This sample Occupational Safety and Health Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Preventing occupational disease and injury, eliminating hazards, and improving the quality of the working environment is an essential component of public health and preventive medicine. In industrialized nations, people who are economically active spend about 40% of their waking hours in the working environment. People in developing nations may spend even more of their day working and earning a more meager living. In general, hours spent at work are the most active physically and mentally. The work environment likely includes chemical, physical, and psychosocial hazards that are either not found or are present at much higher or more intense levels compared to those exposures in the general community. Further, the work environment and the nature of work itself may have ramifications beyond the workplace. Indeed, conditions at work, like excessive stress or compromised health due to toxic exposures, may determine many of the qualities of life, health, and well-being outside the workplace.
This research paper reviews statistical measures of occupational safety and health performance, and link these to specific prevention programs. The approach is framed by extensive experience in the manufacturing sector, and especially the motor vehicle manufacturing sector, which is the historical base of the discipline.
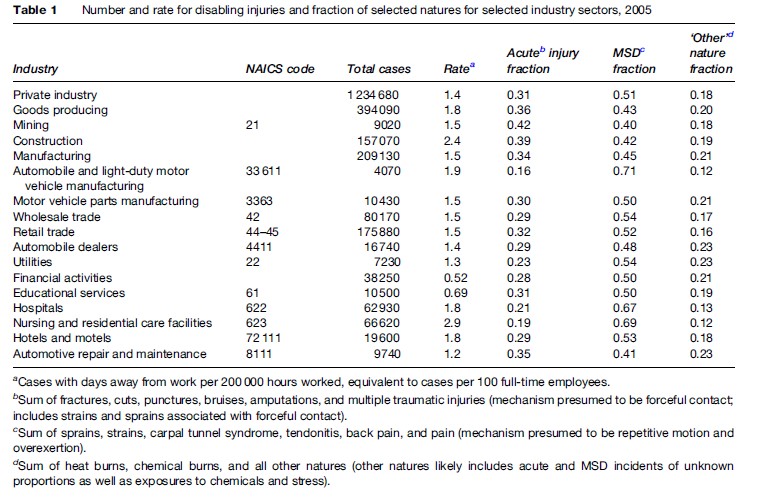
Manufacturing is an important generator of wealth and well-paid employment, but it is only a fraction of the world of work, and in the developed world, a declining fraction. Sectors and occupations historically recognized as ‘dangerous’ include construction, mining (perhaps best understood as construction and excavation underground in poorly ventilated spaces), transportation (including warehousing), and agriculture. Newly emerging as sectors with high risks and therefore opportunities for prevention are the ‘high-risk service sectors,’ including health care and social service agencies. Many service sector workers – for example, hotel staff – perform activities found in the home environment, except much intensified in duration, intensity, and pace, and performed within an authoritarian work organization scheme. Finally, occupational health and safety approaches based on the hierarchy of controls are applicable to the vast array of clerical, technical support, professional, and managerial jobs and environments that encompass nearly half the economy. Table 1 presents the rates and natures of the recorded disabling injuries in various selected sectors of American private employment. The methodology and approaches we describe below for the manufacturing sector can similarly be employed for prevention and control to the risks listed in the table.
General Statistical Measures Of Occupational Injury And Illness
In this section we provide a brief overview of the extent of occupational illness and injury. Much of our focus is on the United States, where conditions and production processes are comparable to those in developed industrialized nations worldwide. Both the nature of work, the distribution of jobs in various workplaces, the extent of exposure, and the lack of regulation make it clear that these conditions and exposures are much worse in developing nations, but few reliable or comparable statistics are available.
In 2005 in the United States, according to its Bureau of Labor Statistics (BLS), there were 4.2 million nonfatal injuries and illnesses in private industry (Bureau of Labor Statistics, 2006). These workplace injuries and illnesses occurred at a rate of 4.6 cases per 100 workers among private industry employers. Approximately 2.2 million of the reported injuries and illnesses were serious enough that the worker was unable to perform his or her normal duties; that is, they involved either days away from work, job transfer, or job restrictions. This injury rate corresponds to an incidence rate for cases with days away from work, job transfer, or restriction of 2.4 cases per 100 workers. These rate data are, by design, underestimates of the true injury and illness rate among workers because they exclude incidents diagnosed among retired or otherwise inactive workers. It is widely acknowledged these data do not include occupational illness arising from long-term exposure. Such conditions are simply neither counted nor, for the most part, even recognized as attributable to occupational exposures.
