This sample Social Gradients and Child Health Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Recognition of the social origins of illness dates back hundreds if not thousands of years (Antonovsky, 1967). The literature on the relationship between poverty and ill health began with the inauguration of regular censuses of populations almost two centuries ago (Starfield, 1975). That social factors have an influence on an otherwise biological phenomenon is a fact. Why is it so?
Systematic study of this subject began in earnest well over 100 years ago. Originally, studies focused primarily on the impact of social factors on the most disadvantaged segment of the population: the poor. Most of the early explorations of societal influences focused on the role of the environment (Etches et al., 2006), consistent with the focus of early observations of noxious elements in the environment and the potential provided by censuses to detect geographical pockets of disadvantaged. Observers also recognized that working conditions compromised the health of the working class. However, by the end of the nineteenth century, recognition of germs as the cause of infections in the population raised the possibility of controlling illness with medical rather than environmental or social means. By the 1920s, poverty as an antecedent of disease had ceased to be a focus of attention as concern shifted to the biological and technological aspects of health and health services. Attention to poverty as a correlate of disease greatly diminished in first half of the twentieth century literature. Social conscience was briefly reborn in the 1960s; since then, increasing availability of data and international interest in the health of nations has solidified concern about social origins of illness and their relationship to people’s health (Starfield, 1984). It is quite evident that, even now, virtually every common health condition in childhood (with the exception of myopia, allergies, and some cancers) is more common in poor children than in nonpoor children.
Most research on the social and societal roots of health and illness continues to be descriptive rather than analytic. Many studies have attempted to examine the role of a few characteristics both those of individuals and those of the society in which individuals live that might explain why poverty is highly associated with ill health, but the studies are hampered by two realities: an inadequate conceptualization of pathways to inform development of research design and the fact that extreme social disadvantage entails extreme disadvantage in virtually every characteristic that might be related to ill health. Thus, it is difficult if not impossible to ascertain the relative importance of various influences on health, when they all are so highly interrelated and, therefore, co-occur. Moreover, eliminating poverty alone will not eliminate the adverse impact of social disadvantage on health because other aspects of social position and other societal features also influence the distribution of health in populations (Pruss-Ustun et al., 2004).
It is only relatively recently that research has turned to the concept of the social gradient, wherein health is progressively worse the greater the social disadvantage and progressively better the greater the social advantage. A major stimulant to this reorientation of the issue of social origins of disease was the series of studies by Marmot and colleagues of civil servants in the United Kingdom. These studies conclusively documented a striking gradient in health in adults, even among white-collar employees (Marmot et al., 1987, 1991).
The situation with regard to children has followed the adult pattern: first attention to the very socially disadvantaged and subsequently to social gradients. The impact of social conditions on child health was explicitly recognized at least by the middle of the nineteenth century, when Engels documented the higher death rates from smallpox, measles, scarlet fever, and whooping cough among the working class as compared to upper class children. He even linked the likelihood of childhood falls, drowning, and burns to inadequate child care in families where both mother and father had to work, thus laying the groundwork for study of mechanisms by which social disadvantage produces poorer health (Engels, 1845). But as with adults, the biologically oriented technological imperative has been commanding the greatest attention ever since the end of the 1800s, with brief interruptions as noted for adults.
Despite the tremendous scientific advances underlying medical care in the last half of the twentieth century, which were associated with greatly improved health indicators, there are still large differences in health across different social groups of children. The literature is extensive in attempting to relate this gap to various individual, community, and societal characteristics (IOM, 2004). Only recently has it been noticed that even industrialized countries differ considerably in the health of their children, and that these differences can be explained by historical and societal differences in attitudes toward the health and welfare of children.
What Is Known About The Existence And Nature Of Social Gradients In Children
Research on social gradients, if designed well, has the potential to help understand the mechanisms by which social disadvantage operates to compromise health. In contrast to studies concerning the poor, who suffer virtually every increase in risk and decrease in resilience, studies of social gradients promise to provide more nuance in the search for explanations of health disadvantage as a result of differences in various influences on health.
One of the early studies on social gradients in childhood (Wise et al., 1985) found a progressive increase in mortality with decrease in family income in 10to 14-year-olds and, to a lesser degree, in 15to 19-yearolds. Studies have consistently found social gradients in infancy, in England (West, 1988) and in England and Wales (Pattenden et al., 1999). Dutton (1985) found differences in the results of clinical examinations in African-American children of ages 6 months to 11 years living in one city (Washington, DC). There were social class differences for all three clinical conditions: Hearing loss, ear disease, and vision problems, but there was no gradient because the relationships were U-shaped, with higher prevalence in the lowest and highest income groups. A history of past illnesses of these types had the highest relationship to abnormal clinical findings, even higher than that of family income. Ostberg (1992) reported increasingly clear social class gradients in likelihood of death in Swedish children as age group increased from 1–4 years to 5–9 years, to 10–14 years, and to 15–19 years. A series of studies by Patrick West and colleagues in Scotland led to the conclusion that there was no social class gradient in mortality in adolescence, which they attributed to the ‘‘homogenizing effects of experiences in school, with peers, and pervasive youth culture’’ (West, 1988; West et al., 1990). As mortality in adolescence is predominantly associated with injuries, his conclusions are largely influenced by environmental and social situations that predispose to injury. Williams and colleagues (1997) reported that although there were no social gradients for overall rates of medically attended injuries in Scotland, there were marked differences in where the injuries occurred and the activity associated with the injury. Faelker and colleagues (2000), reporting on data from the Kingston area of Canada, found strong gradients in injuries of certain types (but not of other types). Others have shown gradients in injury mortality among 10 to 14-year-olds and to a lesser degree among 15to 19-year-olds: Avery and colleagues (1990) in England and Wales, and Carey and colleagues (1993) in Australia (New South Wales).
Studies concerning outcomes other than those related to injuries have been relatively consistent in showing social class gradients for:
- Height in Dutch children of ages 5, 7, 11, 14 (Jansen and Hazebroek-Kampschreur, 1997), which were reported to be similar to findings of an earlier study in the Netherlands and in the UK;
- Ratio of weight to height, with more obesity in the lower classes (Jansen and Hazebroek-Kampschreur, 1997), reported to be consistent with studies in France and Stockholm;
- Greater persistence of height deficits in children of low birth weight among lower class children in Britain (Teranishi et al., 2001);
- Psychosocial difficulties (but not mental health status, accident rates, or blood pressure) in youth of ages 13–15 in England (DoH, 1999);
- Activity limitation and long-standing illness in children of ages 10–16 in Britain (Cooper et al., 1998);
- Depression and obesity (but not asthma or sexually transmitted diseases) in U.S. teens (Goodman, 1999);
- Self-reported illness (by parental report) in U.S. adolescents (Call and Nonnemaker, 1999);
- Self-rated physical and psychological health (although not reaching statistical significance) in 16-year-old Australians (Siahpush and Singh, 2000);
- Chronic conditions (and less or insignificantly so, short stature, and incidence of moderate to severe symptoms) in children of ages 2–17 in five Nordic countries (Halldorsson et al., 2000);
- All-cause mortality in U.S. children of ages 0–19 from 1968 to 1992 (DiLiberti, 2000).
More recent studies (published from 2001 through 2006), from a wide variety of countries (Canada, Denmark, New Zealand, Nordic, the United States, UK/Britain, and several European countries), have continued to provide evidence of the existence of social gradients in health. All four studies that addressed injuries are consistent in showing gradients (although varying by type of injury and locale of the study) (Chen et al., 2002; Laflamme and Engstrom, 2002; West and Sweeting, 2004; Emerson et al., 2006).
