This sample Smoking Cessation Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Introduction
Smoking is a global epidemic. Approximately half of all smokers will die of a smoking-related disease and 50% of these will die in middle age losing, on average, 22 years of life. If people stop smoking before the onset of smoking related illnesses they can regain a number of years lost to smoking, but stopping smoking at any time can result in health gains, reduced chance of premature death, and a reduction in the severity of disability caused by smoking. Furthermore, smoking cessation is one of the most cost-effective interventions available to health-care systems (Godfrey et al., 2005).
Most smokers want to quit and many try each year. However, most will attempt to quit on their own, and although overall many succeed, unaided quitting is associated with the lowest chance of long-term success. Not every smoker will require help in stopping, but all should be encouraged to quit and at least offered evidence-based treatments.
There is a plethora of smoking cessation treatments available to smokers, yet not all of these are efficacious. New effective treatments are being developed all the time. This means that it will become increasingly challenging for the health-care professional to stay up to date with what works best for whom. This research paper considers the various challenges facing the smoking cessation practitioner.
Harm From Tobacco Use
Smoking is one of the major public health issues of all time. By 2020 tobacco smoking will have killed more people than the number that died during the First and Second World Wars added together, and will kill more people than HIV/AIDS, other chemical dependencies, and road traffic accidents added together. In addition to the harm to public health, tobacco growing exacts huge social and environmental costs around the world. For example, vast tracts of forest have been destroyed to make way for tobacco plantations and farmers have been lured away from growing food, which in turn contributes to worldwide poverty. Tobacco users themselves spend a significant amount of their income on tobacco, sometimes prioritizing its purchase over more important needs, such as food and clothing for children.
Tobacco is manufactured, produced, and used in several forms. Smoking cigarettes is the principal method of tobacco use worldwide. Loose dried tobacco is also smoked as roll-your-own cigarettes and in pipes. Cigars make up a small proportion of tobacco products smoked. Tobacco is also produced in loose form for chewing and it is powdered for sniffing (e.g., snuff) and packed into small pouches for use in the mouth (e.g., Swedish snus). Not all tobacco types carry the same degree of risk, but it is inhaled smoke that is responsible for the majority of deaths, disease, and disability associated with tobacco use. For example, smoking directly increases the risk of cardiovascular disease (CVD), a number of cancers (including cancer of the lung, esophagus, and cervix), chronic obstructive pulmonary disease (COPD), and age-related macular degeneration. Smoking while pregnant increases the risk of miscarriage, placental abnormalities (placental abruption and placenta previa), and early-for-term births. There is a greater chance of low-birth-weight babies and increased risk of sudden infant death syndrome. As well, children exposed in utero have a higher risk of later developing respiratory illnesses, middle ear infections, and are more likely to have learning and behavioral difficulties. Some evidence suggests that children of mothers who smoked during pregnancy are predisposed to take up smoking themselves.
Smoking exacerbates and worsens the prognosis of many other illnesses, such as asthma and diabetes. Exposure to the smoke from other people’s cigarettes, that is, secondhand smoke (SHS) is also associated with an increased risk of illnesses such as lung cancer and CVD in nonsmokers.
This research paper therefore focuses on how to help people stop smoking. Many of the principles presented in this research paper, while specifically directed at cigarette smokers, can be applied to assist users of other tobacco products (and other nicotine delivery mechanisms) as well, and end their dependency on those products.
Nicotine Dependency
Despite knowing some of the many health risks of smoking, many people are unable to stop. This is primarily because of the highly addictive nature of nicotine in tobacco. However, it was not until the 1970s that there was support for the notion that nicotine was a dependence producing drug. Before this time most scientific bodies viewed smoking as merely a habit. The tobacco industry has also successfully promoted smoking as a lifestyle choice, a behavior no riskier than many other choices people make on a daily basis. The belief that people could just stop if they wanted to lingers, even among many health professionals.