Despite the fact that these official survey data are widely thought to be undercounts (Rosenman et al., 2006) and largely represent only acute injuries diagnosed by the employers, they still result in substantial costs. In 2004, the workers’ compensation cost of occupational injuries in the United States was $87.4 billion, representing employer expenditures of about $1.76 per $100 of labor cost, with $1.13 per $100 going to actual wage replacement and medical care of workers. The balance of employer costs goes to administration. When a worker does receive benefits, the usual replacement in the United States is generally about half the pre-injury wages. Of the costs to the employer, only slightly more than half represents wage replacement, with the balance going to medical costs (Sengupta et al., 2006).
Other data sources provide a more reliable idea of the much larger impact of the working environment on health than is revealed by workers’ compensation and official occupational injury statistics. One such source is disability insurance. Disability insurance covers costs associated with incidents or illnesses that are not recognized as ‘related to’ workplace exposures or conditions, even if, in fact, workplace conditions either caused or exacerbated the condition. For example, a private insurance company reported an incidence of 9.1 short-term disability claims per 100 covered employees and concluded that of these, one-third were musculoskeletal conditions. A substantial fraction of these musculoskeletal conditions were likely to be of occupational origin. They also reported that long-term disability claims were filed at 0.36 per 100 covered employees, and of these, one-third, again, were musculoskeletal, with a substantial fraction of likely occupational origin (Leopold, 2004). Similarly, claims-based insurance data from an industrial employer revealed approximately a 20 per 100 incidence of claims, with approximately 50% for musculoskeletal or injury causes.
Although health insurance claims are a difficult data source to analyze for possible work-related disorders, some specific databases have been identified that could help elucidate the true work-related incidence of disease and disability (Park, 2001; Reeve et al., 2003). When evaluating general disability insurance data, it is important to keep in mind that the particular condition that has led to the disability may not be the work environment. Rather, it may be the case that the rigor of the work environment requires a worker to withdraw from or delay return to work after a non-occupational illness. Thus, occupational exposures result in lost time, even if the initial incident was not occupational in origin.
Some indications of the extent of chronic disease related to employment can also be gleaned from epidemiological studies, but often these are more difficult to generalize from and true rates are not as readily calculable as in claims-based data.
Analyzing Occupational Injury And Illnesses By Categories
To devise methods of reducing the burden of illness and injury arising from employment and the work environment, it is essential to analyze patterns of disease outcomes in ways that reflect the mechanisms by which the injury or illness may have occurred. The three most useful broad categories are industry classification, occupational group, and health outcomes.
For industry classification, the BLS employs 20 major categories of activity and many subcategories in the official U.S. system for categorizing employment (the North American Industrial Classification System, or NAICS). A useful grouping for analysis by process type is:
- mining and extractive;
- construction;
- transportation;
- manufacturing;
- retail and wholesale trade;
- service (including health care and education);
- finance;
For occupational groups, the BLS employs 36 major categories. Job assignment groups have different spectra of risks. For manufacturing industry, some useful groupings of jobs categories are:
- skilled trades (maintenance, repair, installation, service);
- mechanical material handling (powered industrial trucks, cranes);
- other support (cleaners, production service);
- fixed production (machine operators and assemblers);
- clerical and technical;
- executive and professional.
For health outcomes, the BLS categories that are used to describe the nature of the condition are not as useful. A more useful cause-oriented grouping combining both nature of injury and gravity is:
- fatal or severe acute injuries;
- injuries and illnesses of lesser gravity;
- musculoskeletal disorders;
- short-onset chemical effects;
- chronic disease related to long-term chemical exposure;
- outcomes from psychosocial stressors.
It is important to realize that there is a great deal of overlap between categories in actual practice. First, with regard to health effects, it is very likely that a worker who develops one kind of impairment may be simultaneously exposed to several hazards and would, in any case, be more susceptible to additional problems once any aspect of his or her health has been compromised on the job.
Also, many types of jobs cross industry category lines. For example, truck drivers are employed in the service sector, in construction, in manufacturing, and in agriculture, not just in transportation. Thus they face the same risks as those of a transportation employer and in addition are exposed to the particular hazards that are found in their industrial sector.
Some of these employment categories are very broad. For example, service sector job environments are quite diverse and include two major and very different employment groups: health care and education services. Health care itself is a very broad category that clearly encompasses many more opportunities for intense exposure to injury and chemical and physical hazards, as well as unique hazards in patient handling and infectious disease. Educational services’ physical hazards are less intense, but they are not benign. Hazards in educational services can include exposure to infectious agents; physical attack, even murder; very poor indoor air quality; and extreme stress.
It is also important to recognize that the diversity of the employed population may lead to differing levels of risk in the various worker demographic groups present. The differing risk may be a reflection of different susceptibilities and physical characteristics, different types and levels of exposure, or both. One typical breakdown of worker demographics focused on vulnerability is:
- women;
- young workers;
- older workers;
- minority status;
- immigrant status;
- poverty status.