All seven studies that examined the prevalence of chronic conditions (most but not all by proxy reports of parents) confirmed the social gradient in health, although not always for every condition (Case et al., 2002; Heaney et al., 2002; Saxena et al., 2002; Starfield et al., 2002a; Due et al., 2003; West and Sweeting, 2004; Emerson et al. 2006). Two studies that used vital statistics (infant mortality, low birth weight, under-5 mortality, cause specific mortality) confirmed the existence of social gradients (Martens and Derksen, 2002; Blakely et al., 2003). All five studies using only self-reported overall health found gradients, but not always statistically significant ones, across successively disadvantaged children (Chen et al., 2002; Starfield et al., 2002a, 2002b; Newacheck et al., 2003; West and Sweeting, 2004; Ravens-Sieberer et al., 2005; Emerson et al., 2006). The only measure of health that has not revealed a pattern of social gradients is reported acute symptoms; at least two studies (Due et al., 2003; West and Sweeting, 2004) failed to find any relationships.
Newer studies are increasingly using conceptualizations of ill health that were not used in the past. Development of multidomain health status instruments that tap a wide range of self-reported aspects of health are making it possible to capture a broad view of health and its relationships with social position and other characteristics. One instrument (KIDSCREEN) was recently validated in several European countries. It elicits information from children of ages 8–18, usually in school, in ten domains (physical well-being, psychological well-being, moods and emotions, self-perceptions, autonomy, parent relations and home life, social support and peers, school environment, social acceptance and bullying, and financial resources) (Ravens-Sieberer et al., 2005). Its full potential has yet to be realized, and it is possible that it could be used to develop profiles of health to characterize children according to their pattern of health experiences. A prototype of such an effort is the CHIP (Child Health and Illness Profile). Developed in the United States as a suite of instruments (for self-administration by adolescents, self-administration by children, self-administration by parents, as well as interviewer-administered versions), it provides separate domain and subdomain scores as well as profiles of individuals and, by aggregation, to distinct groups of individuals (Riley et al., 1998a, 1998b).
Using the CHIP, the relationship between social position (a composite of parental education and job status) and health (divided into six domains) was explored by means of questionnaires self-administered by parents for children under age 12 and separately by children of ages 6–10 and 11–17. Additional information was available for 14 subdomains (from parent reports for the younger children and from self-reports by adolescents). Table 1 presents the domains and subdomains. Data were obtained in schools from children and by self-administration at home from parents in several rural and urban areas of the United States.
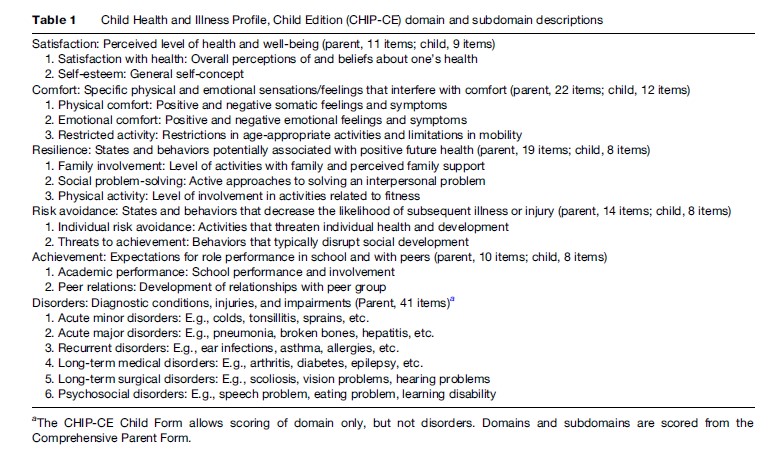
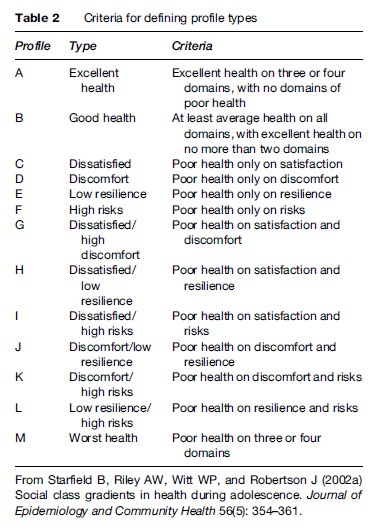
The results confirmed the presence of gradients across three social class groups, but the pattern of significance of the differences varied by domain, generally being less or absent for the domains and subdomains involving symptoms and risky behaviors, and strong for domains and subdomains involving overall satisfaction with health, physical activity, family involvement, and major acute illnesses, as well as long-term conditions. Thirteen profiles of health were constructed by trichotomizing scores on each of the domains (Table 2). Social class gradients in the profiles were present for the adolescents, for the parent reports of the children, and for the children themselves. Most noteworthy was a consistent gradient such that there were progressively more children in the poor profile type with lower social position and progressively more children in the good–excellent profile type with higher social position (Starfield et al., 2002a, 2002b).
The pattern of social gradients was the same both for the younger children and the adolescents, but they were clearer and more likely to be statistically significant for the adolescents, suggesting that the manifestations of social disadvantage increase as children are exposed to it longer. This interpretation is supported by the results of a substudy of 10to 11-year-olds, which showed stronger gradients in the various domains than was the case for younger children responding to the same questionnaire (Starfield et al., 2002b). Stronger gradients in health at older childhood ages was also found by Ostberg (1992), who reported increasingly clear gradients in likelihood of death of Swedish children as age group increased from 1–4 years to 5–9 years, to 10–14 years, and to 15–19 years. Thus, it is likely that the effects of social disadvantage accumulate over time.
The utility of the information obtained by the profile method was provided by a subsequent study that examined the ability of the information on health status to predict subsequent use of health services. The child reports of health were even better predictors of the number of doctor visits in the subsequent year than was the case for parent reports (Forrest et al., 2004). Fortunately, the recent development and growth of the health outcomes strategy, directed in part at assessing the quality, adequacy, and equity of health throughout the world (as represented, for children, by the multicounty collaborative KIDSCREEN instrument) could be an important development, at least with regard to country comparisons of social gradients in childhood.
The potential for wider use of profiles of health is large. As the review of prior studies shows, gradients vary with the measure of health, with age, and with place. Abnormalities in one or more aspects of health provide no information on the total burden of ill health suffered by individuals, and particularly on the burden suffered by individuals in particular social groups. Profiles of health, in contrast, combine information on various aspects of health into a single measure that characterizes individuals and groups according to their total morbidity burden, a useful characterization for monitoring the impact of health services over time, for making needed changes, and for evaluating the effectiveness and equity of these changes over time and across regions and countries.
The Relative Impact Of Prior Child Health And Social Class On Subsequent Health
The existence of social gradients in child health has a large impact on the well-being and resilience of children evidence of the relationship between physical and emotional health. The review did not consider, however, whether the constancy of illness over time was related to social disadvantage associated with ill health in groups of children. themselves. They play a major role in influencing the opportunity for children in different social groups to achieve their inherent potential, both during child-hood and subsequently in adulthood. Is it the long-term effects of poor health in childhood that account for the accumulation over time of subsequent poor health, or is the tracking of poor health a result of the persistence of low social class status over time? Although large-scale longitudinal studies addressing these issues are uncommon (with the exception of the British national birth cohorts), the recent literature is increasingly focusing on these two phenomena.