Getting Hooked On Nicotine
When people first try smoking a cigarette they are not dependent and therefore are free to choose to not repeat the experience. Unfortunately, most experimentation with smoking occurs when people are still children or in early adolescence. While many young people find the experience distasteful and subsequently avoid smoking again, too many young people are swayed by powerful influences on their behavior such as smoking being perceived as the norm in their family, peer group and culture, cigarette advertising, easy access to tobacco, poorly developed social skills, and poor emotional control. For many children smoking is just one of a repertoire of behaviors they have learned and that they will adopt without question.
To understand how people become addicted to nicotine, it is necessary to understand how nicotine affects humans. Nicotine is inhaled with tobacco smoking into the lungs where it is rapidly absorbed into the circulation. It reaches the brain within seconds where it binds to and subsequently activates nicotinic acetylcholine receptors (nAChRs). These are located in many parts of the central nervous system, but those located on the dopamine neurons in the ventral tegmental area appear to be most important in nicotine dependence. Activation of nAChRs leads to an increase in dopamine in the nucleus accumbens that in turn ‘rewards’ behavior. It is this speed of nicotine delivery and action and the quick and frequent repetition of the behavior that allows smoking and the psychoactive ‘hit’ to become undeniably associated. An increase in dopamine is associated with most dependency-causing drugs and behaviors (e.g., gambling).
The Transition From Experimenting To Occasional To Regular Smoking
The first 100 cigarettes might be smoked irregularly in response to some trigger, for instance, during a social context wherein the smoker wants to elevate their mood, or conversely in reaction to some depressing trigger, such as boredom or an upsetting argument with a peer or parent. Some cigarettes will be smoked merely because others are smoking and it is offered. Each time the triggering emotion or situation – and the context in which the smoking occurred, including the people and environment – will become strongly associated with the ‘rewarding’ effects of smoking. The experimenter learns more ways in which they can use smoking, for example, to relieve stress, to induce a sense of relaxation, or to abate nervous tension during awkward social moments.
Nicotine has a relatively short half-life. Thus, to reexperience the ‘hit’ smokers must have another dose of nicotine after a relatively short period of time. The speed with which a person graduates from occasional smoking to regular daily smoking depends on age at initiation, the social restrictions that might be placed on young people smoking, access to tobacco, and prevalence of triggers. The less restrictions the faster the transition to daily smoking can be. Only about 5% of smokers do so on a casual basis and do not go on to become daily smokers.
Daily smoking initiates physical changes in the brain chemistry and eventually structure that explains nicotine dependency. Neuroadaptation in the brain establishes a greater expression of nAChRs on the cell membrane. Ceasing intake of nicotine subsequently results in the emergence of withdrawal symptoms, the severity of which has some relationship to the level of dependency.
Doses must be repeated frequently throughout the day to maintain the desired pharmacological state and avoid withdrawal symptoms. A common pattern of smoking emerges, given no restrictions on where people can smoke, whereby a smoke is had soon after waking, followed by a second and third cigarette over the next 1–2 hours. These few cigarettes help reestablish a particular blood nicotine level to which the smoker has become accustomed. Regular cigarettes throughout the day help to maintain this level. Additional ‘situational’ cigarettes are still smoked for a surge of stimulation or in reaction to the many triggers that have now been established. Each repetition reinforces the association, resulting in the contextual factors themselves sensory cues such as taste, smell, and stimulation of the respiratory tract becoming triggers to smoke.
Nicotine dependency is compounded by the potential psychoactive effects of some of the 4000 chemicals used during the tobacco manufacturing process (Hoffmann et al., 2001). Some of these chemicals, and products of combustion, may cause dependency in and of themselves. Thus, the term tobacco dependency has been promoted as a more appropriate replacement for the term nicotine dependency.
Criteria For Drug Dependence
One of the first definitions of nicotine dependence was that of the World Health Organization (WHO) in 1964. The focus was primarily on compulsive use of the drug as opposed to the dependence-producing properties of nicotine. In 1977, the Royal College of Physicians (RCP) published their report that described tobacco smoking as a drug dependence and in 1980, the American Psychiatric Association (APA) recognized that smoking met most of the criteria for drug dependence and thus tobacco dependence was included in the Diagnostic and Statistical Manual of Mental Disorders (DSM-III). In 1988, the U.S. Surgeon General issued a report titled Nicotine Addiction, which concluded that tobacco is addictive, nicotine is the substance in tobacco that is responsible for this, and that the psychopharmacology of nicotine is similar to other major drugs of addiction such as heroin and cocaine.
