This sample Sexual Health Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Introduction
Defining The Area Of Sexual Health
Sexual health is often seen in terms of the prevention of adverse outcomes of sexual behavior, such as unplanned pregnancy and sexually transmitted infections (STIs). The definition of sexual health formulated by the World Health Organization as a guide for those working in this public health field, however, incorporates more positive and pleasurable aspects of sexual health, so broadening the public health remit to include the enhancement of life and personal relations, and not merely counseling and care related to reproduction and STIs:
Sexual health is a state of physical, emotional, and social well-being in relation to sexuality; it is not merely the absence of disease, dysfunction or infirmity. Sexual health requires a positive and respectful approach to sexuality and sexual relationships, as well as the possibility of having pleasurable and safe sexual experiences, free of coercion, discrimination and violence. For sexual health to be attained and maintained, the sexual rights of all persons must be respected, protected and fulfilled. (WHO, 2006)
The past decade has seen growing attention in the international policy arena to sexual rights, and new standards have been formulated for the creation and maintenance of a sexually healthy society, invoking values of respect and choice (Miller and Vance, 2004).
Barriers To The Achievement Of Sexual Health
Sexual health presents particular challenges to public health. The human behaviors involved are not only for the most part personal and private, but are often stigmatized and discriminated against. As a result, those who practice them are often hidden or difficult to reach. This has consequences for sexual health status at a number of levels. Men and women may feel unable to talk about safer sex; they may feel disinclined to seek help; politicians may be unwilling to support provision of services for some populations; and service providers may feel unable to reach people in need of help, or may have negative attitudes toward them.
The Public Health Burden
Efforts to improve sexual health are vital to the achievement of the Millennium Development Goals on gender equality, maternal health, and HIV/AIDS. Sexual ill-health contributes significantly to the global burden of disease (Ezzati et al., 2003). The impact of the HIV epidemic is well documented. By the end of 2007, more than 30 million people worldwide were living with HIV, 15 million of whom were women, and 2.5 million, children (UNAIDS and WHO, 2007). HIV/AIDS is responsible for 6% of the global burden of disease. In developing countries, STIs and their complications are among the top five diseases for which adults seek care and are a major cause of infertility.
Sexual and reproductive ill health accounts for one third of the global burden of disease among women of reproductive age and one-fifth of the burden of disease among the population overall (Ezzati et al., 2003). Unintended pregnancy often leads to unsafe abortion, which in turn may lead to other health consequences, such as reproductive tract infections, pelvic pain, and infertility.
The burden of sexual ill health due to STIs varies markedly between populations, since transmission patterns relate to both patterns of sexual behavior and access to treatment. Congenital syphilis, for example, is rare in Western countries but is a major cause of infant mortality and morbidity in resource-poor countries lacking effective screening and treatment programs. Similarly, the advent of highly active anti-retroviral therapy (HAART) has considerably increased survival rates for HIV in developed countries, while prognoses in poor settings where HAART is unavailable are still poor.
Sexual health problems also include sexual dysfunction, sexual violence, and discrimination on the basis of sexual orientation. Global estimates of lifetime prevalence of sexual violence by an intimate partner range from 10–50%. Population-based estimates of the prevalence of sexual dysfunction vary greatly. In developed countries, the range is from 1 in 12 to 1 in 3 of the adult population (Laumann et al., 1999) and a pan-European study of women (Graziottin, 2007) also showed large differences between countries. The variation stems largely from differences in defining and measuring the problem. Persistent lack of interest in or desire for sex is classified as a disorder of sexual function both by ICD-10 (WHO, 1992) and the DSM-IV-TR (American Psychiatric Association, 2000). Yet sexual interest varies across age, gender, cultural context, and sexual orientation, and attempts to define ‘abnormal’ must be made with caution.
The concept of ‘psychosexual dysfunction,’ which first appeared in the third edition of the DSM (DSM-III) (American Psychiatric Association, 1980), was based on a biomedical model of sex involving physical processes such as lubrication and orgasm, and stages of desire, arousal, and orgasm. Subsequent revisions of the DSM have reflected advances in thinking about the nature of sexual difficulties, in particular, the concern to avoid labeling temporary alterations in sexual performance as ‘sexual dysfunction’ and to broaden the diagnostic criteria to include duration of, and distress caused by, the problem, and the extent to which it reflects the relationship context (Balon et al., 2007). Increasing use of sildenafil citrate (Viagra) has helped many people, but there is growing recognition that pharmacological solutions are likely to prove effective only if psychosocial issues are also dealt with, and if medical treatment and sex therapy are combined.
