This sample Spinal Injury Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Introduction
Spinal injury can have a devastating impact on an individual and have far-reaching consequences for future health-care and socioeconomic requirements. It is both an acute and a long-term condition that requires not only initial treatment and rehabilitation but also continuing care provision and support for those affected.
Preventative measures may help to reduce the burden of spinal injuries on society, and in some instances there may be a role for legislative procedures to lessen the frequency and severity of the disease.
Nature of Injury
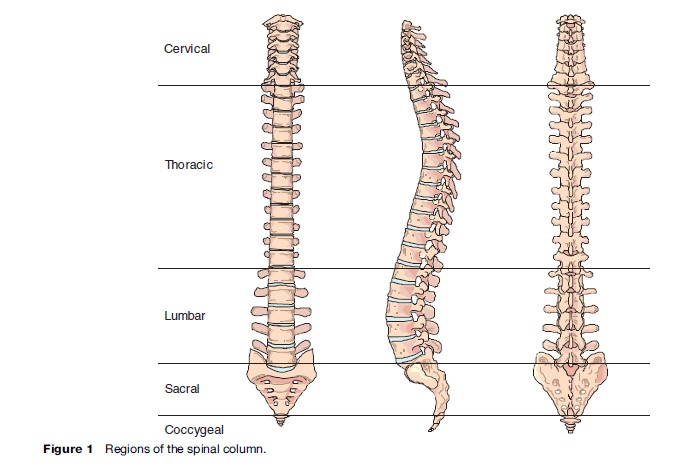
The term spinal injury encompasses many different diseases. To fully understand the differences, it is useful to have a basic understanding of the anatomy of the spinal column. It is made up of 33 vertebrae – 7 cervical, 12 thoracic (dorsal), 5 lumbar, 5 sacral, and 4 coccygeal (Figure 1). Structure and mobility is maintained by longitudinal muscles and spinal ligaments.
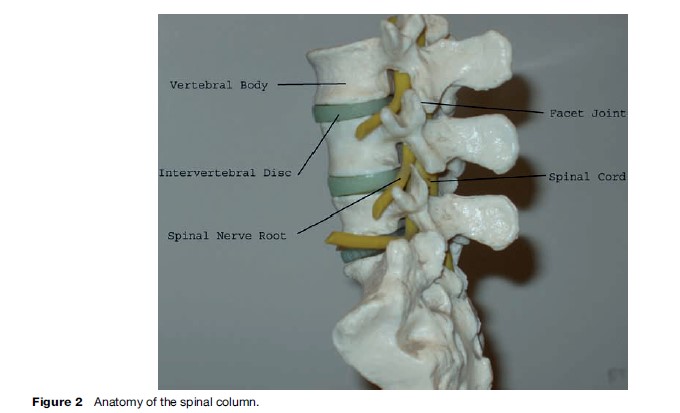
The spinal cord carries impulses to and from the brain via all parts of the body excluding the front of the head and face. At each vertebral level, nerve fibers project from the spinal cord between the vertebrae to skin, muscle, and organs (Figure 2).
Injury may range from minor soft tissue injuries to the supporting ligaments and muscles to complete transection of the spinal column, leading to loss of communication between the brain and those parts of the body innervated by the cord below the level of the injury. In a similar fashion, one must also consider the level of any cord injury, as all areas below the level of injury may be affected.
Epidemiology
Defining the prevalence and incidence of spinal injury is complicated by a number of factors. First, as noted previously, the definition of spinal injury varies from minor soft tissue injury to complete cord injury. Second, published data differ from study group to study group, with many studies looking at preselected populations, such as patients attending trauma centers or those already being screened for potential spinal injury. Third, despite the presence of national registries – for example, the National Spinal Cord Injury Database (NSCI) in the USA and the Trauma Audit Research Network Database (TARN) in the UK, there is a lack of large population-based databases with the ability to identify all trauma presentations in a denominator population.