An early review (Starfield and Pless, 1980) of the extent of persistence of physical health problems (excluding those that are, by nature, persistent, e.g., congenital abnormalities) concluded that, although illness in childhood certainly does not invariably predict poor health in adulthood, people who have an illness in childhood are much more likely to have recurrences of that illness or other illnesses later on. The evidence derives from a variety of types of studies: Studies of the natural history of specific acute illnesses, studies of use of health services over time, studies of overall physical functioning, and evidence of the relationship between physical and emotional health. The review did not consider, however, whether the constancy of illness over time was related to social disadvantage associated with ill health in groups of children.
In Britain, studies using longitudinal data (Holland et al., 2000) showed that children of different heights during childhood have different subsequent experiences. Children who are tall for their age have less exposure to a variety of environmental hazards if they are males with fathers in manual occupations or females with fathers in nonmanual occupations. Chronic disease in childhood was also associated with subsequent greater hazard exposure in males with fathers in manual occupations, but females with chronic disease were less exposed to health hazards if they had fathers in nonmanual occupations. The authors interpreted these findings as evidence that
exposure to health-damaging environments during adulthood may accumulate on top of health disadvantage during childhood and that this process of life-course accumulation of disadvantage may vary by gender and childhood social class. (Holland et al., 2000: 1285)
In the United States, Blackwell and colleagues (2001) used the U.S. Health and Retirement Survey (HRS) to relate adult health to people’s recall of childhood health experiences. They showed that self-reported poor childhood health was associated with increased morbidity in later life. Their findings also indicated that both poor childhood health and current social disadvantage (in adulthood) were independently associated with poor health. In this study, social position was represented by a continuous scale for purposes of regression analysis, so that the relationship between specific characteristics of social classes could not be estimated.
In their review of life-course development of unequal health, Power and Kuh (2006) found evidence of compounding effects of antecedent ill health and current (adult) social disadvantage. That is, early ill health and social disadvantage are both important, and the ill effects of adult low social position are made even more serious by ill health in childhood.
For cardiovascular heart disease (the major cause of death in industrialized countries), early childhood social disadvantage is a highly influential risk, and the effect is cumulative: The longer the social disadvantage, the higher the risk. This increase in risk for heart disease is greater than that for self-reported poor physical or mental health. Moreover, the nature of the increased risk is different for males than for females, at least partly because a large part of the effect of early social disadvantage is its risk for later social disadvantage; females are more likely to stay lower class than are males (Singh-Manoux et al., 2004). Thus, the importance of social gradients in childhood is not only of importance for children but is of more generalizable importance to the health of societies.
There is also evidence for possible pathways that include the impact of prior ill health. For example, adverse effects of prior ill health may operate through effects on maternal ill health and poor nutrition. Moreover, the relationship between poor maternal health on newborn birth weight is intergenerational (Hackman et al., 1983; Klebanoff et al., 1991; Starfield et al., 1991), and the risks are even greater for poor women (Starfield et al., 1991). As low-birth-weight infants are at much greater risk of poor health, it is clear that intergenerational disadvantage creates a vicious circle in which poor health leads to poor health of offspring, leading to poor health in the next generation.
A variety of analyses have indicated that specific patterns of ill health in adulthood are associated with specific patterns of ill health early in childhood. Early influences are of two types: Those related to growth and development and those related to infections early in life. Problems with growth and development, as manifested by intrauterine growth retardation (Starfield et al., 1982) and nutritional short stature in childhood (Case and Paxson, 2006), are associated with higher likelihood of coronary artery disease later in life (Galobardes et al., 2004). Those related to infections and their sequelae, such as from poor access to adequate health services (Starfield, 1985), are often subsequently manifested in chronic respiratory disease, rheumatic heart disease, gastric cancer, hemorrhagic stroke, and hypertension. Interactions of a variety of socioeconomic characteristics and other social determinants have been found for almost all common diseases, with the exception of many types of cancer (Galobardes et al., 2004; Lynch and Davey Smith, 2005). The fact that these associations are not invariable indicates that there are likely to be many other intervening influences, including those that are specifically related to social class as well as a myriad of other social and environmental exposures. Although some of these influences have been described, the pathways through which they operate and interact have not been explored yet.
Characteristic of the growing literature on the influences of prior ill health on subsequent health is the difficulty in sorting out pathways through which early disadvantage (in the form of both health gradients and social gradients) predisposes to later ill health and the relative influence of each. Although it is clear that there are both biological and social mechanisms that are intermediate in the pathway between early health and subsequent health, how they interact and how they are influenced by social position is very poorly understood. Most of the literature on life-course influences has not been designed to examine these influences across the social gradient, focusing instead on comparing life course experiences of the poor versus the nonpoor.
Interactions among influences play a major role in pathways to ill health. It is even likely that pathways differ in different areas and across the social gradient. For example, insulin resistance (which is associated with subsequent diabetes) in children is inversely related to family income in Denmark, but directly related to family income in Estonia and Portugal. The influence on insulin resistance of parental education (which is related to physical fitness in Denmark but not in Estonia or Portugal) shows the same association: negative in Denmark but positive in Estonia and Portugal. Furthermore, findings for adults are similar to those for children in Denmark, southern Europe, and the United States, but different from children in eastern Europe (Lawlor et al., 2005). Similarly, low birth weight and the nature of infant diets interact to influence the likelihood of subsequent heart disease. Low birth weight followed by subsequent rapid growth confers increased risk for obesity, a risk factor for heart disease. The complexity of the pathway – and the likelihood that it contains interactions leading to different types and magnitudes of effects – is indicated by a recent review showing that larger size in infancy is associated with increased risk of insulin-dependent diabetes, but associated with reduced likelihood of ischemic heart disease in men, but not in women. There were considerable gaps in the evidence, and relationships with many other highly prevalent diseases have not been studied (Fisher et al., 2006).
Across developing and middle-income countries, societal influences on under-5 mortality differ by income quintile. For the richest quintile, the higher the country wealth (gross national product), the lower the under-5 mortality. In contrast, infant mortality in the poorest quintile is lower when public spending on health is higher, when skilled attendants are present at delivery, and by immunization coverage (Houweling et al., 2005). Pathway effects differ in different countries; socioeconomic inequalities in mortality are larger in northern Europe than in southern Europe, possibly due to a varying socioeconomic gradient in risks for ischemic heart disease (Kunst et al., 1998). Neighborhood poverty rates and housing inadequacy increase the rate of very preterm births in African-American households, whereas the fraction of female-headed households is influential for Hispanics, and a low fraction of people employed in professional occupations is influential for white populations, at least in the United States (Reagan and Salisberry, 2005; Barros et al., 2006). Thus, there are marked differences, including different interactions in different social strata, within the pathways to aspects of ill health, depending on the context (Lawlor et al., 2005).
All of these findings on the extent of influences of early exposures on later health are consistent with a more general applicability of pleiotropism, etiologic heterogeneity, and penetrance, which were originally used to explain genetic influences on health. The likelihood that a risk factor will result in disease (penetrance) in the presence of different degrees of social disadvantage depends on a constellation of other factors, both in individuals and in populations. Any given health problem may result from different combinations of risk factors in different individuals and different populations (etiologic heterogeneity). Any given combination of risk factors may result in different health outcomes in different individuals and different populations (pleiotropism). Understanding why social gradients exist and why they may differ at different times and in different places requires a recognition of these phenomena, and attempting to reduce social gradients requires exploration of the impact of a variety of individual, social, and societal factors in each different population.
What can be said of the possibility that further research can shed light on the relative mutability of these effects and the possibility for interventions to reduce their impact? If there are no magic bullets (Power and Kuh, 2006), what might be the range of artillery? Answering these questions requires consideration of pathways to ill health in different populations.
What Are The Pathways By Which Social Gradients Influence Health?