Risk Behaviors
Trends And Patterns
An understanding of trends and patterns in sexual behavior is essential to the design of public health interventions to improve sexual health status. Marked shifts in sexual behavior have occurred in the past half century. These include demographic changes in the age structures of populations, in the timing of marriage, and in the scale of mobility and migration between and within countries. The increase in intra and international travel, particularly, has played its part in increasing possibilities for the transmission of STIs, including HIV. The HIV epidemic has significantly influenced the context in which sexual behavior occurs, providing the impetus for public discussion of sexual matters, research on the subject, and innovation in interventions designed to improve sexual health.
Policy and legislation governing health-care systems and public health strategies have also brought about changes. The advent of reliable contraception has increasingly freed sexual expression from its reproductive consequences. Access to family planning services has increased, and few areas have been unaffected by efforts to prevent HIV transmission. Attitudes toward sexual behavior have altered in many countries (Wellings et al., 2006). Global communications, including the Internet, have had a bearing on social norms, transporting Western sexual images to more conservative societies, particularly those in which advances in information technology have been rapid.
Given these trends, surveys of sexual behavior show perhaps less change over time than might have been supposed. Considerable public health interest surrounds onset of sexual activity, since early sexual intercourse is more likely to be nonconsensual, to be regretted, to be unprotected against unplanned pregnancy and infection, and to be associated with larger lifetime numbers of sexual partners. Trends toward early and premarital sex are less marked than is sometimes assumed. In countries in which first intercourse still occurs predominantly within marriage, the trend toward later marriage has been accompanied by a trend toward later sex among young women. In industrialized countries, sexual activity before age 15 has become more common in recent decades but the prevalence is low. The trend toward later marriage has led to an increase in the prevalence of premarital sex in some, but not all, countries.
Multiple sexual partnerships increase the risk of STIs and HIV. The majority of people report only one sexual partner in the past year. The prevalence of multiple partnerships varies regionally but is notably higher in industrialized countries. However, rates of condom use are lower in countries with lower sexual health status, and this is likely to be attributable to factors relating to access and service provision.
Risk Factors And Risk Groups
Sexual ill health affects all age groups and sections of society, but some groups are more vulnerable than others. Young people, minority ethnic groups, and those affected by poverty and social exclusion are disproportionately affected. Globally, young, sexually active people are at highest risk of unplanned pregnancy and STIs. Preventive efforts also focus on men who have sex with men, a particularly high-risk group for HIV and other STIs.
Mean partner numbers are higher among male and female sex workers. (In addition to the formal trading of sex for money, sex may be exchanged for gifts or favors within personal relationships, and hence the term ‘transactional sex’ is sometimes preferred.) However, the primary risk for STIs among commercial sex workers is unprotected sex with high-risk regular partners. In countries with wide gender differences between men and women in the prevalence of premarital sex, young men are more likely to report sex with sex workers. Clients of sex workers are important bridging groups in the transmission of STIs and HIV to wider sexual networks.
A focus on behaviors in addition to groups is needed in a public health context, since risk behaviors are not necessarily limited to the traditional high-risk groups. Many men who have sex with men, for example, have also had sex with women and, except in the West, are unlikely to identify as ‘gay.’ An individual’s risk depends also on his or her partner’s risk. Monogamous women in many parts of the world may be more susceptible to sexually transmitted infection on account of their partner’s risk behavior, yet may be unable to negotiate condom use (Clark, 2004). Similarly, simply identifying the ‘multi-partnered’ will not help target men and women at greatest risk. Increasingly, high rates of concurrent partnerships are thought to contribute substantially to the global HIV epidemic (Kretzschmar and Morris, 1996). Concurrent sexual partnerships (those that overlap in time) allow more rapid spread of STIs, including HIV, than the same rate of new sequential partnerships.
Social And Environmental Factors
Social and environmental factors are powerful influences shaping sexual behavior and its consequences for sexual health. Poverty, deprivation, and unemployment, for example, contribute markedly to sexual ill health. Economic adversity limits the power of men and women to take control over their health; unemployment may drive men and women to sell sex or travel greater distances to work. Being away from home is associated in both developed and developing countries with concurrent partnerships, disruption of existing partnerships, and an increase in risk behaviors (Figure 1).
