptococcal pharyngitis, and should have health-care workers for medical care. The secondary prevention with penicillin prophylaxis is the most cost-effective strategy. Attention should be given for strict compliance of long-term penicillin prophylaxis in RF/RHD patients, as the defaulters are very frequent because of long-term therapy for years, painful injection, lack of health awareness and education, fear of penicillin allergy and anaphylaxis, the nonavailability of drugs, and social reasons. Strengthening diagnostic accuracy and curative services throughout the region must go hand in hand with preventive measures. Adequate infrastructures such as streptococcal diagnostic labs and echocardiography machines at the ground level with adequate expertise are essential. A lack of diagnostic and treatment facilities and the unaffordable cost of medical care add to the huge existing burden of RHD. The cost of surgery makes this option impractical for most patients. There is also a gross mismatch in the supply and demand ratio for cardiac surgery in developing countries. There are 1222 cardiac surgeries done per million population in North America, which is far more than the 25 surgeries in Asia and 18 surgeries in Africa. It is estimated that only 7% of needy patients undergo cardiac surgery in Asia, Africa, South America, and Russia. This is because of the nonavailability of infrastructure, expertise, unaffordable cost and the lack of medical insurance. Even following valve surgery, there is a need for long-term monitoring for anticoagulation treatment, infective endocarditis, bleeding and thrombotic complications, cost and availability of anti-heart failure and anticoagulant treatment in the community.
Health Education Activities
Health education activities should address both primary and secondary prevention. The activities must be organized by trained doctors, primary health-care workers, and school teachers and should be directed to the public, teachers, children, and their parents. Health education activities should focus on the importance of recognizing and reporting sore throats, methods that minimize and avoid the spread of infection, the benefits of treating sore throats properly, and the importance of complying with prescribed treatment regimens. Health education campaigns in schools and in the community, particularly in rural areas and in slums and overcrowded parts of urban areas, are effective methods for communicating health messages and awareness. The involvement of the print and electronic media (radio, TV, newsletters, posters) is vital for the success of such programs. Patients’ group meetings are also a potent means of transmitting and networking health information. The commitment of the school and school health service to the health education of children is of tremendous importance when implementing RF/RHD control programs.
Training Of Health-Care Providers
When financial resources are scarce, the available knowledge and human resources should be pooled to achieve the community’s priority goals. There should be a comprehensive and integrated approach among health-care workers for timely detection and management of streptococcal pharyngitis, RF, and RHD. They should receive adequate and appropriate training at regular intervals and should understand their roles and responsibility in RF/RHD prevention programs. There is a need for developing effective intercountry, interregional, and global networks for concerted global action to enhance the capacity of developing countries to meet their health-care needs. The developed, experienced countries can help in building infrastructure, provide the expertise, train the local physicians and surgeons, and facilitate the availability of low-cost heart valves to these countries. With the advancement in information technology, there should be more live demonstrations or video conferencing among experts in the cardiac field with those in developing countries, to help them to become independent and to improve the standard and quality of care in the field.
Bibliography:
- Begovac J, Bobinac E, Benic B, et al. (1993) Asymptomatic pharyngeal carriage of beta-haemolytic streptococci and streptococcal pharyngitis among patients at an urban hospital in Croatia. European Journal of Epidemiology 9(4): 405–410.
- Dajani AS (1991) Current status of nonsuppurative complications of group A streptococci. Pediatric Infectious Disease Journal 10: S25–S27.
- Jones TD (1944) Diagnosis of rheumatic fever. Journal of the American Medical Association 126: 481–484.
- Kemeny E, Husby G, Williams RC Jr., and Zabriskie JB (1994) Tissue distribution of antigen(s) defined by monoclonal antibody D8/17 reacting with B lymphocytes of patients with rheumatic heart disease. Clinical Immunology and Immunopathology 72: 35–43.
