This sample Severe Acute Respiratory Syndrome (SARS) Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Background
The worldwide panic and chaos that resulted from the outbreak of severe acute respiratory syndrome (SARS) in February 2003, caused by a novel coronavirus (SARSCoV), was unprecedented for the twenty-first century (Tsang et al., 2003). SARS rapidly spread via Hong Kong to the rest of Asia, North America, and Europe within a few months, affecting 8437 patients with a mortality rate of 9.6%. In May 2005, SARS was declared ‘eradicated’ by the World Health Organization (WHO), thus becoming the second human disease, after smallpox, to receive this label. Coronaviruses isolated from civet cats and other game animals in China have remarkable sequence homology with SARS-CoV, suggesting a zoonotic origin.
Clinical Pathology
There are three nondistinct theoretical phases of SARS, namely viral replication, inflammatory pneumonitis, and pulmonary fibrosis. Shedding of SARS-CoV, as evaluated by reverse-transcriptase (RT)-PCR, peaks at 6 to 11 and 9 to 14 days after onset of fever for nasopharyngeal aspirates and feces, respectively.
Autopsy studies on SARS lungs only reveal nonspecific features including diffuse alveolar damage, secondary bacterial pneumonia, and giant cell and macrophage infiltration of alveoli and lung interstitium (Nicholls et al., 2003). The presence of subpleural fibro-granulation proliferation in small airways and air spaces is similar to bronchiolitis obliterans with organizing pneumonia, a steroid-responsive immune-mediated pneumonitis. Four out of 8 SARS patients had pulmonary thromboemboli, which is otherwise an unusual condition among Asians.
Clinical Features
SARS-CoV appears to spread mainly by droplet transmission, although fomites and feces are also possible modes for human transmission. Airborne transmission might have contributed to an outbreak in Amoy Gardens, a residential complex in Hong Kong, where hundreds of people were infected.
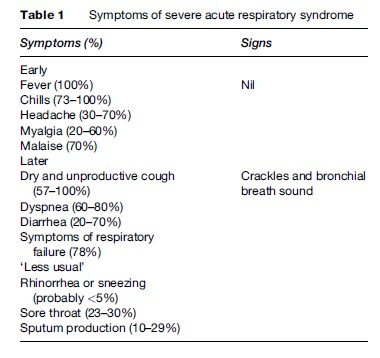
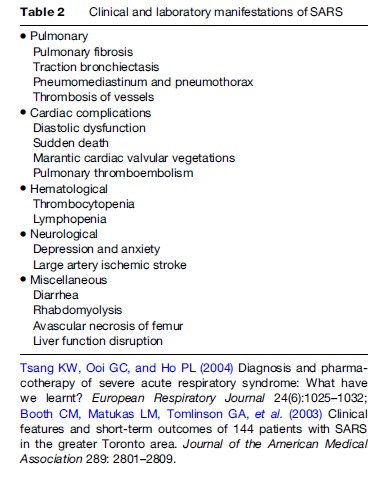
The mean incubation period of SARS is 6.4 days (2 to 10 days), and the clinical features are summarized in Table 1. The key feature is the occurrence of rapidly progressive pneumonia, sometimes with dramatic overnight progression from a mild to bilateral pneumonia and then acute respiratory distress syndrome. The occurrence of upper respiratory tract symptoms is unusual. Patients with diarrhea could potentially be highly infectious. Physical signs are scarce in the first few days but become more prominent as patients develop extensive lung consolidation. Although SARS is predominantly a respiratory illness, extrapulmonary manifestations are not infrequently encountered (Table 2).