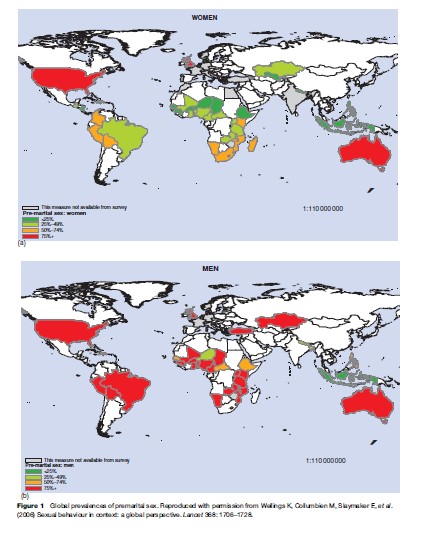
There are striking differences between men and women in sexual behavior, and these are most pronounced in the less industrialized countries (Wellings et al., 2006). Men report more premarital sex and multiple partnerships than women in all but the more industrialized countries. The sexual ‘double standard,’ whereby restraint is expected of women while excesses are tolerated for men, compounds the problems for both men and women. Reporting bias doubtless accounts for some of these differences, but in some areas, for example, in Africa, the difference can be largely explained by the age structure and patterns of age mixing, that is, older men having sex with younger women. Women may be disadvantaged in protecting their sexual health when their partner is senior to them in age and/or superior in status, and when they are beholden to a man for favors, goods, or money in return for sex.
Possibly the most powerful influences on human sexuality are the social norms governing its expression. Morals, taboos, laws, and religious beliefs employed by societies the world over circumscribe and radically determine the sexual behavior of their citizens. Such strictures may have been instituted to protect well-being and rights, yet they may also hinder attempts by both men and women to protect their sexual health, and they strongly influence the selection of acceptable public health messages. In some countries, such as Brazil, condoms are available to young people in schools; in others, such as parts of Indonesia, possession is a criminal offence.
Nowhere are social norms more strongly felt than in the area of homosexual activity. In some parts of the world, sex between men can be celebrated in public parades of pride; in others, it carries the death penalty. Whether sexual orientation is innate is an issue that is hotly contested in scientific circles, but more important from a public health perspective is the issue of sexual identity, a term used to refer to the way in which an individual sees him-or herself and is seen by others. Where cultures stigmatize homosexual behavior and relationships, men and women may be wary of assuming an openly gay identity. Behaviors that are discriminated against may be driven underground, thwarting public health initiatives to protect sexual health. Homophobic attitudes may have a negative impact on mental health, including a higher incidence of depression and suicide. In its extreme form, homophobia can lead to violence; studies have shown that 80% of gay men and lesbians had experienced verbal or physical harassment on the basis of their orientation.
Effective Public Health Strategies
Interventions Aimed At Individual Behavior Change
Men and women have sex for different reasons and in different ways in different settings. This diversity needs to be respected in a range of approaches tailored to specific populations and to particular groups and individuals within them. The repertoire of public health approaches is broad and includes health promotion, social marketing, media advocacy, health service provision, legislative activities, and community empowerment.
Approaches based on voluntary individual behavior change continue to be a central plank of public health policy. Interventions, however, focusing on provision of information alone have been shown to be less effective than those including the development of skills relating to condom use and negotiation of safer sex that use multiple delivery methods, and take account of the social context and the need for sustainability (Rotheram-Borus et al., 2000).
Mass media campaigns can be effective in bringing sexual health issues to the attention of the broad mass of the public, in increasing knowledge, and in influencing social norms, but they are less effective in increasing self-efficacy and personal skills (Bertrand et al., 2006).
To be successful, individual-based interventions also need to be targeted, in the workplace, for example, and in school settings. The evidence is that curriculum-based sex education does not increase risky sexual behavior as is sometimes feared, but instead is likely to increase the practice of safer sex and delay, rather than hasten, the onset of sexual activity (Santelli et al., 2007).