These demographic categories may not be particularly useful for prevention or intervention. It is, in general, very difficult to change the workers (and probably illegal to try), and in any case, making the workplace safe for all demographic groups qualified to work in it is the preferable approach. Often if different risks are observed between workers in these categories, the differences arise from substantially different employment patterns and exposures on the job rather than from true inherent differences among categories of workers. Indeed, studies that have controlled for job characteristics and industrial sector have generally found fewer differences based on worker demographics. In addition, another practical problem is that vulnerable workers may be exposed to worse working conditions and at the same time may have less ability to ensure that their employment rights are intact. Thus, ensuring that workplace rights and guarantees are available to all workers, rather than creating separate employment classes, is the means by which the workplace can be made safer for all workers.
Contrasting Approaches To Prevention
In 1931, H.W. Heinrich published Industrial Accident Prevention, and his approach became the dominant paradigm for prevention of occupational injury (Heinrich, 1931). Underlying his model was the assertion that 90% of workplace injuries are caused by ‘unsafe acts’ – in other words, the antithesis of a systems approach to accident prevention. The concept and the canonically repeated 90% incidence became a mainstay of occupational safety practice and theory. This proportion has never been verified in the published literature. The idea that unsafe acts cause most accidents and injuries remains the conceptual framework underlying the historical approach to health and safety. Specifically, the unsafe acts theory posits that:
- accidents are caused by unsafe acts and operator error;
- accidents can be averted if employees are trained to follow safety rules;
- employees should be motivated to follow safety rules.
In the 1970s, the quality movement, a new and contrasting approach to that of Heinrich and the ‘unsafe worker’ conceptualization, was developing. In the quality movement approach, occupational injury is viewed as follows:
- Adverse effects are caused by the physical environment and production system.
- Processes can be modified to avoid injuries and illnesses.
- Workers can be trained to recognize hazards and system failures.
- Workers can be motivated to participate in hazard identification and abatement.
The quality movement is reflected in competing approaches to injury prevention; the best known is the Hierarchy of Controls (Rosenstock, 1996; Plog et al., 2002). The hierarchy is an approach to modifying the environment in various categories in order to prevent injury and illness, rather than prescribing worker-behavioral modification within an unchanging environment. The ‘hierarchy of controls’ is:
- elimination;
- substitution;
- engineering;
- warnings;
- training and procedures;
- personal protective equipment.
The hierarchy of controls has been more readily recognized in practice for chemical and physical health hazards than it has for safety hazards. For example, most modern safety practitioners will prefer higher-level environmental controls for noise and chemical exposures, like vibration damping, noise enclosure or fume capture technologies, to earplugs and respirators. The approach is far less commonly applied to injury controls, where, in the United States, safety rhetoric favors ‘working safely’ rather than extending the reach of safety devices and guards. The hierarchy of controls, however, is much more commonly practiced for injury control in the European Union, where most experts agree that ‘unsafe behaviors’ are best reduced by modifying the social environment or work organization that causes and reinforces such behaviors.
Generalized Elements Of A Workplace Health And Safety Management Program
The quality movement and other advances in the management and prevention of occupational safety and health risks made it clear that a comprehensive safety and health management system for abating workplace hazards and improving protections was needed. In addition to the expansion of the conceptual framework underlying accidents from unsafe workers to more realistic systems approach, the need for such a generalized program arose, in part, because even full compliance with Occupational Safety and Health Administration (OSHA) standards was less than fully protective. For example, the majority of recognized injuries arose from ergonomic hazards, for which no OSHA standard exists. Further, even if exposures were in compliance with the permitted exposure levels (PELs), chemically related symptoms still would arise. Standards that were developed to address key hazards, like machine guarding, walking and working surfaces, and powered industrial trucks, were incomplete and not specific on allowed and prohibited conditions.
To respond to the perceived need for a comprehensive safety and health management system, OSHA developed its Program Evaluation Profile (PEP), which outlined the key elements in a management system (Occupational Safety and Health Administration, 1996).
Later, an industry consensus standard entitled Safety and Health Management Systems (Z-10-2005) was developed and ratified under the auspices of the American National Standards Institute (ANSI) (American Society of Safety Engineers, 2007).
The elements of a workplace health and safety management program represented in this standard are generally recognized to be:
- management commitment and employee involvement;
- worksite analysis;
- hazard prevention and control;
- safety and health training.
Benchmarks for management commitment and employee involvement are the demonstration that policies and objectives of health and safety in the workplace are established and communicated. There must be visible involvement of top management, and employees must be involved in identifying hazards and solving abatement issues. Responsibility for safety and health must be clearly assigned, and those assigned must have adequate authority to meet their responsibilities. Managers, supervisors, and employees are held accountable in the management system, and program operations must be reviewed at least annually.