Measuring Dependence
The APA diagnosis of nicotine dependence requires three or more of the listed criteria to be present at any time in a 12-month period: tolerance; withdrawal; often takes in larger amounts or over longer period of time than intended; has persistent desire or unsuccessful efforts to cut down or control use; spends great deal of time in activities necessary to obtain the substance, use the substance, or recover from its effects; given up important social, occupational, or recreational activities or reduced due to substance use; continues to use despite knowledge of persistent physical or psychological problems caused by or exacerbated by the substance. Existence of these can be checked within the context of assessing a person’s smoking history.
Measuring the magnitude of dependency can help identify those smokers who would benefit from extra assistance to quit. One of the most frequently used tools for assessment of nicotine dependence is the Fagerstrom Test for Nicotine Dependence (FTND). Two items out of the six in the questionnaire (time to first cigarette in the morning and cigarette consumption) account for most of the variance predicting outcome of smoking cessation treatment. Smokers seeking treatment for helping them to stop usually have slightly higher scores.
Cigarette consumption is often used on its own to measure dependency, but it does not always correlate well with the degree of dependence because of titration. This is a smoking method used to maximize nicotine dosage per cigarette. For example, the smoker can take deeper puffs, block the vent holes on the cigarette, increase puff frequency, and smoke more of each cigarette. Titration is particularly common among lower socioeconomic smokers and in countries with widespread, smoke-free environment laws restricting places where people can smoke. To save money, smokers often switch to loose tobacco that is sometimes cheaper per gram of tobacco than tailor-made cigarettes. Loose tobacco can be hand rolled in to slimmer cigarettes and rolled in slow-burning paper to prevent wastage. Tailor-mades can be smoked a half at a time and butts can be saved for their scraps of leftover tobacco. These behaviors make it difficult to determine the number of cigarettes per day. Further, these behaviors allow the smoker to reduce their overall number of cigarettes per day without reducing their blood nicotine level at all. By smoking efficiently, smokers can cut down to about 5–6 cigarettes a day while maintaining the same blood nicotine level normally obtained by smoking a pack of 20.
Biochemical tests provide the most accurate measure of the amount of nicotine consumed. The concentration of nicotine or cotinine, a nicotine metabolite, can be measured in blood, urine, and saliva. Cotinine has a longer half-life allowing for detection of nicotine exposure over a number of days. There are simple saliva test kits that can provide a semiquantitative measurement of cotinine in saliva or urine within a few minutes. The fastest and least intrusive tool is a carbon monoxide monitor that measures the concentration of carbon monoxide in the smoker’s expired breath.
Nicotine Withdrawal Syndrome
For many smokers, it is the withdrawal symptoms that make quitting one of the hardest behavioral changes they will ever attempt to make. Nicotine withdrawal symptoms vary in severity and in how long they will go on for, and may be in part responsible (urges to smoke and depressed mood in particular) for the majority of relapses, which occur within the first month after a quit attempt.
The withdrawal syndrome (also listed in DSM-IV) emerges as blood nicotine levels drop. Reduced levels of nicotine in the brain set off a domino effect of reduced levels of acetylcholine and other neurotransmitters, such as dopamine and serotonin resulting in increasing levels of irritability, depressed mood, anxiety, poor concentration, restlessness, and sleep disturbance. Other systems within the body are also affected resulting in decreased heart rate, constipation, and mouth ulcers. Increased appetite combined with decreased metabolic rate often leads to weight gain that is a commonly cited cause of relapse to smoking.
Smokers may report urges to smoke for many weeks after stopping. These are often precipitated by smoking cues that trigger changes in neurotransmitter levels in anticipation of an influx in nicotine. The association between the cues and smoking will gradually be extinguished each time the new ex-smoker is exposed to those cues and maintains their abstinence.