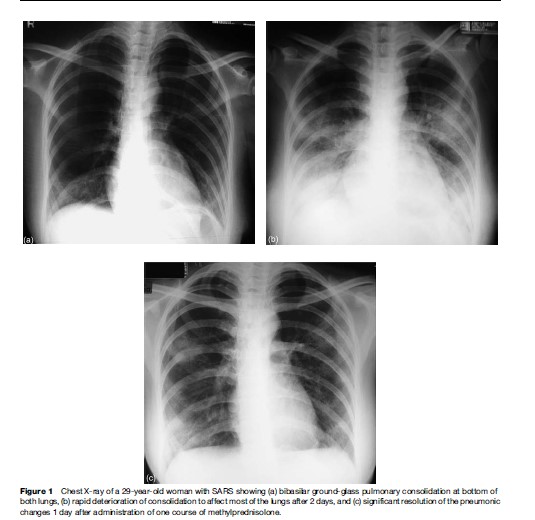
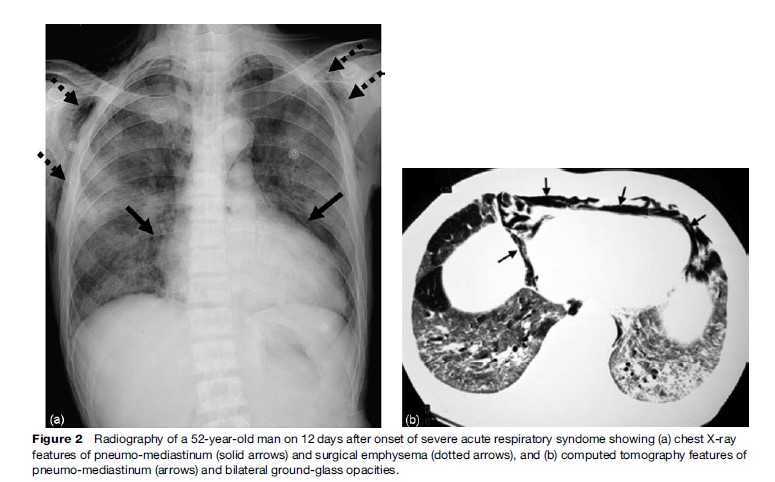
At fever onset, 80% of SARS patients have airspace consolidation, especially peripheral and lower zone in distribution, on their chest radiographs (Ooi et al., 2003; Tsang et al., 2004). Generally, rapid deterioration of groundglass consolidation occurs in the first 3 days, peaking between 8 and 10 days after onset of fever to become multilobar and bilateral (Figure 1). Pneumomediastinum and pneumothoraces, often spontaneous but also occurring with assisted ventilation, can complicate extensive disease (Figure 2).
Diagnosis
The current WHO diagnosis of SARS entails demonstration of clinical features (fever ≧38 C, respiratory symptoms, radiographic pneumonia, and autopsy results of consistent pathology in otherwise unexplained illness) and the presence of virological proof of SARS-CoV infection (i.e., positive RT-PCR for presence of SARS-CoV RNA, seroconversion with significant antibody rise in paired sera, or virus isolation). Practically, prerequisites for the diagnosis of SARS include the presence of an epidemiological linkage, rapidly progressive pneumonia resistant to standard treatment, clinical features, and virological evidence of SARS-CoV infection. An epidemiological link, defined as a history of contact with a SARS patient or visiting a hospital with nosocomial SARS outbreak, in the 10 days preceding disease onset, is useful even for patients in areas with outbreaks. Virtually all patients deteriorate despite potent antibiotic therapy (Tsang et al., 2003), and most have lymphopenia and raised transaminase levels.
Treatment
The treatment for SARS, administered amid the crisis situations in 2003, is largely anecdotal and without backing from controlled trial data.
Pharmacotherapy Of SARS
Theoretically, none of the manifestations of SARS would occur if an efficacious antiviral agent is given at disease onset. However, agents of proven efficacy are not available despite prolific suggestions. Apart from administering empirical antibiotic therapy for severe community acquired pneumonia, controlled clinical trials should be conducted to evaluate the efficacy of potential antiviral and immunomodulating agents. Clinical experience is only available on a few agents used in the 2003 outbreak, namely ribavirin, ritonavir/lopinavir, interferons, corticosteroids, immunoglobulin, and convalescence serum.
Historically, and before SARS was even defined by the WHO, patients were treated with a broad-spectrum antiviral agent, namely ribavirin, and corticosteroid. About 60% of patients dropped their hemoglobin by 2 g/dl after treatment with ribavirin (1.2 g tid) for two weeks, and higher doses were associated with elevated liver transaminase levels and bradycardia (Booth et al., 2003). The rapid recovery of the first few Hong Kong patients had led to the adoption of the above as standard antiSARS regimen in Hong Kong and elsewhere in 2003. Ribavirin is now considered to be ineffective. The efficacy of other possible anti-SARS-CoV agents such as antiproteases like Kaletra (ritonavir 400 mg and lopinavir 100 mg for 14 days), in combination with ribavirin as initial treatment, was associated with reduction in mortality (2.3% vs. 15.6%) and intubation rate (0% vs. 11%) when compared with historical controls (Chu et al., 2004). It appears, therefore, that ritonavir/lopinavir could be considered for early treatment of SARS patients, preferably in a controlled clinical trial setting. Adverse reactions are not infrequent and include severe pancreatitis, diarrhea, abdominal pain, asthenia, headache, nausea, insomnia, and skin rash.