The requirements for worksite analysis within the health and safety management system include carrying out a baseline survey of hazards and carrying out a change analysis each time that any change occurs in the work environment that has an impact on the existing occupational health and safety conditions. There must also be ongoing job hazard analysis. Worksite analysis requires that regular self-inspections and routine inspections be made and that each employee know the appropriate person to notify about hazards and how to make such notification. There can be no reprisals for hazard notification. An incident investigation mechanism must be in place, and there must be an established means for analyzing any injuries or illnesses that occur and are related to the workplace environment.
Hazard prevention and control is the requirement that hazards be controlled to the extent feasible and that safe work practices be established that are based on the aforementioned job hazard analysis. It is the obligation of supervision to enforce and reinforce safe practices, but such supervision must include fair disciplinary procedures. In order to be in compliance with this aspect of the standard, hazards must be identified and corrected in a timely fashion and there must be adequate preventive maintenance procedures in place and in practice to ensure that already recognized hazards are controlled and that no new hazards are inadvertently introduced. A prevention and control program must include medical services. Minimally, first aid and CPR must be available on every work shift. There must be adequate preparation for dealing with emergencies, and evacuation routes and emergency numbers must be prominently displayed.
Benchmarks for adequate safety and health training are that employees can explain how and why they do their jobs safely. If employees are required to use personal protective equipment (PPE), those employees must be able to demonstrate knowledge about the appropriate use, care, and maintenance of their assigned equipment. Benchmarks for supervisor safety and health training are that the supervisor must be able to explain the rules and procedures that are in place, including the training and enforcement requirements. It is the obligation of managers to be able to explain the various levels of responsibilities.
The Matrix Approach To Recognizing And Controlling Safety And Health Hazards
Relative risks of disabling occupational injury, stratified by occupational classification, are shown in Table 2. The rate of disabling injuries among material-moving workers is more than 20 times that of executives. Production workers, like assemblers and machine operators, suffer more than 10 times the disabling injury rate. Service workers suffer nearly 8 times the rate, clerical workers suffer 3 times the rate, and even professional workers suffer twice the rate as the executive reference group. These differences imply that any measurement of safety and health performance in a workplace has to take occupational mix into account.
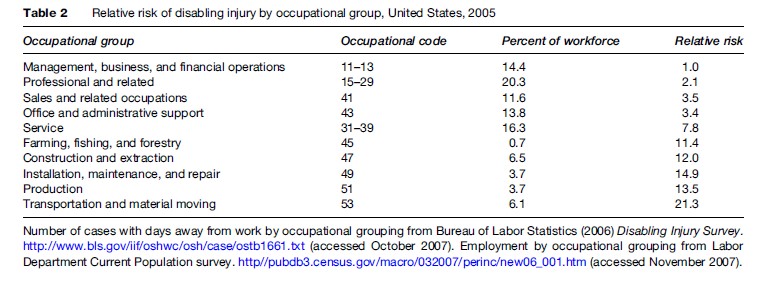
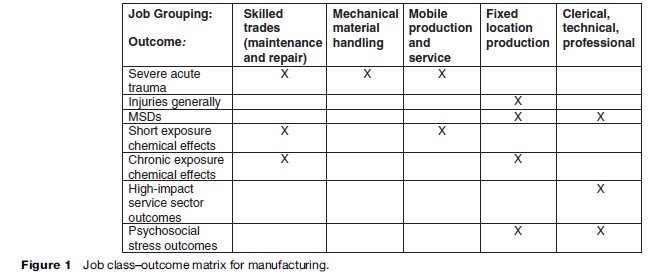
In Figure 1 we illustrate a job–outcome matrix, a useful tool for analyzing health outcomes and job classes. This figure illustrates the combination for the manufacturing sector, but a similar matrix with perhaps different categories can be created for any industry sector. Similar matrices have been developed for jobs and exposures. Such matrices are regularly used in epidemiological occupational health studies.
An Example Of Application Of The Matrix Approach: Manufacturing Sector
Because of the great utility of the matrix approach, we illustrate its application here with a manufacturing sector example. The example combines experience in a primarily transportation equipment and metalworking manufacturing environment with diverse other sectors where the workers were represented by a single trade union with an active health and safety program. This example provides a framework for analyses of other sectors, for which there is currently less practical experience that has been applied to the matrix model. The reader is referred elsewhere for fuller description of the processes and some of the outcomes in this sector (Mirer, 1998). The fatality data supporting these analyses have been collected and published as well (International Union, 2006), and in this research paper we link in, for the first time, the disability insurance data. We present the model on an outcome by outcome basis.
The model was framed by observations over many years of differential outcomes across job assignments. Specifically, the rate for fatal injuries was very elevated for the skilled trades (maintenance and repair workers) compared to production workers at fixed stations (assemblers and machine operators). This differential risk was a major driving force in prevention programs over decades.