A Public Health Approach To Smoking Cessation
The 3Ts Model (Figure 1) provides a conceptual framework for understanding smoking cessation (West and Sohal, 2006). Even though smoking is largely an individual behavior and the decision to stop is made at the individual level, smokers can be encouraged to quit smoking in a number of ways.
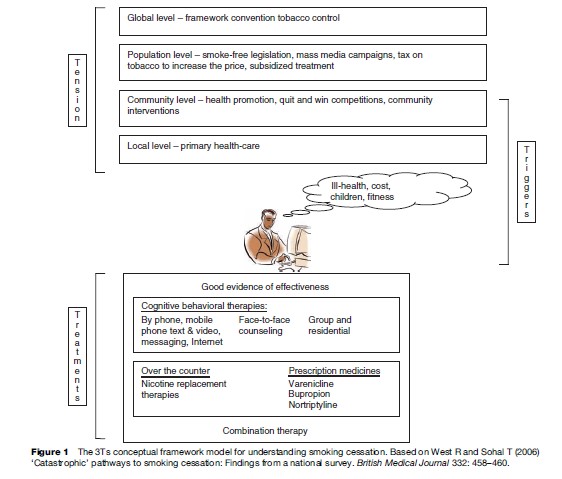
Public Health Programs
Smoking cessation is likely to be more effective if delivered as an integral component of a multifaceted country or population-level tobacco control program. While focused on reducing uptake of smoking and reducing consumption and smoking prevalence, many tobacco control program strategies can prompt smokers to think about quitting.
At a global level, the WHO has established the Framework Convention for Tobacco Control (FCTC). This is the first framework established to address a public health epidemic. Signatories to the FCTC are required to implement a minimum set of policies designed to slow the spread of the epidemic. These include measures that ban tobacco advertising and sponsorship, protect nonsmokers from secondhand smoke, eliminate smuggling of tobacco products, cigarette packet warning labels, tobacco tax increases, and product regulation (for more information about the FCTC, see the section titled ‘Relevant Websites’).
Access to smoking cessation support and effective pharmacotherapies can also be enhanced at a population level. For example, in New Zealand the government funds a national, free quitline telephone counseling service and provides heavily subsidized nicotine replacement patches or gum. In the UK, the government subsidizes all smoking cessation medications with proven efficacy.
It is much easier to stay smoke free in an environment that restricts smoking and encourages and rewards healthy lifestyles. These public health actions create tension for individual smokers who find it less socially acceptable to smoke.
The Role Of Health Promotion In Prompting Quitting
At the community level, health promotion strategies and interventions can add to the pressure to quit and provide information about how to access support. ‘Quit and Win’ competitions are one example of a community-level intervention that directly engages smokers and prompts them to make a quit attempt. Cessation programs can be promoted at the community level – for example, in the workplace to employees – or through schools to parents and teachers.
How Primary Health Care Can Promote And Support Quitting
Most smokers visit their family doctor at least once a year. Brief opportunistic advice to stop smoking, given by a doctor, consists of delivering advice during a routine consultation. Regardless of whether a smoker is seeking help regarding quitting, brief advice can significantly contribute to increasing quitting in the population, resulting in up to a 2.5% increase in long-term abstinence rates (Lancaster, 2004). Translating this effect size into the number needed to treat to get one long-term quitter equates to the provision of brief advice to 40 smokers. This is a cost-effective method that can be delivered opportunistically to large numbers of smokers. Most physicians believe that they have an important role to play, but many do not provide assistance, not even simple advice to their patients who smoke. The evidence for the effectiveness of brief advice delivered by other health-care professions is less robust, however, given the small amount of time that it takes to deliver, this should not dissuade any health-care professional from asking about smoking and then advising to stop. There are a number of memory aids to assist health-care professionals in helping their clients who smoke; the most widely known is the ‘5 As’ listed subsequently (USDHHS, 2000). More recently various groups have tried to shorten this to make it even easier to remember, for example, ‘AAR’ (Ask, Advise, and Refer) is advocated by the American Dental Hygienists’ Association, and ‘ABC’ (Ask, give Brief advice to quit, and provide or refer for Cessation support to those who want to quit), is used in the New Zealand smoking cessation guidelines.