Risk-reduction messages need to take account of the diversity of sexual behavior and the need for people to be able to act on them. Options in public health may include advice to abstain from sex, to have sex with only one partner, or to practice safer sex. Considerable debate takes place over the relative merits of each of these. Research has shown that a significant proportion of young women and men first have sex before they are ready, and so efforts to help young people optimize the timing of first intercourse, and to resist unwanted sex, are justified. Yet abstinence may not be an option where first sexual relations may be forced, where the sexual abuse of adolescents is common, and where financial circumstances force young people to sell sex. A WHO study has shown that over 30% of women who first had sex before the age of 15 years described having been forced to do so (Garcia-Moreno et al., 2005). Similarly, advice to an individual to be monogamous may not reliably safeguard sexual health where men and women are put at risk by their partners’ risk behavior. In Uganda, married women constitute the population group among whom HIV transmission is increasing most rapidly. Married women find it more difficult than single women to negotiate safer sex, and fewer use condoms for family planning.
Interventions also need to address the social norms influencing sexual health. Efforts on the part of professional educators and the medical profession need to be supported by those working at the grassroots level. Community-level interventions have been effective in mobilizing local groups in support of preventive strategies. Information gained through social networks is more salient, and more likely to lead to behavior change, than that conveyed by more impersonal agencies (McIntyre, 2005). The prompt response from gay communities to the prevention of HIV/AIDS in Western countries in the early 1980s owed much to the preexistence of infrastructures in the nongovernmental sector and to the visibility and mobilization of gay men. Preventive programs using naturally occurring social networks have been used to reduce levels of risky behavior among gay men in Russia and to increase contraceptive use among married women in Bangladesh and condom use among sex workers in India; and have proved more effective in changing norms than more orthodox approaches using conventional health care and field workers.
Sexual behavior is subject to extensive legislation, and this also has implications for sexual health. In general, laws protect the young and those vulnerable to coercion and exploitation, but they may also impede safer sex practices. Where sexual practices are illegal, they are more likely to be engaged in in a furtive or clandestine manner, and people may have fewer opportunities to protect themselves. For example, condom use is uncommon among sex workers in India, where commercial sex is heavily socially proscribed, but is near-universal among those in Kampala and Mexico, where public health agencies have been able to adopt a more open approach.
Intervention At The Level Of The Social Context
Patterns of risk behavior vary between cultures and regions, as do patterns of sexual health status, yet often there is no obvious association between the two. The link between sexual behavior and rates of STIs/HIV and unplanned pregnancy is not always seen. It has been difficult to explain differences in patterns of HIV transmission in Africa and in the West, for example, by reference to differences in sexual behavior, and evaluation studies have not always shown a link between behavior change and health outcomes. The prevalence of multiple partnerships is comparatively high in the richer countries of the West, yet it is the poorer countries of the world that have higher rates of STIs and HIV (Wellings et al., 2006). The impact of poor sexual and reproductive health falls hardest on the most disadvantaged groups, and disproportionately affects women in low-income countries (Figure 2).
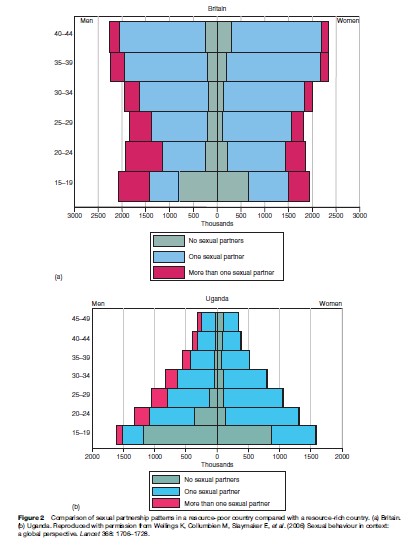
This has led to pleas for a public health focus on the broader determinants of sexual health such as poverty, mobility, and gender. Interventions need to be pitched not only at the individual level but also at the level of the social context within which sex occurs. Individual level intervention may have less chance of success in settings in which people have less control over their lives. In particular, individual-level interventions may have less chance of success where sex is tied to livelihoods, duty, and survival, and individual agency is more limited. In wealthier countries, personal choice is greater, yet power inequalities persist.