- Limbergen JV, Kalima P, Taheri S, and Beattie TF (2006) Streptococcus A in paediatric accident and emergency: Are rapid streptococcal tests and clinical examination of any help? Emergency Medical Journal 23: 32–34.
- Marijon E, Ou P, Celermajer DS, et al. (2007) Prevalence of rheumatic heart disease detected by echocardiographic screening. New England Journal of Medicine 357(5): 470–476.
- Nandi S, Kumar R, Ray P, Vohra H, and Ganguly NK (2001) Group A streptococcal sore throat in a periurban population of Northern India: A one-year prospective study. Bulletin of the World Health Organization 79: 528–533.
- World Health Organization (1988) WHO Technical Report Series 764. Rheumatic Fever and Rheumatic Heart Disease. Report of a WHO Study Group Geneva: World Health Organization.
- Bach JF, Chalons S, Forier E, et al. (1996) 10-year educational programme aimed at rheumatic fever in two French Caribbean islands. Lancet 347: 644–648.
- Bisno AL, Gerber MA, Gwaltney JM Jr., Kaplan EL, Schwartz RH, and Infectious Diseases, Society of America (2002) Practice guidelines for the diagnosis and management of group A streptococcal pharyngitis. Infectious Diseases Society of America. Clinical Infectious Diseases 35(2): 113–125.
- Carapetis JR, Currie BJ, and Mathews JD (2000) Cumulative incidence of rheumatic fever in an endemic region: A guide to the susceptibility of the population? Epidemiology and Infection 124: 239–244.
- Carapetis JR, McDonald M, and Wilson NJ (2005a) Acute rheumatic fever. Lancet 366: 155–168.
- Carapetis JR, Steer AC, Mulholland EK, and Weber M (2005b) The global burden of group A streptococcal diseases. Lancet Infectious Diseases 5(11): 685–694.
- Cox JL (2001) Presidential address: Changing boundaries. Journal of Thoracic Cardiovascular Surgery 122(3): 413–418.
- Dajani AS, Ayoub E, Bierman FZ, et al. (1992) Guidelines for the diagnosis of rheumatic fever: Jones criteria 1992 Update. Journal of the American Medical Association 268: 2069–2073.
- Grover A, Dhawan A, Iyengar SD, Anand IS, Wahi PL, and Ganguly NK (1993) Epidemiology of rheumatic fever and rheumatic heart disease in rural community in northern India. Bulletin of the World Health Organization 71: 59–66.
- Kaplan EL (1993) Global assessment of rheumatic fever and rheumatic heart disease at the close of the century. Influences and dynamics of populations and pathogens: A failure to realize prevention? Circulation 88: 1964–1972.
- Kaplan EL (2005) Pathogenesis of acute rheumatic disease: Evasive after half a century of clinical, epidemiological, and laboratory investigations. Heart 91: 3–4.
- Kaplan EL, Wotton JT, and Johnson DR (2001) Dynamic epidemiology of group A streptococcal serotypes associated with pharyngitis. Lancet 358(9290): 1334–1337.
- Kotloff KL and Dale JB (2004) Progress in group A streptococcal vaccine development. Pediatrics Infectious Disease Journal 23: 765–766.
- Stollerman GH (1997) Rheumatic fever. Lancet 349: 935–942.
- World Health Organization and International Society and Federation of Cardiology (1994) Joint WHO/ISFC Meeting on RF/RHD Control with Emphasis on Primary Prevention, Geneva. 7–9th September 1994, Document WHO/CVD 94.1.Geneva: World Health Organization.
- World Health Organization (2001) WHO Technical Report Series 923: Rheumatic Fever and Rheumatic Heart Disease. Report of WHO expert consultation. Geneva, 29 October to 1 November 2001.
- World Health Organization (2005) The Current Evidence for the Burden of Group A Streptococcal Diseases. Discussion Paper on Child Health, pp. 1–52. WHO/FCH/CAH/05.07. Geneva: WHO.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.