The 5 As
- ASK – The smoking status of every adult should be identified and prominently documented in their medical record.
- ASSESS – Determine nicotine dependency and motivation to quit.
- ADVISE – At nearly every encounter, provide brief cessation messages that are clear, strong, and personalized; supportive; and nonconfrontational.
- ASSIST – Provide assistance to quit by offering self-help materials, assisting with setting a quit date and developing a quit plan; providing practical counseling and support; exploring barriers to successful cessation and strategizing solutions; referring to organized cessation support (e.g., free phone quitlines); and encouraging use of an effective pharmacotherapy.
- ARRANGE – Arrange follow-up (in person or by phone).
Triggers To Quit
The risks of smoking are generally known to many smokers in countries with good public health policies. In those countries health is likely to be the number one reason for quitting. This is not the case in developing countries where the health risks of smoking are not publicized. The benefits of quitting smoking are numerous (e.g., see section titled ‘Relevant Websites’). Smokers who stop reduce their risk of premature death as well as risk of morbidity from a wide range of smoking-related diseases. Other reasons include the cost of smoking, concern about exposing others, particularly children, to secondary smoke, wanting to set a good example for others, fitness, and longevity. The majority of smokers say they would like to give up.
Smoking Cessation Treatments: Overview
The majority of smokers decide to quit unaided, that is, without seeking external support from any formally delivered behavioral or pharmacotherapy. The most common method is stopping abruptly, often referred to as cold turkey. Some smokers may try to cut down first. Many smokers have inherent behavioral change skills or can quit using self-help resources. These three methods are discussed first.
As soon as a smoker seeks external support with their quitting they are likely to receive some form of behavioral support, which can be delivered briefly (e.g., taking no more than 5 min) or more intensively during weekly classes.
Smoking cessation is twice as likely to be achieved if the behavioral support is complemented with an effective pharmacotherapy, such as nicotine replacement therapy (NRT). (The range of effective pharmacotherapies is briefly outlined in the following section titled ‘Pharmacotherapies with Proven Efficacy.’) However, many smokers may initially try products and treatments that can be obtained at their local pharmacy or natural therapy shop, or from local providers of ‘natural’ therapies. The range of unproven ‘alternative’ therapies is immense. The most popular ones used by smokers for smoking cessation are outlined here.
Self-Help Approaches To Quitting
‘Cold Turkey’ (Abrupt Cessation Without Assistance)
The majority of smokers who decide to quit try to just stop, either by setting a quit day or impulsively stopping in reaction to some trigger. Approximately 3% of smokers who try quitting this way will achieve long-term abstinence (Raw et al., 1998).
Cutting down
Many smokers reduce their tobacco consumption as an alternative to quitting altogether, believing that by doing so they will reduce the risks to their health. Unfortunately, cutting down without quitting altogether may not result in health gain.
Cutting down is often used as a preparatory step to stopping smoking. Health-care professionals often support a reduction in consumption, especially if their patients are resistant to stopping or find it difficult to stop completely. There is evidence to suggest that cutting down prior to quitting can increase self-efficacy and prompt a quit attempt.
One of the major problems with this approach is that smokers tend to compensate for a lower quantity of cigarettes by smoking their remaining cigarettes more intensively. Therefore simply halving cigarette consumption does not imply a reduction in nicotine or exposure to the harmful components of cigarette smoke. There is also an argument that reducing cigarette consumption makes the remaining cigarettes more rewarding and therefore harder to give up completely.
Self-Help Resources
There are many books, CDs, videos, and websites designed to assist people to quit smoking. Self-help materials provide a very modest increase in long-term cessation rates over and above no help at all. Unfortunately, it may not be easy for smokers to identify resources that provide legitimate and helpful information.
Behavioral Interventions
Behavioral interventions include any cessation assistance delivered by health professionals that imparts knowledge about smoking and quitting, provides support, and teaches skills and strategies for changing behavior.
