This sample Rhinoviruses Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Introduction
The common cold has that name for a reason: It is the illness that most frequently affects humans around the world. Rhinovirus is the causal agent for about 50% of common colds.
Human rhinovirus (HRV) has a special affinity for the nasal airway mucosa (rhino means nose). Rhinoviruses can infect ciliated cells in the nasal epithelium but may also infect other nasal cells. ICAM-1 is the receptor that most rhinovirus serotypes use to gain entrance into human cells (Greve et al., 1989). A minority of rhinovirus serotypes use the LDH receptor and one rhinovirus serotype uses sialoprotein. Rhinoviruses belong to the Picornavirus family and are closely related to the enteroviruses. In contrast to enterovirus, however, rhinovirus is killed by gastric acid and does not cause gastrointestinal infection in normal individuals. Laboratory detection of infectious rhinovirus has been performed in human fibroblast monolayer cultures for many years. Recently, more sensitive methods for detection of rhinovirus RNA utilizing reverse transcription polymerase chain reaction (RT-PCR) technology have provided new perspectives toward understanding the epidemiology of rhinovirus infection, and the clinical implications continue to be developed.
Environment
Rhinovirus is common throughout the world. Adults usually contract colds from children living in the same household. Crowded places such as nursery and day care centers, schools, and military camps are ideal settings for high transmission rates of rhinovirus among young adults and children. Rhinovirus infections occur throughout all seasons, but the infection rate of rhinovirus colds seems to vary during the year due to the prevalence of other more seasonal respiratory viruses. Rhinovirus accounts for up to 80% of colds during the fall season in temperate areas of the United States, but occur less frequently during the winter and spring months when influenza virus types A and B, parainfluenza types I–III, respiratory syncytial virus, adenovirus, coronavirus, metapneumovirus and bocavirus are also present. In tropical areas, the respiratory virus season coincides with the rainy season from May through November. Recent new epidemiologic data of rhinovirus infection determined by RT-PCR suggest that the relative number of rhinovirus infections over the year is fairly constant. It is interesting to note that the frequency of rhinovirus infections may not be a result of the effects of temperature or humidity on rhinovirus survival in nature, but rather that climate alters human behavior. One hypothesis suggests that minor climate changes, such as cooler air or rainy days, will keep people indoors and thereby increase the risk of rhinovirus transmission.
Transmission
Most rhinovirus infections are thought to occur when virus deposited onto the fingertips is introduced to the conjunctiva or nose (self-inoculation from fomites), although small particle aerosol transmission is also a potential inoculation route. The number of rhinovirus particles required to infect nonimmune individuals is low; indeed, a tissue culture infectious dose50 less than 10 can cause infection. Rhinovirus deposited in the conjunctiva reach the nose by way of the tear duct to cause infection in the nose. The eye is not infected following deposit of rhinovirus. Inoculation of rhinovirus into the oral mucosa does not cause infection of the oral or tonsillar mucosa. Saliva may occasionally contain a small amount of rhinovirus, probably from diluted nasopharyngeal secretions, but in general transmission by coughing, sneezing, kissing, or drinking from the same glass is not likely to occur in otherwise healthy individuals. On the other hand, transmission of rhinovirus in nasal mucus from a person with a cold to a susceptible individual is likely either by touching shared environmental objects or by direct hand-to-hand contact (handshakes, holding hands, or high fives) followed by self-inoculation with a contaminated finger into the nose or eye. Rhinovirus can survive on environmental surfaces for at least 4 days. Adults with colds commonly contaminate environmental surfaces during normal daily activities. An individual is most contagious during the first several days of the cold, when the concentration of rhinovirus in nasal secretions is highest. Rhinovirus infection may also play an important role in dispersal of bacteria, such as community-acquired methicillin-resistant Staphylococcus aureus (MRSA), especially among children.