Addressing the broader social influences on sexual behavior, however, presents considerable challenges for public health. Structural factors like poverty, unemployment, and gender are hard to modify, and social and political norms are slow to shift. Yet efforts are being made to address macro-level forces such as gender and poverty in innovative approaches linking health with development, for example, by empowering sex workers to avoid sex work through business and information technology training. In South Africa, a current sexual rights advocacy campaign is focused on achieving a more comprehensive perspective of sexual health and rights into prevention work, involving working with nongovernmental and community-based organizations to address HIV/ AIDS, violence against women, and adolescent sexual health in an integrated manner.
Tackling determinants of sexual health, such as poverty, requires coordination and collaboration across health and social sectors and agencies. Partnerships need to be forged between public health personnel and, for example, economists, politicians, industry, the judiciary, and nongovernmental organizations. Improvements in sexual health are generally achieved as a result of a combination of preventive policies and strategies mounted by different agencies, with strong partnerships between the media, government, nongovernmental organizations, sex workers, the AIDS community, and international and local public health agencies, endorsed at the highest political level.
The need for preventive approaches that are multilevel and multipartnered, that have strong support from government, and that promote messages carefully tailored to the local context is demonstrated in many of the success stories in public health: the successes of Thailand and Uganda in reducing HIV rates, for example, and of the United States in reducing teenage pregnancy rates. The 100% condom-use program in Thailand, which achieved increasing rates of condom use and reduced STI and HIV rates and sex work activity, incorporated a variety of components, such as free condom provision; mass media campaigns and workplace programs; regular check-ups for STIs and encouragement of testing and treatment among sex workers; extensive contact tracing; and legal action against brothel owners not implementing the program (Nelson et al., 1996). Coordination between national and local governments, public health officials, and brothel owners was a strong characteristic of the program and the approach was pragmatic, involving tacit acceptance of sex work.
By the same token, Uganda’s past success in reducing HIV prevalence and improving reproductive health status compared with neighboring countries has been attributed to the careful tailoring of messages to cultural context; the successful assimilation of scientific knowledge about modes of transmission; restoration of stability following the end of the Ugandan civil war in 1986; and two decades of strong policy support (Parkhurst, 2002). Uganda was the first African nation to establish a national AIDS program, and the response to the epidemic went beyond the individual-level factors, incorporating mobilization of local groups; collaborative partnerships with religious groups and community activists; and commitment to tackling the problem at the highest political level.
Rates of teenage pregnancy in the United States fell by 30% during the 1990s. Some studies have suggested that the decline resulted from increased uptake of abstinence and increased use of reliable methods of contraception. But other studies also provide evidence that the explanation may lie in changes in economic factors, notably the welfare reforms introduced by the Clinton administration. A number of factors influence adolescents’ motivation to prevent pregnancy, and no one approach satisfactorily accounts for the decline that has occurred so far.
Conclusion
Sexuality is an essential part of human nature, and its expression needs to be affirmed rather than denied, if public health messages are to be heeded. No general public health approach will work everywhere and, by the same token, no single-component intervention is likely to work anywhere. The evidence is that the interventions that work best are complex, multilevel, multipartner behavioral interventions that take account of the social context in mounting individual-level programs; attempt to modify social norms to facilitate uptake and support maintenance of behavior change; and tackle the structural factors contributing to risky sexual behavior. Public health strategies limited to voluntary individual behavior change are unlikely to achieve such radical change without sociostructural changes. The mix of components in national programs needs to be tailored to the local context. The emphasis must be not merely on which approaches work, but on why and how they do so in particular social contexts.
Bibliography:
- American Psychiatric Association (1980) Diagnostic and Statistical Manual of Mental Disorders. 3rd edn. Washington, DC: American Psychiatric Press.
- American Psychiatric Association (2000) Diagnostic and Statistical Manual of Mental Disorders. 4th edn. Washington, DC: American Psychiatric Press.
- Balon R, Segraves RT, and Clayton A (2007) Issues for DSM-V: Sexual dysfunction, disorder, or variation along normal distribution: Toward rethinking DSM criteria of sexual dysfunctions. American Journal of Psychiatry 164: 198–200.
- Bertrand JT, O’Reilly K, Denison J, Anhang R, and Sweat M (2006) Systematic review of the effectiveness of mass communication programs to change HIV/AIDS-related behaviors in developing countries. Health Education Research 21(4): 567–597.
- Clark S (2004) Early marriage and HIV risks in sub-Saharan Africa. Studies in Family Planning 35: 149–160.