Previous reports have estimated the worldwide incidence of spinal cord injury as between 15 and 40 cases per million population ( Jackson et al., 2004). In the United States, four times as many men as women sustain spinal cord injury, with a mean age of 33 at presentation ( Jackson et al., 2004). Data from the United Kingdom reflect a similar, though less marked, sex bias with 65% of cases of all spinal injury being seen in men and the presence of spinal injury in the polytrauma patient being greatest in the under-35-year age group (O. Amin, unpublished data).
Spinal cord injury is associated with an increase in mortality for a number of reasons. The mechanism and forces involved in spinal cord injury frequently mean that other major organs are similarly injured. There is a clear relationship between the probability of survival and both the severity and number of injuries in the multiply injured patient. In addition, the direct effects of the injury itself may be fatal. The diaphragm, which is essential for normal breathing, is innervated by the third, fourth, and fifth cervical nerve roots. Injury above these levels is frequently fatal. For those that do survive the initial trauma, there remains a high mortality rate. The 1-year case fatality rate for patients who are admitted to hospital with spinal cord injury is 13% with 11% of all patients dying during the initial hospitalization. When pre-hospital death rates are considered, this rises to 46% (Kraus et al., 1975).
Nervous tissue has very little capability of healing or regeneration. Unlike many other forms of trauma, disability from spinal cord injury is usually permanent. As advances in care and rehabilitation progress, both in the developed and the developing world, the prevalence of spinal injury is set to rise.
Etiology
By far the biggest common single cause of spinal injury is motor vehicle collisions (MVC). The NSCID demonstrates a total of 45.6% of spinal cord injuries occurring due to this mechanism ( Jackson et al., 2004). Other studies have demonstrated a relative risk of spinal cord injury of 1.91 (95% CI 1.73–2.10) for MVC versus all other mechanisms of trauma. This pattern is reflected also in children – 49.8% of all spinal injuries in those aged 16 or under are due to MVC (Martin et al., 2004).
In the developed world, there is an increasing trend for recreational causes of spinal injury, most notably through the use of all-terrain vehicles and in contact sports or in extreme sports activities. In the developing world, industrial injuries and violence remain common causes of injury to the spinal column.
Burden
There are three key areas that spinal injury places a burden upon, namely physical health, emotional and social well-being, and economic stability. These may be considered not only in terms of the needs of the individual but also in terms of the impact upon society as a whole.
Physical Health
The impact on health of spinal injury may be devastating, and chronic health problems may occur with any injury, from minor soft tissue injury through to complete spinal cord injury. Soft tissue injury to the neck following an MVC and its associated symptoms of headache, muscle pain, dizziness, and paresthesia to the hands and arms is referred to by the term ‘whiplash-associated disorder’ or WAD. Although the injuries themselves may be minor and expected to heal quickly, there is an increasing tendency for this to lead to more chronic problems. There is no clear pathological mechanism for this phenomenon, and it is thought by many to be influenced by cultural and psychological factors. Despite this, as many as 50% of patients with WAD report persistent symptoms at 3 months and 25% of patients still have symptoms 2 years after the initial injury (Gargan, 1994; Ferrari, 1999; Melody, 2003).
The majority of spinal cord injury (approximately 55%, rising to 60% in children) occurs at the cervical level due to the excessive mobility that may take place here. Of all spinal cord injuries, 45% are complete – in other words, causing total loss of function and sensation at some level below the injury (Sekhon, 2001).
Probably the most serious associated physical effect from high (i.e., cervical) spinal cord injuries is loss of respiratory function. This may be partial or complete, and may require permanent respiratory support using a ventilator. This will necessitate the presence of an artificial airway, which is usually created by a procedure known as tracheostomy. However, normal speech cannot take place once a tracheostomy is fashioned (although adjuncts do exist which can provided for some degree of communication); there is also an increased risk of infection at both the tracheostomy site and in the lungs themselves.