Pathogenesis
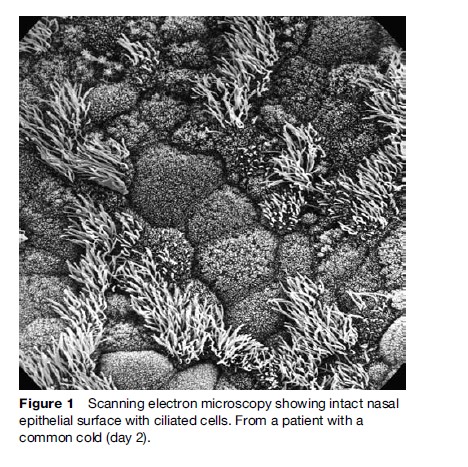
Rhinovirus has a propensity to affect young children disproportionately. A recent study demonstrated that preschool-age children have approximately six rhinovirus infections per year. These infections are caused by different rhinovirus serotypes. Each serotype is thought to give lifelong immunity, but with at least 100 different rhinovirus serotypes, it is no wonder that colds are common. Rhinovirus replicate in the nasal cells for up to 3 weeks until the humoral neutralizing antibodies terminate the infection. Following rhinovirus infection, most individuals develop neutralizing antibodies of 1:16 dilution or greater, and are resistant to reinfection with the same serotype. Rhinovirus infection causes lysis of the infected cells and a decrease in nasal mucociliary clearance. However, the nasal lining remains intact, as observed by light and scanning electron microscopy (Figure 1), because only a limited number of cells are infected at one time. The symptoms of a rhinovirus infection are thought to be caused by the host response to the rhinovirus infection (Hendley, 1998) due to an elaboration of pro-inflammatory mediators and cytokines, and the influx of a high number of polymorphonuclear cells.
Several inflammatory pathways, including neurologic reflexes triggered by the infection, have been identified as playing a role in the pathogenesis of rhinovirus symptoms. Increased kinin levels are found in nasal secretions during rhinovirus infection and may be responsible in part for sore throat symptoms and contribute to rhinorrhea due to plasma transudation (Proud et al., 1990). Kinins are also thought to release histamine from mast cells, although most studies have not demonstrated elevated levels of histamine in nasal secretions during colds. Inflammatory events that occur during rhinovirus infection include stimulation of pain, cough, and sneeze reflexes, vasodilation, transudation of plasma, and increased glandular output of secretions from goblet cells and seromucous glands. The parasympathetic tone is increased during the early phase of a cold, resulting in an increase of secretions from the anterior serous gland on the nasal mucosa. Several pro-inflammatory mediators are increased (e.g., interleukin (IL)-1, -6 and -8). IL-8 is a chemoattractant for polymorphonuclear leukocytes (PMNs) and results in an influx of PMNs on days 1 and 2 during rhinovirus infection. The number of PMNs increases about 100-fold in nasal secretions and has been found to correlate well with symptom expression. Colored nasal discharge (yellow or green) occurs in about 50% of adults and correlates with the increased number of PMNs, but bacteria have not been shown to increase in the nasopharynx during uncomplicated colds.
Symptom Expression Of A Rhinovirus Infection
Although the majority of rhinovirus infections occur in children, our knowledge of the symptomatology is mainly acquired from adults. Accurate determination of symptoms is a challenge in children because symptoms are reported second-hand by parents trying to interpret what their child may feel. Two studies have evaluated the expression of cold symptoms in children who were brought to the doctor. A recent study evaluated cold symptoms in normal school-age children who actively participated with the parent in recording their symptoms (Winther, 2002). Cough, nasal congestion, and runny nose were present in roughly 60% of school-age children and continued for more than 10 days in uncomplicated colds. Feverishness was reported in 15% during the early phase. Rhinovirus was detected in 46% of these reported colds, and one or more bacterial pathogens were isolated in 29%. Symptom profiles for rhinovirus illnesses versus those with bacteria isolated were not different. In adults, 60% of those with colds report sore throat, sneezing, nasal discharge and obstruction, while cough and malaise are reported in approximately 40%. Fever is rare in uncomplicated colds, and feverishness is reported in less than 10% of adults with colds. Most cold symptoms in adults have diminished by day 7, with sneezing, congestion, and runny nose reported in less than 20%, whereas cough is still reported as present in roughly 40%.