- Ezzati M, Vander Hoorn S, and Rodgers A (2003) Estimates of global and regional potential health gains from reducing multiple major risk factors. Lancet 362: 271–280.
- Garcia-Moreno C, Jansen HA, Ellsberg M, Herse L, and Watts C (2005) WHO Multi-Country Study on Women’s Health and Domestic Violence Against Women. Geneva, Switzerland: World Health Organization.
- Graziottin A (2007) Prevalence and evaluation of sexual health problems: HSDD in Europe. Journal of Sexual Medicine 4(supplement 3): 211–219.
- Kretzschmar M and Morris M (1996) Measures of concurrency in networks and the spread of infectious disease. Mathematical Biosciences 133: 165–195.
- Laumann EO, Paik A, and Posen RC (1999) Sexual dysfunction in the United States: Prevalence and predictors. Journal of the American Medical Association 281: 237–244.
- McIntyre JA (2005) Sex, pregnancy, hormones, and HIV. Lancet 366: 1141–1142.
- Miller AM and Vance CS (2004) Sexuality, human rights, and health. Health and Human Rights 7: 5–16.
- Nelson KE, Celentano DD, Eiumtrakol S, et al. (1996) Changes in sexual behavior and a decline in HIV infection among young men in Thailand. New England Journal of Medicine 335: 297–303.
- Parkhurst JO (2002) The Ugandan success story? Evidence and claims of HIV-1 prevention. Lancet 360(9326): 78–80.
- Rotheram-Borus MJ, Cantwell S, and Newman PA (2000) HIV prevention programs with heterosexuals. AIDS 14(Supplement 2): S59–S67.
- Santelli JS, Lindberg LD, Singh S, and Finer LB (2007) Recent declines in adolescent pregnancy in the United States: more abstinence or better contraceptive use? American Journal of Public Health 97(1): 150–156.
- UNAIDS and World Health Organization (2007) AIDS Epidemic Update: December 2007. Geneva, Switzerland: UNAIDS. http://data.unaids.org/pub/EPISlides/2007/2007_epiupdate_en.pdf (accessed February 2008).
- Wellings K, Collumbien M, Slaymaker E, et al. (2006) Sexual behaviour in context: a global perspective. Lancet 368: 1706–1728.
- World Health Organization (1992) ICD–10: International Statistical Classification of Diseases and Related Health Problems, 10th edn. Geneva, Switzerland: World Health Organization.
- World Health Organization (2006) Defining Sexual Health: Report of a Technical Consultation on Sexual Health, 28–31 January 2002, Geneva. Geneva, Switzerland: WHO. http://www.who.int/ reproductive-health/publications/sexualhealth/index.html (accessed February 2008).
- Bancroft J, Graham CA, and McCord C (2001) Conceptualizing sexual problems in women. Journal of Sex and Marital Therapy 27: 95–103.
- Coates TJ, Aggleton P, Gutzwiller F, et al. (1996) HIV prevention in developed countries. Lancet 348: 1143–1148.
- Fathalla MF, Sinding SW, Rosenfield A, and Fathalla MM (2006) Sexual and reproductive health for all: A call for action. Lancet 368: 2095–2100.
- Glasier A, Gu¨ lmezoglu AM, Schmid GP, Garcia Moreno CG, and VanLook PFA (2006) Sexual and reproductive health: A matter of life and death. Lancet 368: 1595–1607.
- Graham CA and Bancroft J (2007) The sexual dysfunctions. In: Gelder M, Lopez-Ibor J, Andreasen N and Geddes J (eds.) New Oxford Textbook of Psychiatry, 2nd edn. Oxford, UK: Oxford University Press.
- Marston C and King E (2006) Factors that shape young people’s sexual behaviour: A systematic review. Lancet 368: 1581–1586.
- Parker RG, Easton D, and Klein CH (2000) Structural barriers and facilitators in HIV prevention: A review of international research. AIDS 14: S22–S32.
- Tiefer L (1996) The medicalization of sexuality: Conceptual, normative, and professional issues. Annual Review of Sex Research 7: 252–282.
- UN Millennium Project (2006) Public Choices, Private Decisions: Sexual and Reproductive Health and the Millennium Development Goals. Geneva, Switzerland: United Nations Development Programmehttp://www.unmillenniumproject.org/reports/srh_main. htm
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