The pathways by which different degrees of social disadvantage operate to compromise health are poorly understood, although theories abound. A systematic national effort took place in the United Kingdom in the early 1980s (Black, 1980), which categorized the hypotheses into those related to deprivation of conditions of living necessary to maintain health, including (but not necessarily limited to) adequate food, housing, clothing, neighborhood security, and safety (including quality of the physical environment), and access to high-quality medical care.
Recognition of the existence of a problem is a necessary first step, but it is not sufficient to solve it. Hierarchies of social position have always been a feature of human society, but hierarchies are not invariably associated with marked differences in people’s opportunities to lead fulfilling lives. As health is a major facilitator of a good life, it is a matter of social justice to find ways to reduce the adverse effects on health of social hierarchies.
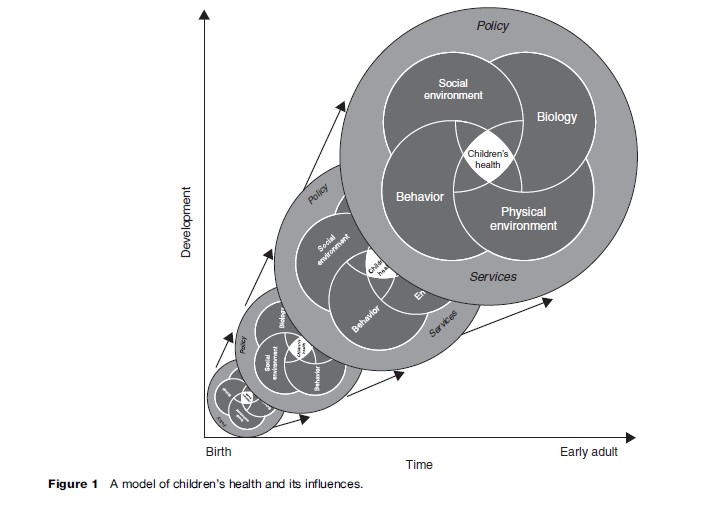
Attempts to elucidate pathways of influence have, so far, been elusive and limited to conceptual schemata that outline the major components in the pathways to ill health. Most of the evidence comes from studies in which populations are divided into poor and nonpoor. A committee of the Institute of Medicine, National Academy of Sciences (United States) devised a kaleidoscopic model specifically for children (IOM, 2004). The diagram (Figure 1) recognizes health as a trajectory over time, with health a product of the interaction of biological characteristics, the physical environment, behavioral characteristics, and the social environment, all operating in a services and policy context. In the publication presenting this conceptualization, the relationships between these types of characteristics and contexts and child health are discussed one by one, mainly in order to set the stage for development of information systems that would capture data to design appropriate policies and programs to overcome vulnerabilities and promote resiliencies.
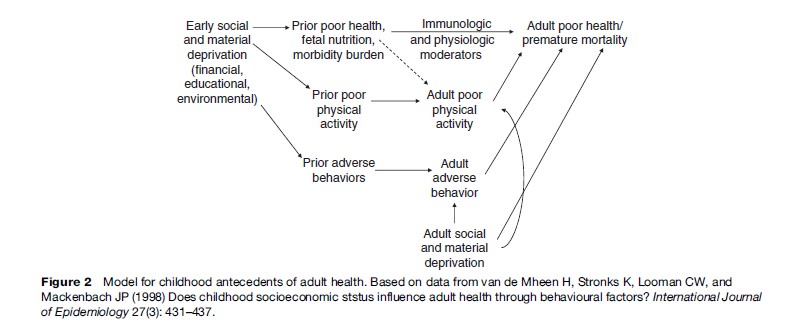
Van de Mheen et al. (1998) examined the relative influence of early childhood social class (based on father’s occupation) on adult health behaviors and self-perceived health (Figure 2). The pathway to health starts with early social and material deprivation (financial, educational, environmental) predisposing to poor health very early in life (as in fetal malnutrition), inadequate physical activity, and adverse behaviors, which, in turn, predispose to immunologic and physiologic deficits, continuing inadequate physical activity, and adverse behaviors, which, in turn (in addition to the direct effects of childhood social and material deprivation), predispose to poor health and premature mortality. Their study included only information on early childhood social class and adult behaviors and reported health status, so that the childhood behaviors can only be presumed. Given this limitation (as well as other methodologic limitations), their data showed that approximately 10% of the differences in adult health are independently attributable to early childhood social class.
Lynch and Kaplan (2000) devised a similar life-course diagram to depict the influence of socioeconomic position at various stages in life. At the very earliest stages of life, socioeconomic position operates by influencing intrauterine conditions leading to low birth weight and growth retardation, which in turn predispose to atherosclerosis (and thus cardiovascular disease and reduced function) later in life. During childhood, socioeconomic position operates primarily through educational and environmental conditions to influence behaviors such as smoking, poor diet, and inadequate physical activity, predisposing to later development of atherosclerosis and cardiovascular disease. In adulthood, socioeconomic position operates through working conditions and income to influence job-related stress predisposing to cardiovascular disease. In later life, income and assets are influenced by socioeconomic position and, with the contribution of inadequate medical care, to reduced function. This formulation depicts the likely influence of poor health, compounded over time by failures to address the adverse effects of prior poor health in childhood, but only low birth weight and growth retardation and not the accumulation of ill health over childhood are recognized.
Power and Kuh (2006) formulated a scheme depicting the impact of childhood social position as starting with parental background, leading to infant health, with subsequent trajectories of educational, social, behavioral, and physical and mental health status, all of which are interrelated and combine to influence health, both directly and indirectly (through later material and social circumstances).
The scheme devised by Diderichsen and colleagues (2001) is broader because it includes societal characteristics as major determinants of pathways to health. Starting with the social context and political characteristics of society, they postulated five general pathways, two of which are inherent in the society and three of which are mutable, depending on the nature of particular policies. The policy characteristics are those that increase social stratification (such as tax policies), those that decrease vulnerability (or increase resilience), and those that prevent adverse consequences (such as regulations that improve safety). These policy characteristics, along with social and cultural characteristics, influence social position, specific exposures, and occurrence of disease or injury, which, in turn, create social consequences on health (such as inability to work).
Although research on children’s health (except for infant mortality) has neglected the influence of the political context, the study by Zambon and colleagues (2006) is an exception. This study used the World Health Organization’s Health Behaviours in School-age Children survey (HBSC) to examine the relationship between the political nature of governments (those whose policies are more redistributive (i.e., conservative welfare regimes and social democratic regimes) and those that are not, i.e., laissez-faire (liberal) regimes). The extent of social gradients in self-reported health of teens was less in the former countries than in the latter countries.
Individual Health And Population Health
Most of these diagrams of influence on health (as well as other common diagrams, e.g., Blum, 1981; Starfield, 1984; Evans and Stoddart, 1990; Wilson and Cleary 1995; Marmot 1999) view health as an individual characteristic and influences on health as characteristics pertinent to individuals. That is, they do not represent the likelihood that specific pathways produce different levels and types of health disadvantages in ‘groups’ in the population. Because pathways may differ by social position (consistent with the findings described earlier in this research paper of the different influences of age, gender, and place on specific health characteristics), it is important to think about their influence on population subgroups as well as on individuals.
Newer conceptualizations of influences on health are addressing influences on populations and on population subgroups (Etches et al., 2006). From the point of view of social gradients in populations, it is the population perspective that is useful. For example, a particular influence, e.g., a rare genetic abnormality, on the health of an individual may be very strong, but if it is rare in the population, it will not contribute to social gradients. In contrast, an influence on health that is common in the population, or in certain subgroups of the population, may contribute considerably to social gradients, even if it causes only a small increase in risk in disadvantaged individuals. For example, ethnic fragmentation, skilled delivery attendance, immunization coverage, and public spending on health contribute more heavily to under-5 mortality among the socially disadvantaged than among the socially advantaged (Houweling et al., 2005) because they are more common among the disadvantaged. Similarly, the relationship between income inequalities and cardiovascular risk factors differs for different socioeconomic strata, being stronger in people with lower incomes (Diez-Roux et al., 2000).