Treatment choice can vary depending on practitioners’ and smokers’ beliefs about smoking. For instance, psychoanalysts might tend to focus on the psychological reasons for smoking, particularly looking for some underlying unresolved issue. They would be interested in the circumstances surrounding the uptake of smoking and what, if any, distresses the person may have been experiencing at the time. Proponents of the biopsychosocial model try to combine treatment modalities that address the biological (physical nicotine dependency), the psychological (cognitive behavioral therapy), and the social (looking at and trying to change the environmental triggers to smoke).
One aspect that is often overlooked is a spiritual component. Some religions, such as the Mormon Church and Seventh Day Adventists, have long been providers of smoking cessation programs. Faith, prayer, and the use of traditional medicinal practices would thus be included in the mix of treatment provided.
Some approaches focus on motivation and use educational principles. Unfortunately, practitioners who minimize the strength of physical dependency on nicotine do not understand the usefulness of pharmacotherapies that effectively treat this aspect of addictive tobacco use. While cognitive behavioral and supportive approaches on their own do increase quitting success rates, combination with pharmacotherapy results in a doubling of the quit rates.
Motivational interviewing, a style of counseling, and the stages-of-change model are so commonly used in smoking cessation they are almost seen to be the way to stop smoking. These are briefly described here.
Motivational Interviewing
Motivational interviewing is a client-centered directive method for enhancing intrinsic motivation to change smoking behavior by exploring and resolving ambivalence. Health professionals using motivational interviewing usually demonstrate the principles of expressing empathy, supporting self-efficacy, rolling with resistance, and developing discrepancy for the client (for more on motivational interviewing, see section titled ‘Relevant Websites’). Motivation interacts with dependence and can guide the level of treatment that can be provided. Measurement of the degree of motivation can be useful in knowing whether to offer treatment. However, once a smoker has decided to embark on a quit attempt the degree of motivation has little bearing on the outcome of the quit attempt.
The Transtheoretical Stages-Of-Change Model
The stages-of-change model has been extensively applied to smoking cessation theory and the development of interventions. Prochaska and DiClemente’s transtheoretical model of change proposes that smokers belong to one of six stages of change: precontemplation (not ready to quit), contemplation (ambivalent about smoking), preparation (is actively planning to quit), action (enacts their quit plan), maintenance (abstains from smoking and actively avoids relapse), and relapse (has smoked one or more cigarettes and then returns to one of the above stages) (Prochaska and DiClemente, 1983).
The model has been criticized for drawing arbitrary lines delineating stages. It assumes that people have to move through each of the stages before moving to the next; however, they could move from the stage of precontemplation to action within a day. The model also ignores other important factors that influence human motivation such as plans, beliefs, wants, and urges. Perhaps more importantly there is no evidence that smoking cessation interventions that are based on this model are more effective than standard interventions.
New theories will evolve and be promoted in response to the need to find more effective smoking cessation interventions and interventions that work for all smokers, not just a select group. One such theory is the PRIME (Plans, Responses, Impulses/Inhibitions, Motives, and Evaluations) theory of motivation (see the section titled ‘Relevant websites’). PRIME incorporates insights from several established theories of behavior and seeks to account for the broader range of factors influencing addictive behaviors. In direct contrast to the stages-ofchange model, West (2006) argues that human motivation is highly responsive to the immediate situation. Thus, health professionals should attempt to trigger a desire to quit in every smoker, not just those deemed to be ‘ready.’
Quitlines
Quitlines provide brief cessation support by way of the telephone. Telephone support lines can be provided to a large number of smokers over a large geographical area. Innovative programs are being developed that deliver tailored cessation assistance via mobile phone text and video messaging, and interactive Internet programs. The greatest evidence for effectiveness of quitlines is with proactive telephone counseling, which typically involves the quitline counselors calling the client on a predefined schedule, as opposed to reactive telephone counseling that relies on the client making the calls (Stead et al., 2006).
Face-To-Face Behavioral Therapy
There is reasonable evidence that face-to-face cessation support is effective, regardless of the type of provider or the type of therapy they use (USDHHS, 2000). Face-to-face behavioral therapies can also be delivered to groups. This is usually more intensive and therefore more costly than cessation support delivered by way of telephone or within the context of a visit to the doctor. There is some evidence that suggests efficacy increases with intensity, for example, a residential program will have higher end-of-program quit rates than less intensive interventions. Other research suggests that no greater benefit is gained past eight sessions.