Different serotypes of rhinovirus are thought to cause a similar symptom profile, although the symptom severity may vary due to the influence of stress and the status of the immune system and host responsiveness. Experimental rhinovirus infections with two different rhinovirus serotypes have demonstrated that approximately 20% of antibody-free adults become infected following rhinovirus challenge but do not report symptoms. The reason for this is unknown, but a similar trend has been found in children. Roughly 30% of children may have a rhinovirus infection without the signs or symptoms of a cold. This may be caused by infection without symptom expression, or that the cold symptoms are not recognized by the parents.
Signs Of Rhinovirus Infection
Examination of the nasal cavity in adults with rhinovirus infection reveals an increase in nasal secretions but is otherwise unspecific, since abnormal erythema and swelling of the turbinates is seldom observed. Rhinovirus infection causes abnormalities in the Eustachian tube and middle ear. Eustachian tube dysfunction results in intermittent negative middle ear pressure and fluid accumulation. Abnormal middle ear pressure can easily be measured by tympanometry and is present in 40–75% of rhinovirus infections in both children and adults. Approximately 40% of young children have changes in middle ear pressure prior to the time when the parent or caretaker realizes that the child has a cold (Moody et al., 1998). The causes of abnormal middle ear pressure during colds are unknown. Rhinovirus infection of the adenoid in the nasopharynx may result in Eustachian tube dysfunction, or rhinovirus infection may spread into the Eustachian tube and middle ear.
Abnormalities of the paranasal sinuses are also very common during the course of rhinovirus infection, as evidenced by computed tomographic scanning (CT scan). Image studies have shown sinusitis during the first week of illness in up to 75–87% of children and young adults, suggesting that sinus involvement is an inherent feature of a cold. It has recently been shown that nose blowing can generate intranasal pressure sufficient to propel nasal secretions into the sinus cavity. The majority of the abnormalities observed by CT scans during colds are likely due to accumulation of sinus secretions rather than mucosal swelling. Stagnant secretions in the sinuses may be due to blockage in the ostiomeatal complex, a narrow opening from the sinus to the nose, or it may be due to decreased ciliary clearance in the sinuses.
Clinical Diagnosis
Colds in adults are usually self-diagnosed, as everyone is familiar with the symptoms of a cold. Adults may commonly misdiagnose the involvement of a viral infection in the sinuses and middle ear as a bacterial complication, when in fact it is part of the rhinoviral infection.
Differential diagnoses to common colds are allergic rhinitis and vasomotor rhinitis, both of which will usually produce more prolonged sneezing attacks than the common cold. Rhinovirus infection can be distinguished from classic influenza in adults based on the more acute onset of malaise and frequently occurring fever present with influenza. However, milder cases of influenza cannot be easily distinguished from rhinovirus infection, especially in children.
Clinical Implications
Following introduction into the nose, rhinovirus can first be recovered from the adenoid area in the nasopharynx. Over several days, newly produced rhinovirus is excreted into the nasal mucus and may be distributed to other areas of upper respiratory mucosa. Adults seem more prone to paranasal sinus involvement, whereas young children seem more prone to otitis media during colds. The paranasal sinuses are not fully developed until about age 12, but other factors may also influence these differences. Children are not good nose blowers and thus may be less likely to spread rhinovirus into the sinuses. On the other hand, children spend more time asleep, and a horizontal position may facilitate the spread of mucus (and thus rhinovirus) into the middle ear cavity. Rhinovirus has been demonstrated in fluid obtained from the maxillary sinus/ear cavity of 40–50% of patients with acute sinusitis and otitis media (Pitkaranta et al., 1997, 1998). Multiple rhinovirus infections may cause hypertrophic adenoids (lymphatic glands in the posterior oropharynx) in children with blockage of the nasal passages, and consecutive rhinovirus infections in children without a wellness period in between may create a clinical picture simulating the chronic sinusitis seen in adults (chronic nasal discharge for more than 6 weeks).