Interferon b-1b, a-n1, and a-n3 and human leukocyte interferon a exhibit complete inhibition of cytopathic effects of SARS-CoV in vitro. SARS patients treated with corticosteroids and interferon alfacon-1 had less ICU admission, mechanical ventilation, and death than their counterparts (Loutfy et al., 2003).
SARS-CoV is an enveloped RNA virus that contains several structural proteins. Currently, different vaccines such as whole killed vaccine, adenovirus vector vaccine, and recombinant spike protein vaccine are being tested among laboratory animals, but none are ready for largescale clinical trials.
Immunomodulating Agents
Administration of corticosteroids to deteriorating SARS patients was associated with significant and sometimes dramatic radiographic and clinical recovery (Figure 1). Despite skepticism, immunomodulating drugs could be considered as rescue therapy. Patients who had pulse steroid therapy (e.g., methylprednisolone 250 to 500 mg daily for 3 to 5 days) did not have higher cumulative steroid dosage or side effects, but had less oxygen requirement and better radiographic outcome, than their counterparts (Ho et al., 2003). Although a retrospective analysis showed a higher 30-day mortality among patients who had pulse methylprednisolone, this could be due to the higher likelihood of using such therapy in more severe SARS cases. Corticosteroids are effective anti-inflammatory agents that significantly reduce interleukin-8, monocyte chemoattractant protein-1, and IFN-g inducible protein- 10 levels in SARS (Wong et al., 2004). The use of highdose steroids was associated with sepsis, particularly ventilator-associated pneumonia, and even systemic fungal infection. Approximately 15% of SARS patients had MRI-proven avascular necrosis (AVN) of the hips and knees (Griffith et al., 2005), which could be steroid-induced, but this incidence seems much higher than that among recipients of organ transplants despite similar steroid dosages.
Intravenous gammaglobulin (IVIg) may downregulate cytokine expression in SARS. However, ill patients who received IVIg developed pulmonary embolism and large artery ischemic stroke despite prophylactic low-molecularweight heparin. Treatment with pentaglobin, a commercially available IgM-enriched IVIg with theoretical enhanced immunomodulating effect, was associated with improved oxygenation and radiographic scores.
Miscellaneous Agents
Convalescence serum was administered to 19 Hong Kong SARS patients in 2003, and recipients had a shorter hospital stay and lower mortality than their counterparts (Soo et al., 2004). The possible transmission of SARS-CoV (and other pathogens), theoretical disadvantages of its proinflammatory actions, and its current unavailability make this mode of potential therapy unacceptable. Numerous other agents have been proposed to be potentially efficacious for SARS, by virtue of their in vitro or merely theoretical activities against SARS-CoV. These include glycyrrhizin (licorice extract), synthetic RNA duplexes targeting both SARS-CoV genomes, nelfinavir, aminopeptidase N inhibitor, niclosamide, rhinovirus 3C proinhibitor analogs, anti-tumor necrosis factor-a, heparin and antiplatelet agents, sodium nitroprusside, and monoclonal antibody against S1 protein (Tsang et al., 2004).
Noninvasive Positive Pressure Ventilation (Nippv)
About 20% of SARS patients developed acute respiratory distress syndrome requiring invasive mechanical ventilation, which was associated with nosocomial spread of SARS. However, NIPPV usage among Hong Kong SARS patients was found to be effective in oxygenation and preventive for intubation, with no evidence of nosocomial spread of SARS (Cheung et al., 2004).
Prognosis
The average hospitalization duration was 21 days for most of the Hong Kong patients in 2003, with a 21-day mortality of 3.6 to 10%. The final case fatality ratio was 17% for both Hong Kong and Canada, due to a much higher mortality among those with poorer prognosis. Poor prognostic factors predictive of ICU admission or death include advanced age, chronic hepatitis B treated with lamivudine, diabetes mellitus or other comorbid conditions, high serum lactate dehydrogenase and high neutrophil count, and low CD4 and CD8 lymphocyte counts. Rehabilitating SARS patients exhibit high incidence of mood and stress-related disorders. Recurrence of SARS among survivors has not been reported.