The body of evidence for matching smokers to specific effective treatments is small, and generally smokers should be free to choose the treatment best suited to their individual needs. The one exception to this is that more dependent smokers typically benefit from higher-dose pharmacotherapy.
Social Support
Having adequate levels of support is an important factor when stopping smoking. This may be provided by a smoking cessation specialist, other people who are stopping smoking at the same time, or family and friends. Partners of smokers also have an influence. Having a partner that smokes and living with other smokers can make it harder to succeed at quitting.
Pharmacotherapies With Proven Efficacy
Nicotine Replacement Therapy
Nicotine replacement therapy has been used to help smokers stop for over 20 years. It is safe and effective and the most widely used and available proven treatment (Silagy et al., 2004). All nicotine products provide less nicotine than the average smoker obtains from smoking. In addition, time-to-peak plasma concentration is much longer. The primary mechanism of action of NRT is to reduce the severity of withdrawal symptoms associated with smoking cessation. Although it does not completely alleviate withdrawal, NRT attenuates symptoms making a quit attempt more bearable so the smoker is more likely to succeed. There are now six NRT products available and more are in development.
The transdermal nicotine patch delivers a continuous controlled dose of nicotine by way of the skin. Adherence to treatment is generally good as the patch is easy to use, is a once-daily application, and is associated with few side effects. Usual treatment is to start with the strongest patch on cessation of smoking, then switch to the medium and finally the lowest strength patch over a course of 8–12 weeks.
The oral nicotine replacement products (gum, sublingual tablet, and lozenge) deliver nicotine by way of the oral mucosa. They allow both regular nicotine dosing and a reactive dosing to control urges to smoke and other withdrawal symptoms. More dependent smokers (e.g., those who smoke within 30 min of waking) should be advised to use the higher dose products (e.g., 4-mg gum and 4-mg lozenge). Many of the oral products may taste unpleasant to smokers initially, but they can be reassured that they will come to tolerate the taste after a short time of regular use. The sublingual tablets have the advantage of being discrete and no chewing or sucking is required.
The nicotine inhaler consists of a small plastic tube inside which is fitted a small cartridge containing nicotine. Air is sucked through the cartridge and nicotine vapor is deposited on the oral mucosa. Despite its name nicotine does not reach the lungs and it has the same pharmacokinetics as the other oral products. Some smokers prefer this product because it offers a greater degree of behavioral replacement.
Nicotine nasal spray is the fastest-acting of the NRTs. It delivers a dose of nicotine in a liquid spray to the nasal mucosa where it is absorbed, and peak plasma nicotine concentrations are reached in approximately 10 min. This product is the most aversive of all the NRTs and is the least popular product. However, it may assist some, especially highly dependent smokers. Local side effects (e.g., sore throat or runny nose) usually pass within the first few days.
Although it is generally recommended that smokers use NRT products for up to 12 weeks, some smokers go on to use them long term. The potential long-term use of a product seems to be related to its speed of nicotine delivery, but the abuse liability of NRT is generally low and smokers can be reassured that most do not require its use for more than the recommended treatment period. In any case long-term NRT use is many times safer than smoking and unlikely to carry any long-term risks.
Many smokers may have tried NRT in the past but have not managed to stop smoking. One possible reason for previous failure is that the smoker had unrealistic expectations of how NRT works (it is not like smoking, and will only make stopping smoking more bearable), did not use it correctly, or did not use it for long enough. Providing clear information on correct usage will aid adherence to treatment and increase chances of abstinence. Finally, these products are safe for the majority of smokers. It is extremely unlikely that smokers will overdose. Similarly, NRT may be used in situations in which smokers are not able to smoke, during which time many smokers will experience withdrawal symptoms (i.e., worsening of mood and cognitive performance).
Combining Products
NRT products are sometimes used in combination. For instance, different delivery mechanisms can be used together, such as the patch, which delivers a steady slow release of nicotine in to the system and gum, which would allow the ex-smoker to attend to cravings as they occur.