We now proceed to illustrate prevention programs for various outcomes: fatal or severe acute injuries; injuries generally; musculoskeletal disorders; short-onset short duration chemical exposure effects; chronic exposure chemical effects; high-risk service sector outcomes; and outcomes from work-related psychosocial stress.
Outcome: Fatal Or Severe Acute Injuries
Table 3 presents proportions of fatal injuries over a 23-year period, stratified on selected exposure categories. We estimate that no more than 20% of hourly workers are skilled trades. Since 41% of fatalities were skilled trades workers, we calculate that the fatality risk is about fourfold compared to the rest of the hourly workforce.
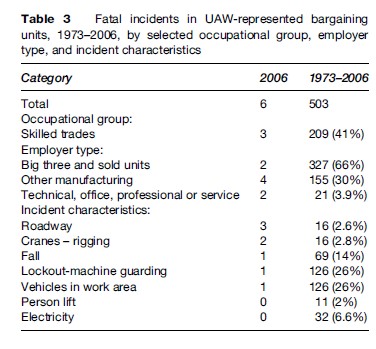
Skilled trades work involves installation, repair, and maintenance of machinery, equipment, and building structures, while production work does not. Thus, using a job-matrix approach, it makes sense that these work activities should be the focus for fatality prevention. Among the health and safety interventions carried out, an initial focus was energy lockout. Energy lockout encompasses shutting off the power to equipment (and also releasing stored energy) and then securing the energy sources with individually assigned locks (lockout process) before engaging in repair and maintenance activities. (Sometimes a less effective ‘tagout’ approach is used, in which the energy source is merely tagged to warn against its usage.) The energy lockout approach is described in the OSHA standard for control of hazardous energy (1910.147). After experience with systematic application of energy lockout, it has become clear that lockout should be an integral part of machine guarding and control circuitry, and it is now required by the OSHA machine guarding standard (1910.212) and the national electrical code (NFPA 79A).
Our analysis also shows that falls from heights to a lower level are another major cause of death. Here, gravity itself is the hazardous energy source. Unlike in the construction industry, there is no fall prevention standard for general industry. Therefore, it became necessary to develop and launch self-designed programs to prevent fall-related fatalities. The approach used was to blend fall arrest equipment with the higher-level control of workplace design. The program emphasized installation of guardrails on maintenance platforms. This approach specifies implementation of the OSHA standard for walking and working surfaces, and frames the new ANSI standards for fall-prevention programs. The ANSI standard is an example of how preventive approaches for one sector can be generalized to other at-risk employment sectors.
Other major sources of energy that must be controlled in order to prevent fatal injuries are material handling equipment like industrial trucks, cranes, and other vehicles in work areas. When a study was carried out in the automobile manufacturing industry, researchers found that obstructed aisles were strongly associated with increased collision risk (Collins et al., 1999). The industry formulated a program to clear the path of vehicle travel to prevent collisions.
In summary, fatality and serious injury risk is associated with maintenance, with work at nonstandard locations, and with mechanical material handling. The most fundamental corrective is to design and build production equipment and the environment to eliminate the problem. Designing for maintenance would also improve reliability of production and reduce downtime and waste. Effective design for maintenance will depend on involvement of employees, who will eventually maintain and repair the equipment in the earliest parts of the design phase.
Outcome: Injuries In General
The dominant measure of health and safety program effectiveness in a facility is the injury-illness incidence rate, measured either as total cases or as cases resulting in disability. Figure 2 illustrates the experience in the motor vehicle assembly sector in the United States, and illustrates the importance to prevention of complete injury and illness reporting.
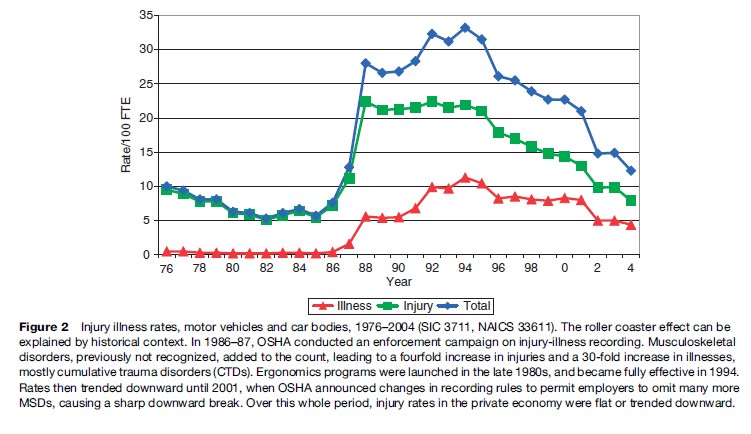
The general injury and illness incidence rate in this sector, as reported by the BLS, was slowly trending down, as was the rate for all private employment from 1976 to 1986. From 1986 to 1994, however, there were steep increases in the recorded rates, with a six fold increase in the overall rate, a fourfold increase in the injury-only rate, and greater than a 30-fold increase in the ‘illness’ rate. Then, from 1994, rates trended down again. By 2005, there was a threefold decrease. Similar but less dramatic time trends were observed in motor vehicle parts and related sectors. Meanwhile, the time trends in the rest of private employment were trending down a few percent.