Complete paralysis of the lower limbs is common in cord injury. As a result, locomotion may be dependent on artificial aids such as wheelchairs. These may need to be motorized, especially when the patient has impairment affecting the upper limbs also. Limitation of movement caused by paralysis leads to other specific complications: pressure sores are more likely to develop, and there is an increased risk of deep venous thrombosis forming in the legs. Where chest muscles are impaired, the ability to clear respiratory secretions is reduced, leading to an increased risk of developing pneumonia.
Disorders of defecation and micturition will occur with nearly all cord injuries. Long-term urinary catheterization may be employed to overcome the latter but may lead to an increased risk of infection, which may give rise to local or systemic illness. This may be overcome by intermittent self-catheterization. Incomplete voiding may lead to stasis of urine and subsequent complications of renal impairment and calculus formation. Fecal voiding may prove difficult due to loss of control over the rectal and anal musculature (Table 1).
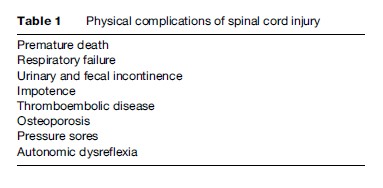
Other problems also frequently seen include impotence (although libido and fertility may be preserved), osteoporosis secondary to immobility, chronic pain syndromes, and autonomic dysreflexia – a ‘resetting’ of some of the body’s homeostatic mechanisms, which may lead to abnormal cardiovascular response to injury. As with all permanent symptoms, these may progress to impact future psychological adaptation to spinal injury.
Emotional and Social Well-Being
The impact of spinal injury on an individual may be devastating. It is a disease with a high prevalence in the young and frequently active and may lead to a lifetime of disability and dependence. As such there are major implications for those injured, their families, and their care-givers.
Psychological difficulties are well recognized in patients with spinal injuries. Both depressive symptoms and major depressive disorders are commonly reported. In some studies, the rate of major depressive disorder is as high as 37.5%. Up to 76.6% of patients may exhibit some depressive symptoms. Other psychological problems, such as post-traumatic stress disorder (PTSD), have also been reported – most notably in those with a violent mechanism of injury or who have witnessed others die in the same incident in which the injury was sustained (Bombardier, 2004).
Return to employment is one important goal in rehabilitation after any major illness or disease. At 1 year postinjury, only 22% of patients report themselves as employed, compared to 58.6% pre-injury. A greater likelihood of return to work is seen in patients who are Caucasian, who are younger age at time of injury, who have had more years of education, and who experienced a less severe injury. The percentage of patients with spinal cord injury who do return to work increases with time from the injury but does not return to pre-injury levels until 5 years after the injury occurred (Krause, 1999).
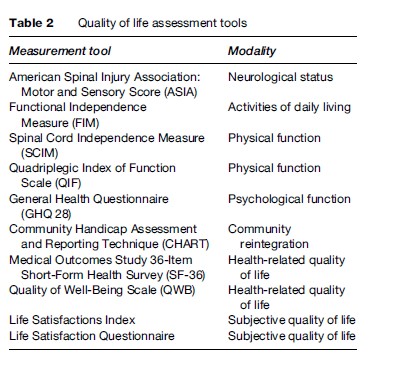
Quality of life (QOL) is defined by the World Health Organization as ‘individuals’ perception of their position in life in the context of the culture and value systems in which they live, and in relation to their goals, expectations, standards and concerns.’ The use of various tools to assess QOL in spinal injury has been studied extensively, but there remains disagreement on how best this is measured. One must also distinguish between physical and psychological function, handicap, health-related quality of life, community reintegration, and subjective quality of life (Table 2).