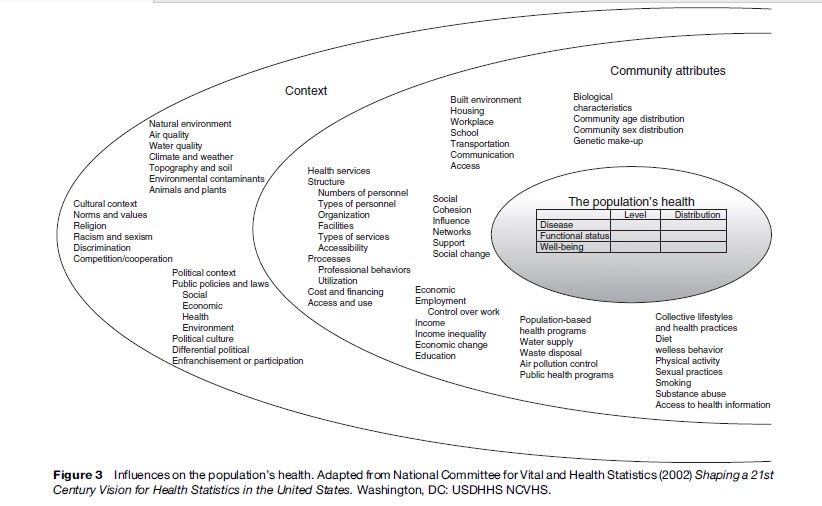
The (U.S.) National Committee on Vital and Health Statistics (2002) devised a model for understanding influences on population health. It divides health into three parts: Rates of disease, functional status, and well-being. Community attributes contribute directly to the health of populations. These community characteristics include demographic composition (e.g., age and sex distribution), the built environment, the social environment, economic characteristics, population health programs, collective lifestyle practices, and health services structures. These community characteristics operate in a context that consists of the natural environment, cultural characteristics, and the political context, all of which are situated in place and time. Figure 3 specifies the different aspects of each of these attributes. As is apparent, the form of the diagram precludes specifying possible pathways and interactions among the attributes and individual aspects of the attributes.
In order to capture the likely major mechanisms that influence social position and, ultimately, health, Starfield (2007) found it necessary to use two diagrams, one representing pathways to the health of individuals and one representing influences on the health of populations (Figures 4 and 5).
These diagrams differ from others in several respects.
- They explicitly represent the likelihood of interactions among influences.
- They reflect the likelihood that different pathways depend on the measure of health (particularly whether the measure reflects incidence or whether it reflects severity as manifested by persistence, or resulting in disability or death).
- The population health diagram includes the distribution of disease as well as overall (average) health, and it gives greater importance to societal influences, i.e., political and policy characteristics.
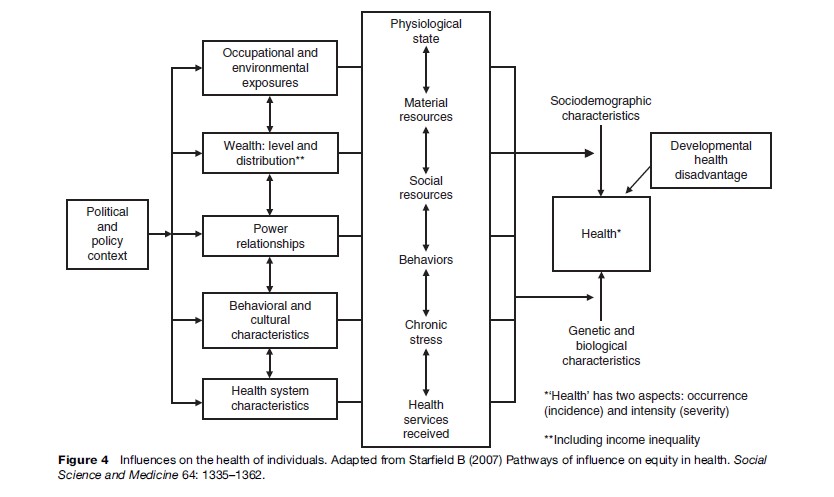
These features make it possible to distinguish influences on the health of individuals (with relative risks and odds ratios depending on different risk factors) from influences on the health of populations and various subgroups (with consideration of the relative frequency of problems and attributable risk). Thus, conceptualizations directed at explaining inequalities in health among individuals and analyzing relative risks of different types of exposures will be different from conceptualizations that are directed at exploring inequities in health across population groups distinguished by social, economic, and geographic characteristics. The utility of the population diagram will be based primarily on knowledge of the relative frequency as well as the strength of the various types of influences on health. For example, the same policy has different effects on health of different racial and ethnic groups in the United States, a result of different frequencies of exposure to various interacting influences (Lipscomb et al., 2006).
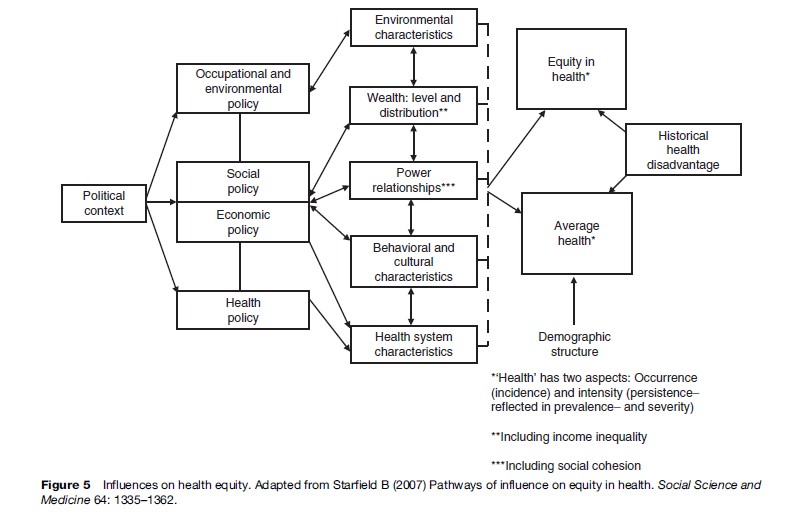
These diagrams are evidence-based in the sense that they derive from existing studies (mostly on poor vs. nonpoor populations rather than on social gradients) that examine each type of influence on at least one aspect of health. In contrast to all other conceptual schemes, these diagrams explicitly recognize that there are many aspects to health, reflecting the reality that the influence of any one type of influence, including social gradients, differs according to the measure of health. In particular, influences differ according to whether the measure of health reflects the occurrence of illness, its persistence over time, its progression to disability, and its case-fatality, i.e., the likelihood of death resulting from it. For example, environmental conditions are most likely to influence the occurrence of illness and its persistence, whereas medical care interventions are more likely to influence the rate of progression of illness and death resulting from the illness. In contrast to many other pathway diagrams, the likelihood of bidirectional and multiple interactions of various types of influences at various levels of effect is explicit. The political and global context is clearly identified in the case of influences on population health and its distribution. In these diagrams, social position is represented differently in the individual and population diagrams. As social gradients is a population characteristic, reflecting the distribution of a characteristic in the population, it appears in the diagram for population health as wealth (level and distribution). It is influenced by a variety of social and economic policies, most notably tax policies, with regard to how regressive or progressive they are. A major challenge for the future is to understand how the relative influence of the various characteristics (including societal as well as individual characteristics) in the pathway differ across the social gradient.