The changes in the various reported rates can be explained by events in the health and safety environment. From 1986 through 1990, OSHA vigorously enforced injury and illness recording requirements, particularly in large facilities in the manufacturing industry, focusing on meat packing and the auto sector. This enforcement involved assessment of six-figure penalties for willfully not recording. One result of the OSHA enforcement program was that it was possible to determine what types of injuries were being underreported. The predominant cases not recorded in the OSHA logs prior to the enforcement crackdown were musculoskeletal disorders (MSDs). Musculoskeletal disorders are defined by the U.S. Department of Labor as ‘‘an injury or disorder of the muscles, nerves, tendons, joints, cartilage, or spinal discs. MSDs do not include disorders caused by slips, trips, falls, motor vehicle accidents, or similar accidents. MSDs include sprain and strain injuries and disorders such as carpal tunnel syndrome’’. The events that cause these are overexertion and repetitive motion. Practitioners believe that many sprain or pain events are acute flareups of chronic conditions. The chronic conditions may arise from long-term repetitive exposures – such as kneeling at work eventually leading to an acute ‘knee sprain’ – or be sequels to a primary overexertion, such as a back injury.
The undercounting of MSDs was primarily identified when paid workers’ compensation claims were analyzed in comparison to the OSHA-required data on occupational injuries. All paid workers’ compensation cases, of course, have an implicit recognition of the work relatedness of the injury; they almost always involve time lost from work and thus should appear in the OSHA data, but few of these cases were recorded in the OSHA-required database.
The observations that musculoskeletal disorders were the most common cause of injury triggered participatory ergonomics programs at every unionized facility in this sector. These programs became fully effective around 1994 and it is very likely that some of the upward trend in the data shown, up to the year 1994, was the combined result of better recognition of MSDs as work-related and of better recording of incident cases. The decreasing trends that are observed in Figure 2 are almost certainly a reflection of the abatement of risk factors for musculoskeletal disorders that also followed the development of the ergonomic programs in the industry. The ergonomics programs continued to mature and dominate the reported injuries trend until 2001. In 2001, OSHA changed the recording rules to permit employers to omit recording of previously recordable injuries, and provided incentives to reduce recording by targeting inspections for workplaces that did record and report more injuries.
Outcome: Musculoskeletal Disorders
Once MSDs are recorded, it becomes clear that MSDs among production and service workers dominate the injury-illness rate in the motor vehicle sector and nearly every other sector of the economy.
The overall number of MSDs comes from a combined count of strain and sprain injuries and cumulative trauma disorders. The impact of MSDs arising from overexertion or repetitive motion on the overall injury rate can be inferred from the Bureau of Labor Statistics Disabling Injury Survey. These data are derived from a large sample of employer injury-illness records, coded by BLS for nature of injury, event or exposure, body part, and agent, stratified on industry and worker characteristics. Table 1 shows that in the motor vehicle manufacturing sector, 71% of disabling injuries are known to be MSDs. In virtually every other sector, the proportion of MSDs is 40% or greater.
A variety of MSD risk factor assessment checklists or simple calculation instruments based on the force-frequency-posture-duration paradigm are available for use by nonspecialist professional practitioners and lay job analysts. These include the NIOSH lifting guide (National Institute for Occupational Safety and Health, 1994), the Rapid Upper Limb Assessment Tool (McAtamney et al., 1993), and the ACGIH Hand Activity Level (Franzblau et al., 2005).
Elements of an effective ergonomics program include prospective job analysis, injury illness analysis, symptom surveys, reactive job analysis following identification of cases, risk factor abatement, reanalysis of abated jobs, worker training for participation in risk factor identification and participation in medical surveillance, and ongoing evaluation (National Institute for Occupational Safety and Health, 1997).
Job analysis for abatement at fixed workstations should also identify acute injury hazards, such as handling sharp objects, deficiencies in machine guarding, and the risk of hand tool use without appropriate fixtures for the work piece.
An example of a higher level of control is designing a product, such as a motor vehicle or significant home appliance, to encompass appropriate health and safety safeguards and features. Employees whose work involves using such a product should participate in redesign of the product, as well as in identifying hazards and recommending changes in workstations, work methods, and tooling.