One might expect that the higher the level of the injury, and thus the greater the disability, the lower the subjective quality of life. However, this does not appear to be borne out by published evidence. Instead, quality of life issues are affected far more by environmental and social issues both before and after the time of the injury. Predictors of better reported quality of life include higher level of education, younger age at time of injury (although QOL improves with time from injury), and Caucasian ethnicity (Whiteneck, 2004). It can be seen that these are the same factors that predict return to work, and both of these findings may reflect societal attitudes as a whole rather than specific advantages in patients with spinal cord injury. Indeed it has been demonstrated that economic and psychosocial factors also have an impact on life expectancy following spinal injury (Krause, 1999).
The impact of spinal cord injury on caregivers should also be considered. Whereas persons with paraplegia may be able to live a relatively independent lifestyle, those with quadriplegia, particularly those with high cervical injuries, may require extensive nursing and social care. This in turn places a burden not only on resources, but also on the psychological and social well-being of the caregiver, who in many cases may be a relative with a previously independent life.
Economic Stability
It may be supposed that minor injury to the spinal column, for example, WAD, places little burden on an economy. However, the impact is extensive – in the United Kingdom alone, an estimated £3 billion (US$5.26 billion) are lost per annum due to this syndrome, principally through insurance claims and loss of earnings.
When one considers cord injury, several other factors come into play, from permanent loss of earnings, to the cost of health care, rehabilitation, and social support. Precise calculations of the cost will vary depending on a number of individual and institutional factors – the precise needs of any particular patient and the ability of an economy to support these needs. For example, in the developing world, the direct provision of long-term social care may not be met by central funding and therefore may not occur at all.
In an analysis of the economic costs of spinal cord injury, Berkowitz et al. (1998) calculated that the annual direct cost to the United States per annum was $9.73 billion. This figure incorporates medical costs and home/transport modifications as well as provision of personal care. Indirect costs, such as those incurred by loss of productivity, are thought to be around $2.6 billion per annum in the United States.
This picture can be expected to change over the next 10–20 years (Lasfargues et al., 1995). Improvement in delivery of immediate medical care has increased the number of patients surviving major trauma. The long-term survival of patients with spinal cord injury is continuing to improve due to advances in medical aftercare. Engineers and designers continue to develop better, though more expensive aids to allow integration into society and improve mobility, such as improved manual and electric wheelchairs and nerve stimulators to allow performance of basic functions. In the developing world, health-care systems are improving, leaving increasing demands on social care for survivors.
Implications
The implications for the public health physician in considering spinal injury reflect the rarity but severity of the disease. Although not a major cause of morbidity or mortality, spinal injury places a large burden on healthcare economies. Measures to reduce this burden should focus on prevention, where there are numerous avenues that can be explored, and the role of the public health physician is paramount.
Given that by far the largest single mechanism of injury to the spinal column is motor vehicle collision, the primary focus on prevention should focus on road safety measures. There is a clear relationship between speed of impact and severity of injury, which may be reduced by traffic-calming measures, such as reduced speed limits in built-up areas, speed bumps, safety cameras, and improvements in road design. An active role from those with an interest in road safety has led to an improvement in car design to allow less force to be transmitted to the vehicle occupants at the time of impact.
Implementation of safety measures may require legislative procedures. Whereas in the United Kingdom, much of Europe, and most of the United States it is compulsory to wear seatbelts in a car, such regulation does not extend across much of the developing world. However, even before the requirement becomes widespread, simple educational programs may be developed to help change behavioral patterns of those at risk.
Early aggressive management of those suffering spinal cord injury can help to preserve some neurological function that may otherwise be lost. Early surgical stabilization of injuries has been shown to reduce the hospital length of stay.
Many of the physical complications listed previously can be prevented by appropriate prophylactic treatment or early intervention. Care systems dedicated to the management of spinal cord injury can reduce the incidence of complications such as pneumonia and pressure sores. Simple, inexpensive measures to reduce complications can be used in some circumstances. While specially designed beds and mattresses may reduce the severity and likelihood of pressure sores developing, measures such as careful skin care and regular repositioning are invaluable and easily implemented in poorer economies.