It is very difficult to distinguish an acute viral otitis media or sinusitis from an acute bacterial otitis media or sinusitis. It is generally accepted that acute bacterial sinusitis complicates an estimated 0.5–2.2% of viral colds. The complication rate of acute bacterial otitis media following colds is not clear (Hendley, 2002). Suppurative otitis media, defined as a bulging tympanic membrane with purulent middle ear fluid or purulent otorrhea from a perforated tympanic membrane, occurs in only 2–15% of young children, but mild otitis media may occur in 40–50%. One problem may be that viruses and bacteria gain entrance to the sinus and ear cavities and are trapped without causing real mucosal invasion or infection.
In addition to the sinuses and middle ear, rhinovirus may also spread to the lower airways. Young children commonly develop bronchiolitis/reactive airway disease during rhinovirus infections (Heymann et al., 2005). The mechanism by which rhinovirus infection induces wheezing is not well understood. Adults with chronic bronchitis frequently develop exacerbation of their illness during rhinovirus infections with transient decreased pulmonary function. Rhinovirus is also an important precipitant for asthma attacks in both children and adults. The severity of cold symptoms is not greater in allergic patients with rhinovirus infection than in normal individuals, but patients with allergic rhinitis have increased airway responsiveness to histamine during rhinovirus infections.
Serious Complications Of Rhinovirus Infections
Fatal pneumonia caused by rhinovirus infection has been reported in immunocompromised patients.
Treatment
At the present time, there is no commercially available antiviral drug for treatment of rhinovirus infections. Intranasal interferon-a2b topically applied for 2 days has been shown to decrease viral titers in nasal secretions (Gwaltney, 1992). Nonprescription drug treatments to relieve symptoms are available to and often warranted by cold sufferers, but treatment measures to prevent rhinovirus infections from further development into viral otitis media, viral acute sinusitis, or bronchiolitis are not available.
Infants have the highest prevalence per year of otitis media as a result of frequent colds. Public perception that bacteria cause colds and that antibiotics are required for otitis media with colds continues to fuel the inappropriate overprescription of antibiotics for colds. Infants with colds also have the disadvantage of being obligate nose breathers. Cold remedies for infants introduce the potential for enhanced toxicity since metabolism and drug excretion vary by age and safe dosing levels have not been established in infants. Evacuation of secretions from the nasal cavity with a bulb suction device remains the best option at this point in time. Mild fever may be treated with acetaminophen for few days.
Symptomatic or supportive therapies are widely used in older children and multiple treatment choices are available. Many treatment options are based on a combination of drugs targeted at several cold symptoms at once. Parents and caregivers are unrelenting in their search for cold remedies for their children and often turn to herbal medicines (e.g., Echinacea herbal derivatives) with unknown and potentially harmful effects. It is important for clinicians to obtain detailed information about the administration of cold remedies from the caregiver when seeing a child with an upper respiratory tract infection. Unintentional dosing errors, especially in young children, can have catastrophic outcomes.
Evidence of symptomatic relief of cold in adults has been demonstrated with several drugs.
Nasal Sprays
A methacholine nasal spray can reduce the amount of nasal secretions, which often pour from the nose during the first few days of a cold (Borum et al., 1981). After 1 or 2 days, when nasal breathing becomes difficult due to the increased viscosity of the nasal secretions, a nasal decongestant spray such as oxymethazoline can relieve congestion. Topical nasal steroid sprays are not recommended for rhinovirus infection; the symptomatic benefit is limited and viral shedding is actually increased.
Oral Combination Therapies
Oral antihistamines with anticholinergic and sedative effects (first-generation antihistamines such as chlorpheniramine and brompheniramine) and oral sympathomimetics (such as pseudoephedrine hydrochloride and phenylephrine hydrochloride) have been shown to be efficacious in adults for reducing nasal congestion, cough, and sneezing during colds. Codeine and dextromethorphan are used to suppress cough, but have not been shown to be effective in controlled studies with patients with colds.
Oral Anti-inflammatory Medications
Aspirin, naproxen, and ibuprofen are effective for reducing systemic aches, headache, and sore throat. In addition, naproxen has been shown to diminish cough and ibuprofen to reduce sneezing. Oral steroids have not been shown to be beneficial for symptomatic relief in rhinovirus infection. Anti-inflammatory treatment of rhinovirus colds increases viral shedding.