Outcome: Illness From Intermittent, Short-Duration, High-Level Chemical Exposures
Fatalities associated with confined space entry dominate the documented instances of adverse health effects that result from short-duration, high-level chemical exposures in the manufacturing industry. We still do not have an accurate measure of the probability of less acute illnesses that arise from lower-level or repeated incidents that do not result in fatality or emergency response. Anecdotal reports of employee symptoms from major and minor spills of process chemicals, emissions from process upsets, fires, and explosions are frequent but not systematically documented. For example, the chemical exposures during restoration of production after a fire, spill, or process upset can be substantial. Servicing of ventilation, air cleaning, and other environmental control equipment is a significant concern. Disturbing or removing asbestos and lead paint is an important risk in the auto industry, where the occupational groups most likely to be impacted are skilled trades workers and nonskilled maintenance and cleanup workers. Health impact can also be inferred from limited studies that reveal chronic illnesses among skilled trades workers whose chemical exposures follow this pattern due to the nature of their work assignments (Park and Mirer, 1996).
Preventive measures include job-specific chemical hazard control procedures and information for nonroutine activities (supported by 1910.1200), hazardous waste and emergency response operations programs (supported by 1910.120), and confined space entry programs (supported by 1910.146), as well as construction asbestos and construction lead programs. An industrial hygiene evaluation of nonroutine activities needs to be carried out in order to develop appropriate exposure-based protective measures and information. The limitations of an industrial hygiene exposure measurement approach, however, are the governmental exposure limits (OSHA PELs) discussed below. Without appropriate and available PELs, industrial hygiene evaluations are limited.
The fundamental prevention of these outcomes depends on eliminating or reducing sources of nonroutine exposure: Eliminate confined spaces or the need to enter those spaces; clean without solvents; and modify equipment or production processes to prevent spills, leaks, and process upsets. A canonical solution is to substitute nonhazardous or less hazardous materials; however, examples of such substitution are largely limited to exchanging water-based cleaners for volatile organic solvents.
Outcome: Illness From Long-Term Chemical Exposures
The risk of a work-related fatality caused by illness from long-term chemical exposures far exceeds that of a fatality caused by traumatic injury (Fingerhut et al., 2006). The fatality risk of United Auto Workers members generally, calculated from the database described above, is about 5 per 10 000. For the high-risk skilled trades worker group, the risk is about 2 per 1000. By contrast, the risk over the whole private workforce is 2 per 1000, and that for construction workers (comparable to UAW skilled trades) is 8.7 per 1000. Translating the rate of mortality from occupational cancer generally into the same units, based on the very limited estimate of 4% of cancers due to occupational exposures, yields an estimate of 1 per 100, between 5 and 20 times the rate of traumatic injury fatalities.
Studies in the U.S. motor vehicle manufacturing industry have reported increased mortality from cancer among foundry workers (lung), workers exposed to metalworking fluids (a variety of sites), vehicle assembly workers (lung), stamping and sheet metal fabricators (lung, stomach), and electronics workers (brain) (Mirer, 2003). These illnesses arose from exposure levels that were in compliance with current and past occupational health exposure limits (except for silica in foundries).
Respiratory conditions are the most prominent chemically related noncancer illness observed among foundry workers and workers exposed to metalworking fluids.
Prevention of these adverse outcomes is hampered by the absence of governmentally enforced or generally accepted exposure limits that sufficiently restrict exposure to prevent a significant risk of adverse effects. This problem has largely been discussed in the political arena rather than in the peer-reviewed literature. Prevention strategies revolve around best practices for ventilation, prevention of skin contact, and medical surveillance. Control of exposure is supported by the Hazard Communication standard (1910.1200).
Outcome: High-Impact Service Sector Occupations
Service sector occupations are found in virtually every industry sector. For example, health-care workers are found in most large factories. Their exposures include infectious disease and patient movement, as well as the potential for client violence. Other occupations such as personnel management and union representation have the aspect of social work, also with a potential for client violence.
The most applicable regulation is bloodborne pathogens (1910.1030), although a general infection control program is indicated in every large facility.
Outcome: Somatic And Mental Illness Arising From Work-Related Psychosocial Stress
The prominence of mental illness as a leading cause of disability among manufacturing workers suggests that work-related psychosocial stress may play some causal role. Adverse effects of work-related psychosocial stress have largely been investigated outside the manufacturing sector, in job settings with less intense exposure to physical and chemical hazards. Stressors frequently mentioned under the rubric ‘work organization’ include high-demand low-control jobs, lack of social support, and effort–reward imbalance. These same stressors may be present, with similar or greater intensity, in the manufacturing environment. The effect of stressors may be direct or indirect through an association with increased health risk behaviors such as smoking, substance abuse, or poor diet.