The Role Of Policy
The role of policy in maintaining or reducing social gradients in health is controversial. Based upon observations in some countries that income inequality is associated with worse health, including infant mortality and, especially, rates of homicide and suicide, some have suggested that reduction or elimination of income inequality within societies is indicated (Wilkinson and Pickett, 2006). But the observation that this association is not present everywhere, and is not found for many measures of health, suggests that it is, at best, only a partial explanation. Moreover, there have been no studies that examined the association between income inequality in an area and social gradients in child health; all existing studies have examined only average levels of health in the area or country. Starfield and Birn (2007) explored the possible role of other social policies in influencing the distribution of health in populations. Their analysis concluded that policies that merely redistribute income in the form of money would do little unless services were expanded where they were needed. Moreover, social policies that were universal (rather than targeted toward social deprived populations) were more likely to achieve better health for all (Starfield and Birn, 2007).
In view of the extraordinary complexity of influences on health and on distribution of health in populations, the challenge to develop either a research strategy or a policy strategy to reduce or eliminate social gradients in health is daunting. Fortunately, there are clues as to approaches that would reduce social gradients in health. The fact that pathways to inequity are so variable, often varying by population group, also argues for universality of social programs rather than targeted ones, as the targets would have to be different for every social and demographic group.
As noted above, different aspects of health should be responsive to different influences. Phelan and colleagues showed that there are fewer social gradients for mortality from diseases for which knowledge about preventability and treatment effectiveness exists (Phelan et al., 2004), suggesting that health services, which are generally more available and responsive to individuals of higher social class, play a role in maintaining social class differences. Therefore, health problems that can be prevented or effectively treated by health services interventions are prime (although not sole) targets for health policy. In Finland, social class gradients in deaths from conditions amenable to medical care are greater (at least up to the early 1990s) than those from deaths from other causes, thus indicating a considerable role of inadequate health services in maintaining social gradients in health (Poikolainen and Eskola, 1995). In the last half of the twentieth century, major advances in health services technology have been responsible for large gains in health almost everywhere in the world, although not to the same degree everywhere (Mackenbach, 2005). Gary and Brancati (2005) showed that higher rates of death from diabetes in lower socioeconomic groups are not a result of differences in incidence, thus suggesting a lack of access to health services that could have reduced progression of the illness. Similarly, Maty et al. (2005) found that social position does not predict incidence of diabetes after controlling for overweight and obesity, again suggesting the possibility that poorer access to effective health services early in life is at least partly responsible for poorer prognosis in disadvantaged social groups.
The Role Of Health Services In Reducing Social Gradients
Recent studies provide evidence that countries with health services that are better oriented around primary care (as distinguished from specialty health services) have reduced social class differences in health. For example, in Canada, social class disparities in rates of death from causes amenable to health services have been greatly reduced in the 25 years since the institution of its universal health insurance and orientation to primary care services ( James et al., 2007). Disparities in health are much greater in the United States (which lacks universal financial access to health services and is more oriented to specialty services than to primary care services). A comparison of the prevalence of self-reported major health problems showed that social gradients are less in England (with its universal health system and high primary care orientation) than in the United States for those health problems (diabetes, stroke, lung disease) amenable to health services, particularly primary care services (analyses based on Banks et al., 2006). A summary of existing literature showed that well-organized primary health care reduces disparities in health, particularly for children (Starfield et al., 2005). For example, in the United States, socially deprived areas well-endowed with primary care physicians have 17% lower postneonatal mortality rates, compared with the population mean for those areas, whereas postneonatal mortality rates are 7% higher if primary care resources are poor. The findings are even more striking for levels of self-reported health. The adverse effect of income inequality (reflecting social disadvantage) on all-cause mortality and mortality associated with heart disease and cancer is considerably diminished where primary care resources are adequate. In the United States, the supply of primary care physicians has a larger positive impact on low birth weight and infant mortality in areas with high social inequality than it does in areas with less social inequality. Other studies in the United States had similar findings: Reduced social and racial inequity in health where primary care services are higher (Starfield et al., 2005). Studies in the United Kingdom concerning coronary disease mortality and diabetes reinforce this conclusion (see studies cited in Starfield et al., 2005: 471). Studies in Mexico and in Costa Rica also support the conclusion that primary care reforms reduce social gradients in health with the effect being especially strong in infancy and childhood (as cited in Starfield et al., 2005: 471–473). These findings are confirmed by international comparative studies that show that countries with health systems oriented toward primary care have less marked social gradients than countries with less adequate primary care infrastructures in their health systems (van Doorslaer et al., 2004).
The role played by health services, and especially primary health-care services, in reducing social gradients in health provides a good example of the importance of universal approaches to social welfare. Countries in which policies are based on guaranteed services to the whole population achieve better health than countries that use solutions based on market mechanisms that provide services on demand, with a social safety net to rescue individuals and population groups without power or ability to make demands and purchase services ( Jones et al., 2006).
Future Directions
Future research on social gradients can build on prior research to design more informed and more useful studies by:
- Pre-specifying the likely relative magnitude of various influences and types of influences, based on existing studies, and testing their impact on different social groups in the population.
- Starting with children. Because of their younger age, children have been subjected to fewer influences than have adults, so that finding the most important influences should be easier than is the case in adults.
- Including a variety of types of influences that prior evidence suggests are important. As primary healthcare services have repeatedly been shown to influence at least those aspects of health known to be amenable to health services, it does not make sense to exclude quality of primary care received by people in studies of influences on social gradients.
- Including health outcomes that represent more than one type, i.e., measures of incidence, prevalence, severity, and case fatality, as well as profiles of health.
5.. Examining evidence according to the relative likelihood of the risk leading to a problem (predictive value in different populations as well as the extent to which the risk has a large influence in populations (attributable risk in different populations).
- Stratifying populations into major subpopulations, including a variety of competing hypotheses, and testing for interactions as well as main effects of influences.
7.. Examining strength of relationships; where relationships are weak or variable across individuals or populations, considering the possibility that other (unmeasured) characteristics are involved.
- Using longitudinal study designs to test long-term as well as short-term influences.
- Carefully considering the most appropriate measure of social position. Although the extent to which different types of measures, e.g., income, occupation, education, accumulated wealth, have different associations with health is beyond the scope of this research paper, each has a different pattern of relationship in the pathway to ill health.
Armed with existing and new knowledge, policy makers can make more informed decisions about approaches to reducing and, ultimately eliminating social gradients, which compromise the health of children and the adults they will become and that, ultimately, will influence the success of a society in achieving a better life for all.
Bibliography:
- Antonovsky A (1967) Social class, life expectancy and overall mortality. Milbank Memorial Fund Quarterly 45(2): 31–73.
- Avery JG, Vaudin JN, Fletcher JL, and Watson JM (1990) Geographical and social variations in mortality due to childhood accidents in England and Wales 1975–1984. Public Health 104(3): 171–182.
- Banks J, Marmot M, Oldfield Z, and Smith JP (2006) Disease and disadvantage in the United States and in England. Journal of the American Medical Association 295(17): 2037–2045.
- Barros AJD, Victora CG, Horta BL, et al. (2006) Effects of socioeconomic change from birth to early adulthood on height and overweight. International Journal of Epidemiology 35: 1233–1238.
- Black D (1980) Inequalities in Health: Report of a Research Working Group. London: Department of Health and Social Security.
- Blackwell DL, Hayward MD, and Crimmins EM (2001) Does childhood health affect chronic morbidity in later life? Social Sciences and Medicine 52(8): 1269–1284.