Hand Sanitizers
A reduction in the frequency of rhinovirus infections might be possible through interruption of transmission, since rhinoviruses must be acquired from another person. However, the alcohol gels commonly used as hand sanitizers to prevent colds were not shown to reduce rhinovirus infections in a controlled field trial (Sandora et al., 2005). In laboratory tests, alcohol may reduce titer but does not eradicate rhinovirus. Careful hand-washing will remove rhinovirus.
Socioeconomic Impact
Although a single rhinovirus infection is generally mild and self-limited, the frequency of colds produces morbidity that is a challenge to public health officials. Colds occur at an estimated rate of one billion per year in the United States, with about 25 million patients seeking medical care for uncomplicated upper respiratory illness and 5 million for otitis media. Colds account for an estimated 22 million missed days of school and 20 million absences from work annually. It is obvious that a better understanding of the pathogenesis of rhinovirus infections and more effective treatment modalities would have a strong impact on public health.
Bibliography:
- Borum P, Olsen L, and Winther B (1981) Ipratropium nasal spray: A new treatment for rhinovirus in the common cold. American Review of Respiratory Diseases 123: 418–420.
- Greve J, Davis MG, Meyer AM, et al. (1989) The majority HRV receptor is ICAM-1. Cell 56: 839.
- Gwaltney JM Jr (1992) Combined antiviral and antimediator treatment of rhinovirus colds. Journal of Infectious Diseases 166: 776–782.
- Hendley JO (1998) Editorial comments: The host response, not the virus, causes the symptoms of the common cold. Clinical Infectious Diseases 26: 847–848.
- Hendley JO (2002) Otitis media. New England Journal of Medicine 347: 1169–1174.
- Heymann PW, Platts-Mills TA, and Johnston SL (2005) Role of viral infections, atopy and antiviral immunity in the etiology of wheezing exacerbations among children and young adults. Pediatric Infectious Disease Journal 24(supplement 11): S217–S222.
- Moody SA, Alper CM, and Doyle WJ (1998) Daily tympanometry in children during the cold season: Association of otitis media with upper respiratory tract infections. International Journal of Pediataric Otorhinolaryngology 45: 143–150.
- Pitkaranta A, Arruda E, Malmberg H, et al. (1997) Detection of rhinovirus in sinus brushings of patients with acute community acquired sinusitis by reverse transcription-PCR. Journal of Clinical Microbiology 35: 1791–1793.
- Pitkaranta A, Virolainen A, Jero J, et al. (1998) Detection of rhinovirus, respiratory syncytial virus and coronavirus infection in acute otitis media by reverse transcriptase polymerase chain reaction. Pediatrics 102: 291–295.
- Proud D, Naclerio RM, Gwaltney JM Jr, et al. (1990) Kinins are generated in nasal secretions during natural rhinovirus colds. Journal of Infectious Diseases 161: 120–123.
- Sandora TJ, Taveras EM, Shih M, et al. (2005) A randomized, controlled trial of a multifaceted intervention inducing alcohol-based hand sanitizer and hand-hygiene education to reduce illness transmission in home. Pediatrics 116: 587–594.
- Winther B, Hayden FG, Arruda E, et al. (2002) Viral respiratory infection in schoolchildren: Effects on middle ear pressure. Pediatrics 109: 826–832.
- Gwaltney JM Jr and Heinz B (2002) Rhinovirus. In: Richman DD, Whitley RJ, and Hayden FG (eds.) Clinical Virology, 2nd edn., pp. 995 –1018. Washington, DC: American Society for Microbiology Press.
- Gwaltney JM Jr (2005) The common cold. In: Mandell GC, Bennett JE, and Dolin R (eds.) Principles and Practice of infectious Diseases, 6th edn., pp. 747–758. Philadelphia, PA: Elsevier Churchill Livingstone.
- Winther B (1994) The effect on the nasal mucosa of respiratory viruses (common cold). Danish Medical Bulletin 41: 193–204.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