Rehabilitation of patients with spinal injuries can be expensive both in the short term and over a number of years. For this reason, it is recommended that while it is an essential component of health and welfare provision, the most effective way of reducing costs is through preventative measures. Knowledge of quality of life and functional outcomes, along with the involvement of user groups, can help to focus care on key areas and develop appropriate means of support for those at risk of poor reintegration and psychological difficulties.
Independent living can be seen as the goal for the majority of persons with spinal cord injury. Pursuit of the tools necessary to facilitate independent existence is an important role for those involved in public health. An independent lifestyle can be achieved through initial investment and outlay, with a reduction in recurrent care costs.
In developing economies, the importance of preventative health care is even greater. This applies across all areas, from primary through to secondary and tertiary prevention. Reduction in the prevalence of disease and complications will help to reduce the high costs seen with rehabilitation, long-term care, and loss of earnings. Education of decision makers and those at risk of injury can help to promote these preventative approaches.
Conclusions
Spinal injury is a rare but devastating disease. Its effect can be measured from social, health-care, and economic perspectives. Effective preventative measures are the key to reduction of this burden, especially in developing economies. Return to independence after spinal cord injury should be seen as the goal for care providers and planners alike, with the resultant reduction in the burden it may otherwise place.
Bibliography:
- Berkowitz M, O’Leary PK, Kruse DL, and Harvey C (1998) Spinal Cord Injury: An Analysis of Medical and Social Costs. New York: Demos Medical Publishing.
- Bombardier CH, Richards S, Krause JS, Tulsky D, and Tate DG (2004) Symptoms of major depression in people with spinal cord injury: Implications for screening. Archives of Physical Medicine and Rehabilitation 85: 1749–1756.
- Ferrari R and Russell AS (1999) Epidemiology of whiplash: An international dilemma. Annals of the Rheumatic Diseases 58: 1–5.
- Gargan MF and Bannister GC (1994) The rate of recovery following whiplash injury. European Spine Journal 3: 162–164.
- Jackson AB, Dijkers M, De Viso M, and Poczatek RB (2004) A demographic profile of new traumatic spinal cord injuries and stability over 30 years. Archives of Physical Medicine and Rehabilitation 85: 1740–1748.
- Kraus JF, Franti CE, Riggins RS, et al. (1975) Incidence of traumatic spinal cord lesions. Journal of Chronic Diseases 28: 471–492.
- Krause JS, Kewman D, De Vivo MJ, et al. (1999) Employment after spinal cord injury: An analysis of cases from the model spinal cord injury systems. Archives of Physical Medicine and Rehabilitation 80: 1492–1500.
- Lasfargues JE, Custis D, Morrone F, Carswell J, and Nguyen T (1995) A model for estimating spinal cord injury prevalence in the United States. Paraplegia 33: 62–68.
- Martin BW, Dykes E, and Lecky FE (2004) Patterns and risks in spinal trauma. Archives of Disease in Childhood 89: 860–865.
- Melody J (2003) Whiplash Associated Disorder Training Pack. London: British Association for Accident and Emergency Medicine.
- Sekhon LHS and Fehlings MG (2001) Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine 26 (24 supplement): S2–S12.
- Whiteneck G, Meade MA, Dijkers M, Tate DG, Bushnik T, and Forchheimer MB (2004) Environmental factors and their role in participation and life satisfaction after spinal cord injury. Archives of Physical Medicine and Rehabilitation 85: 1793–1803.
- Berkowitz M, O’Leary PK, Kruse DL, and Harvey C (1998) Spinal Cord Injury: An Analysis of Medical and Social Costs. New York: Demos Medical Publishing.
- Melody J (2003) Whiplash Associated Disorder Training Pack. London: British Association for Accident and Emergency Medicine.
- Wood-Dauphine´ e S, Exner G, and SCI Consensus Group (2002) Quality of life in patients with spinal cord injury – Basic issues, assessment and recommendations. Restorative Neurology and Neuroscience 20: 135–149.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