- Blakely T, Atkinson J, Kiro C, Blaiklock A, and D’Souza A (2003) Child mortality, socioeconomic position, and one-parent families: Independent associations and variation by age and cause of death. International Journal of Epidemiology 32(3): 410–418.
- Blum HL (1981) Planning for Health. New York: Human Sciences Press.
- Call KT and Nonnemaker J (1999) Socioeconomic disparities in adolescent health: Contributing factors. Annals of the New York Academy of Sciences 896: 352–355.
- Carey V, Vimpani G, and Taylor R (1993) Childhood injury mortality in New South Wales: Geographical and socio-economic variations. Journal of Paediatrics and Child Health 29(2): 136–140.
- Case A and Paxson C (2006) Stature and Status: Height, Ability, and Labor Market Outcomes. Working Paper 12466. Princeton, NJ: National Bureau of Economic Research.
- Case A, Lubotsky D, and Paxson C (2002) Economic status and health in childhood: The origins of the gradient. American Economic Review 92(5): 1308–1334.
- Chen E, Matthews KA, and Boyce WT (2002) Socioeconomic differences in children’s health: How and why do these relationships change with age? Psychology Bulletin 128(2): 295–329.
- Cooper H, Arber S, and Smaje C (1998) Social class or deprivation? Structural factors and children’s limiting longstanding illness in the 1990s. Sociology of Health and Illness 20: 289–311.
- Diderichsen F, Evans T, and Whitehead M (2001) The social basis of disparities in health. In: Evans T, Whitehead M, Diderichsen F, Bhuiya A and Wirth M (eds.) Challenging Inequities in Health: From Ethics to Action, pp. 13–23. New York: Oxford University Press
- Diez-Roux AV, Link BG, and Northridge ME (2000) A multilevel analysis of income inequality and cardiovascular disease risk factors. Social Science and Medicine 50(5): 673–687.
- DiLiberti JH (2000) The relationship between social stratification and all-cause mortality among children in the United States: 1968–1992. Pediatrics 105(1): e2.
- DOH (1999) Health Survey of England: The Health of Young People ’95–’97. London, UK: University College London.
- Due P, Lynch J, Holstein B, and Modvig J (2003) Socioeconomic health inequalities among a nationally representative sample of Danish adolescents: the role of different types of social relations. Journal of Epidemiology and Community Health 57(9): 692–698.
- Dutton DB (1985) Socioeconomic status and children’s health. Medical Care 23(2): 142–156.
- Emerson E, Graham H, and Hatton C (2006) Household income and health status in children and adolescents in Britain. European Journal of Public Health 16(4): 354–360.
- Engels F (1845) The Condition of the Working Class in England. Stanford, CA: Stanford University Press (1958).
- Etches V, Frank J, Ruggiero ED, and Manuel D (2006) Measuring population health: a review of indicators. Annual Review of Public Health 27: 29–55.
- Evans RG and Stoddart GL (1990) Producing health, consuming health care. Social Science and Medicine 31(12): 1347–1363.
- Faelker T, Pickett W, and Brison RJ (2000) Socioeconomic differences in childhood injury: a population based epidemiologic study in Ontario, Canada. Injury Prevention 6(3): 203–208.
- Fisher D, Baird J, Payne L, et al. (2006) Are infant size and growth related to burden of disease in adulthood? A systematic review of literature. International Journal of Epidemiology 35(5): 1196–1210.
- Forrest CB, Riley AW, Vivier PM, Gordon NP, and Starfield B (2004) Predictors of children’s healthcare use: the value of child versus parental perspectives on healthcare needs. Medical Care 42(3): 232–238.
- Galobardes B, Lynch JW, and Davey Smith G (2004) Childhood socioeconomic circumstances and cause-specific mortality in adulthood: systematic review and interpretation. Epidemiology Reviews 26: 7–21.
- Gary TL and Brancati FL (2005) Commentary: socioeconomic position and the risk of type 2 diabetes. International Journal of Epidemiology 34(6): 1282–1283.
- Goodman E (1999) The role of socioeconomic status gradients in explaining differences in US adolescents’ health. American Journal of Public Health 89(10): 1522–1528.
- Hackman E, Emanuel I, van Belle G, and Daling J (1983) Maternal birth weight and subsequent pregnancy outcome. Journal of the American Medical Association 250(15): 2016–2019.
- Halldorsson M, Kunst AE, Kohler L, and Mackenbach JP (2000) Socioeconomic inequalities in the health of children and adolescents: a comparative study of the five Nordic countries. European Journal of Public Health 10(4): 281–288.
- Heaney DC, MacDonald BK, Everitt A, et al. (2002) Socioeconomic variation in incidence of epilepsy: prospective community based study in south east England. British Medical Journal 325(7371): 1013–1016.
- Holland P, Berney L, Blane D, et al. (2000) Life course accumulation of disadvantage: childhood health and hazard exposure during adulthood. Social Science and Medicine 50(9): 1285–1295.
- Houweling TA, Caspar AE, Looman WN, and Mackenbach JP (2005) Determinants of under-5 mortality among the poor and the rich: a cross-national analysis of 43 developing countries. International Journal of Epidemiology 34(6): 1257–1265.
- IOM Committee on Evaluation of Children’s Health (2004) Children’s Health, the Nation’s Wealth: Assessing and Improving Child Health. Washington, DC: National Academies Press.
- James P, Wilkins R, Detsky A, Tugwell P, and Manuel D (2007) Avoidable mortality by neighborhood income in Canada: 25 years after the establishment of universal health insurance. Journal of Epidemiology and Community Health 61: 287–296.
- Jansen W and Hazebroek-Kampschreur AA (1997) Differences in height and weight between children living in neighbourhoods of different socioeconomic status. Acta Pediatrica 86(2): 224–225.
- Jones C, Burstrom B, Marttila A, Canvin K, and Whitehead M (2006) Studying social policy and resilience to adversity in different welfare states: Britain and Sweden. International Journal of Health Services 36(3): 425–442.
- Klebanoff MA, Graubard BI, Kessel SS, and Berendes HW (1984) Low birth weight across generations. Journal of the American Medical Association 252(17): 2423–2427.
- Kunst AE, Groenhof F, and Mackenbach JP, EU Working Group on Socioeconomic Inequalities in Health (1998) Occupational class and cause specific mortality in middle aged men in 11 European countries: comparison of population based studies. British Medical Journal 316(7145): 1636–1642.
- Laflamme L and Engstrom K (2002) Socioeconomic differences in Swedish children and adolescents injured in road traffic incidents: cross sectional study. British Medical Journal 324(7334): 396–397.
- Lawlor DA, Harro M, Wedderkopp N, et al. (2005) Association of socioeconomic position with insulin resistance among children from Denmark, Estonia, and Portugal: cross sectional study. British Medical Journal 331(7510): 183–187.
- Lipscomb HJ, Loomis D, McDonald MA, Argue RA, and Wing S (2006) A conceptual model of work and health disparities in the United States. International Journal of Health Services 36(1): 25–50.
- Lynch J and Davey Smith G (2005) A life course approach to chronic disease epidemiology. Annual Review of Public Health 26: 1–35.
- Lynch J and Kaplan G (2000) Socioeconomic position. In: Berkman L and Kawachi I (eds.) Social Epidemiology. New York: Oxford University Press.
- Mackenbach J (2005) Health Inequalities in Europe. Monograph prepared for the UK Presidency of the European Union.