The association of noise exposure, prominent in the manufacturing sector, with hypertension has been observed in a number of studies, but this endpoint has not been taken into account in priority of noise abatement programs. Similarly, adverse effects of various unusual work schedules – extended duty (frequently named ‘overtime’), rotating shift, afternoon and night shift – have been observed but not taken into account. The contribution of work-related musculoskeletal pain directly to cognitive effects and indirectly to health risk behavior has not been sufficiently explored.
Preventive measures for outcomes of psychosocial stress are not generally a part of occupational health and safety programs. These measures are addressed by aspects of labor law – labor standards, hours of work, antidiscrimination legislation. To the degree that unequal treatment and lack of access to information and input on work questions contribute to stress, a labor agreement may alleviate these problems.
Bibliography:
- American Society of Safety Engineers (2007) Impact of ANSI Z10: Perspectives from ASSE members. Compass (special issue): 1. http://www.asse.org/practicespecialties/docs/Z10SpecialIssue.pdf (accessed October 2007).
- Bureau of Labor Statistics (2006) Case and Demographic Characteristics for Work-related Injuries and Illnesses Involving Days Away from work. http://www.bls.gov/iif/oshcdnew.htm (accessed October 2007).
- Collins JW, Smith GS, Baker SP, and Warner M (1999) Injuries related to forklifts and other powered industrial vehicles in automobile manufacturing. American Journal of Industrial Medicine 36: 513–521.
- Fingerhut M, Nelson DI, Driscoll T, et al. (2006) The contribution of occupational risks to the global burden of disease: Summary and next steps. Medicina del Lavoro 97: 313–321.
- Franzblau A, Armstrong TJ, Werner RA, and Ulin SS (2005) A cross-sectional assessment of the ACGIH TLV for hand activity level. Journal of Occupational Rehabilitation 15: 57–67.
- Heinrich HW (1931) Industrial Accident Prevention: A Scientific Approach. New York: McGraw-Hill.
- International Union, UAW (2006) Occupational Fatalities among UAW Bargaining Units 2005. http://www.uaw.org/hs/06/2006_poster6. pdf (accessed November 2007).
- Leopold R (2004) A Year in the Life of a Million American Workers. New York: Metropolitan Life Insurance Company.
- McAtamney L and Nigel Corlett E (1993) RULA: a survey method for the investigation of work-related upper limb disorders. Applied Ergonomics 24: 91–99.
- Mirer F (1998) Automobile and transportation equipment industry. In: Encyclopedia of Occupational Safety and Health, vol. 4, sec. 91.2–91.8.
- Mirer FE (2003) Mortality in the motor vehicle and motor vehicle parts industry. Journal of Occupational and Environmental Medicine 45(8): 789–792.
- National Institute for Occupational Safety Health (1994) Applications Manual for the Revised NIOSH Lifting Equation NIOSH Publication No. 94–110. http://www.cdc.gov/niosh/docs/94-110/ (accessed October 2007).
- National Institute for Occupational Safety and Health (1997) Elements of Ergonomics Programs: A Primer Based on Workplace Evaluations of Musculoskeletal Disorders. NIOSH Publication No. 97–117. http://www.cdc.gov/niosh/docs/97–117/ (accessed October 2007).
- Occupational Safety and Health Administration (1996) Program Evaluation Profile (PEP). http://www.osha.gov/SLTC/safetyhealth/ pep.html (accessed October 2007).
- Park RM (2001) Medical insurance claims and surveillance for occupational disease: Analysis of respiratory, cardiac, and cancer outcomes in auto industry tool grinding operations. Journal of Occupational and Environmental Medicine 43: 335–346.
- Park RM and Mirer FE (1996) A survey of mortality at two automotive engine manufacturing plants. American Journal of Industrial Medicine 30: 664–673.
- Plog BA, Niland J, Quinlan PJ, and Plog H (2002) Fundamentals of Industrial Hygiene. Itasca, IL: National Safety Council.
- Reeve GR, Stout AW, Hands D, and Curry E (2003) Inpatient hospital admission rates for nonmalignant respiratory disease among workers exposed to metal removal fluids at a U.S. automobile manufacturer. Applied Occupational and Environmental Hygiene 18: 930–938.
- Rosenman KD, Kalush A, Reilly MJ, Gardiner JC, Reeves M, and Luo Z (2006) How much work-related injury and illness is missed by the current national surveillance system? Journal of Occupational and Environmental Medicine 48: 357–365.
- Rosenstock L (1996) The future of intervention research at NIOSH. American Journal of Industrial Medicine 29: 295–297.
- Sengupta I, Reno V, and Burton JF (2006) Workers’ Compensation: Benefits, Coverage, and Costs, 2004. Washington, DC: National Academy of Social Insurance.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