Infection Control
The most important control for SARS is to ensure no more outbreaks within the hospitals as well as the community. Details on such measures would be beyond the scope of this research paper. Very briefly, patients should be isolated promptly to ensure no more spread of SARS-CoV to other fellow patients and staff. Isolated nursing could be achieved in dedicated single rooms or on open wards, as long as these are closely supervised and maintained. An air exchange rate of 12 times per hour and a temperature of 20 C appeared desirable, as the wearing of personal protective equipment (PPE) by staff could be too warm at times. Personal protective equipment should be provided to trained staff including the use of full-body gowns and high-specification masks (such as N95 masks). All staff are required to follow strict and stepwise ‘gowning’ and ‘degowning’ procedures. Strict personal hygiene and common sense are important. Diluted bleach is used to wipe all work surfaces and the floor every hour or after any potential contamination. As nebulizer therapy was alleged to be the cause of a major hospital outbreak in Hong Kong, this mode of therapy is forbidden for patients with suspected or probable SARS in Hong Kong.
Bibliography:
- Booth CM, Matukas LM, Tomlinson GA, et al. (2003) Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. Journal of the American Medical Association 289: 2801–2809.
- Cheung TM, Yam LY, So LK, et al. (2004) Effectiveness of noninvasive positive pressure ventilation in the treatment of acute respiratory failure in severe acute respiratory syndrome. Chest 126: 845–850.
- Chu CM, Cheng VC, Hung IF, et al. (2004) Role of Lopinavir/ritonavir in the treatment of SARS: Initial virological and clinical findings. Thorax 59: 252–256.
- Griffith JF, Antonio GE, Kumta SM, et al. (2005) Osteonecrosis of hip and knee in patients with severe acute respiratory syndrome treated with steroids. Radiology 235: 168–175.
- Ho JC, Ooi GC, Mok TY, et al. (2003) High-dose pulse versus nonpulse corticosteroid regimens in severe acute respiratory syndrome. American Journal of Respiratory and Critical Care Medicine 168(12): 1449–1456.
- Loutfy MR, Blatt LM, Siminovitch KA, et al. (2003) Interferon alfacon-1 plus corticosteroids in severe acute respiratory syndrome: A preliminary study. Journal of the American Medical Association 290: 3222–3228.
- Nicholls JM, Poon LL, Lee KC, et al. (2003) Lung pathology of fatal severe acute respiratory syndrome. Lancet 361: 1773–1778.
- Ooi GC, Khong PL, Ho JC, et al. (2003) Severe acute respiratory syndrome: Radiographic evaluation and clinical outcome measures. Radiology 229: 500–506.
- Soo YO, Cheng Y, Wong R, et al. (2004) Retrospective comparison of convalescent plasma with continuing high-dose methylprednisolone treatment in SARS patients. Clinical Microbiology and Infection 10: 676–678.
- Tsang KW, Ho PL, Ooi GC, et al. (2003) A cluster of cases of severe acute respiratory syndrome in Hong Kong. New England Journal of Medicine 348(20): 1977–1985.
- Tsang KW, Ooi GC, and Ho PL (2004) Diagnosis and pharmacotherapy of severe acute respiratory syndrome: What have we learnt? European Respiratory Journal 24(6): 1025–1032.
- Wong CK, Lam CWK, Wu AK, et al. (2004) Plasma inflammatory cytokines and chemokines in severe acute respiratory syndrome. Clinical and Experimental Immunology 136: 95–103.
- Chan PK, To WK, Ng KC, et al. (2004) Laboratory diagnosis of SARS. Emerging Infectious Disease 10(5): 825–831.
- Ho PL, Chau PH, Yip PS, et al. (2005) A prediction rule for clinical diagnosis of severe acute respiratory syndrome. European Respiratory Journal 26(3): 474–479.
- Jones BM, Ma ES, Peiris JS, et al. (2004) Prolonged disturbances of in vitro cytokine production in patients with severe acute respiratory syndrome (SARS) treated with ribavirin and steroids. Clinical and Experimental Immunology 135(3): 467–473.
- Ooi GC, Khong PL, Muller NL, et al. (2004) Severe acute respiratory syndrome: Temporal lung changes at thin-section CT in 30 patients. Radiology 230: 836–844.
- Tsang KW and Lam WK (2003) Management of severe acute respiratory syndrome: The Hong Kong University experience. American Journal of Respiratory and Critical Care Medicine 168(4): 417–424. Respirology 8(supplement 1): S1–S48.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