- Marmot M (1999) Epidemiology of SES and health. In: Adler N, Marmot M, McEwen B and Stewart J (eds.) Socioeconomic Status and Health in Industrialized Nations: Social, Psychological, and Biological Pathways, p. 21. New York: New York Academy of Sciences Press
- Marmot MG, Kogevinas M, and Elston MA (1987) Social/economic status and disease. Annual Review of Public Health 8: 111–135.
- Marmot MG, Davey Smith G, Stansfeld S, et al. (1991) Health inequalities among British civil servants: the Whitehall II study. Lancet 337(8754): 1387–1393.
- Martens P and Derksen S (2002) Improving children’s health. Canadian Journal of Public Health 93(Suppl 2): S21–S26.
- Maty SC, Everson-Rose SA, Haan MN, Raghunathan TE, and Kaplan GA (2005) Education, income, occupation, and the 34-year incidence (1965–99) of type 2 diabetes in the Alameda County Study. International Journal of Epidemiology 34(6): 1274–1281.
- National Committee for Vital Health Statistics (2002) Shaping a 21st Century Vision for Health Statistics in the United States. Washington, DC: USDHHS NCVHS.
- Newacheck PW, Hung YY, Park MJ, Brindis CD, and Irwin CE Jr. (2003) Disparities in adolescent health and health care: does socioeconomic status matter? Health Services Research 38(5): 1235–1252.
- Ostberg V (1992) Social class differences in child mortality, Sweden 1981–1986. Journal of Epidemiology and Community Health 46(5): 480–484.
- Pattenden S, Dolk H, and Vrijheid M (1999) Inequalities in low birth weight: parental social class, area deprivation, and ‘‘lone mother’’ status. Journal of Epidemiology and Community Health 53(6): 355–358.
- Phelan JC, Link BG, Diez-Roux A, Kawachi I, and Levin B (2004) ‘‘Fundamental causes’’ of social inequalities in mortality: a test of the theory. Journal of Health and Social Behavior 45(3): 265–285.
- Poikolainen K and Eskola J (1995) Regional and social class variation in the relative risk of death from amenable causes in the city of Helsinki, 1980–1986. International Journal of Epidemiology 24(1): 114–118.
- Power C and Kuh D (2006) Life course development of unequal health. In: Siegrist J and Marmot M (eds.) Social Inequalities in Health: New Evidence and Policy Implications, pp. 27–53. New York: Oxford University Press
- Pruss-Ustun A, Campbell-Lendrum D, Corvalan C, and Woodward A (2004) Assessing the Distribution of Health Risks by Socioeconomic Position at National and Local Levels. Geneva, Switzerland: World Health Organization.
- Ravens-Sieberer U, Gosch A, Rajmil L, et al. (2005) KIDSCREEN-52 quality-of-life measure for children and adolescents. Expert Reviews of Pharmacoeconomics Research 5(3): 353–364.
- Reagan PB and Salsberry PJ (2005) Race and ethnic differences in determinants of preterm birth in the USA: broadening the social context. Social Science and Medicine 60(10): 2217–2228.
- Riley AW, Forrest CB, Starfield B, et al. (1998a) Reliability and validity of the adolescent health profile-types. Medical Care 36(8): 1237–1248.
- Riley AW, Green BF, Forrest CB, et al. (1998b) A taxonomy of adolescent health: development of the adolescent health profile-types. Medical Care 36(8): 1228–1236.
- Saxena S, Eliahoo J, and Majeed A (2002) Socioeconomic and ethnic group differences in self-reported health status and use of health services by children and young people in England: cross sectional study. British Medical Journal 325(7363): 520.
- Siahpush M and Singh GK (2000) A multivariate analysis of the association between social class of origin and current social class with self-rated general health and psychological health among 16-year-old Australians. Australia and New Zealand Journal of Medicine 30(6): 653–659.
- Singh-Manoux A, Ferrie JE, Chandola T, and Marmot M (2004) Socioeconomic trajectories across the life course and health outcomes in midlife: evidence for the accumulation hypothesis? International Journal of Epidemiology 33(5): 1072–1079.
- Starfield B (1975) Definitions of ill health. Encyclopedia Britannica, Britannica Book of the Year, 1975, pp. 341–344. Chicago, IL: Helen Hemingway Benton Publishers
- Starfield B (1984) Social factors in child health. In: Green M and Haggerty RJ (eds.) Ambulatory Pediatrics III, pp. 12–18. Philadelphia, PA: WB Saunders
- Starfield B (1985) The Effectiveness of Medical Care: Validating Clinical Wisdom. Baltimore, MD: Johns Hopkins University Press.
- Starfield B (2007) Pathways of influence on equity in health. Social Science and Medicine 64: 1335–1362.
- Starfield B and Birn A-E (2007) Income redistribution is not enough: income inequality, social welfare programs, and achieving equity in health. Journal of Epidemiology and Community Health 61: 1038–1041.
- Starfield B and Pless IB (1980) Physical health. In: Brim O and Kagan J (eds.) Constancy and Change in Human Development, pp. 272–324. Cambridge, MA: Harvard University Press
- Starfield B, Shapiro S, McCormick M, and Bross D (1984) Mortality and morbidity in infants with intrauterine growth retardation. Journal of Pediatrics 101(6): 978–983.
- Starfield B, Shapiro S, Weiss J, et al. (1991) Race, family income, and low birth weight. American Journal of Epidemiology 134(10): 1167–1174.
- Starfield B, Riley AW, Witt WP, and Robertson J (2002a) Social class gradients in health during adolescence. Journal of Epidemiology and Community Health 56(5): 354–361.
- Starfield B, Robertson J, and Riley A (2002b) Social class gradients and health in childhood. Ambulatory Pediatrics 2: 238–246.
- Starfield B, Shi L, and Macinko J (2005) Contribution of primary care to health systems and health. Milbank Q 83(3): 457–502.
- Teranishi H, Nakagawa H, and Marmot M (2001) Social class difference in catch up growth in a national British cohort. Archives of Diseases in Childhood 84(3): 218–221.
- van de Mheen H, Stronks K, Looman CW, and Mackenbach JP (1998) Does childhood socioeconomic status influence adult health through behavioural factors? International Journal of Epidemiology 27(3): 431–437.
- van Doorslaer E, Koolman X, and Jones AM (2004) Explaining incomerelated inequalities in doctor utilisation in Europe. Health Economics 13(7): 629–647.
- West P (1988) Inequalities? Social class differentials in health in British youth. Social Science and Medicine 27(4): 291–296.
- West P and Sweeting H (2004) Evidence on equalisation in health in youth from the West of Scotland. Social Science and Medicine 59(1): 13–27. West P, Macintyre S, Annandale E, and Hunt K (1990) Social class and health in youth: findings from the west of Scotland twenty-07 study. Social Science and Medicine 30(6): 665–673.
- Williams JM, Currie CE, Wright P, Elton RA, and Beattie TF (1997) Socioeconomic status and adolescent injuries. Social Science and Medicine 44(12): 1881–1891.
- Wilkinson RG and Pickett KE (2006) Income inequality and population health: A review and explanation of the evidence. Social Science and Medicine 62(7): 1768–1784.
- Wilson IB and Cleary PD (1995) Linking clinical variables with health- related quality of life. A conceptual model of patient outcomes. Journal of the American Medical Association 273(1): 59–65.
- Wise PH, Kotelchuck M, Wilson ML, and Mills M (1985) Racial and socioeconomic disparities in childhood mortality in Boston. New England Journal of Medicine 313(6): 360–366.
- Zambon A, Boyce W, Cois E, et al. (2006) Do welfare regimes mediate the effect of socioeconomic position on health in adolescence? A Cross-national comparison in Europe, North America, and Israel. International Journal of Health Services 36: 309–329.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