Trials examining the effectiveness of combining NRT products compared to single use have shown mixed results; however, overall there is a moderate advantage in using a combination of products over single-product use. Safety concerns with combining products are unfounded, and it is very unlikely that a smoker would overdose on nicotine as a result of combining NRT products.
Bupropion (Zyban)
Bupropion, an atypical antidepressant, was the first nonnicotine treatment specifically licensed for smoking cessation. The precise mechanism of action for aiding smoking cessation is not well understood, but it is thought to act by way of its ability to inhibit the neuronal reuptake of dopamine and norepinephrine (noradrenaline), both important in nicotine dependence and withdrawal. It may also have some action as a noncompetitive inhibitor of the nicotinic acetylcholine receptor, and perhaps by way of its effect on serotonin reuptake.
Bupropion is a safe treatment when used correctly, however, it cannot be used for as many people as there are contraindications to be checked before prescribing it. How bupropion interacts with other drugs also needs to be considered. The most common side effects of bupropion are insomnia and dry mouth. The medication also has a small 1 in 1000 risk of seizure, which is similar to some other antidepressants.
Nortriptyline
Nortriptyline is the only other antidepressant that has demonstrated efficacy in improving smoking cessation outcome (Hughes et al., 2007). It is a tricyclic antidepressant that inhibits the reuptake of norepinephrine (noradrenaline) and serotonin, and it is thought that it aids cessation by way of its noradrenergic mechanism thereby reducing the severity of withdrawal symptoms. An advantage of nortriptyline is that it is an inexpensive medication. However there are cautions that need to be applied when using this medication, for example, there are risks in using it for people with CVD. Contraindications need to be checked before prescribing.
Nortriptyline has a number of common side effects, for example, dry mouth, light-headedness, shakiness, and blurred vision. Urinary retention, constipation, sexual difficulties, and seizure risk are also reported.
Given that other effective medications for smoking cessation are readily available, nortriptyline is currently regarded as a second-line therapy by some smoking cessation guidelines.
Varenicline
Varenicline (Champix, Chantix) was developed specifically for smoking cessation. It is a partial nicotine acetylcholine receptor (nAChR) agonist and is highly selective for the alpha-4 beta-2 receptor. This agonist effect leads to dopamine release, but less than that seen with nicotine. It also possesses antagonist properties as it competes with nicotine for the same receptor site.
Its mode of action in aiding smoking cessation is primarily by reducing the severity of tobacco withdrawal symptoms (via its agonist effects) but it also reduces the rewarding properties of nicotine (via its antagonistic effects). The latter effect may be beneficial in extinguishing smoking behavior for the week it is used prior to quitting and helping to protect against complete relapse if a smoker lapses.
The most common side effect associated with this medication is nausea and this appears to be dose dependent. The titration period prior to quitting helps limit the occurrence of nausea. Sleep disturbance and constipation have been more frequently reported in controlled trials by those receiving varenicline compared to placebo. However, it should be noted that these symptoms are also withdrawal symptoms and are likely to occur more frequently in the varenicline group because these people are more likely to be abstinent. Most of the symptoms are reported as mild and dissipate within a few weeks.
Clonidine
Clonidine is an antihypertensive and has been used for prevention of recurrent migraine and also to treat opioid and alcohol dependence. It is an alpha-2 adrenoceptor agonist and reduces sympathetic activity by decreasing norepinephrine (noradrenaline) release. Although efficacy is comparable with that of NRT and bupropion, clonidine has undesirable side effects, such as postural hypotension, dizziness, and dry mouth. It is not routinely used as a smoking cessation aid.
Non-Nicotine Therapies Without Proven Efficacy
A number of medications have been investigated as possible smoking cessation aids but evidence of effectiveness has not been found. These include other antidepressants such as doxepin and imipramine, and selective serotonin reuptake inhibitors (SSRIs). Some monoamine oxidase inhibitors (MAOIs) show promise, but currently there is no evidence to support their use in smoking cessation. Anxiolytic drugs are not effective. There is no strong evidence for the use of the opioid antagonists naloxone and naltrexone, used in the treatment of other chemical dependencies, nor has mecamylamine, a nicotine antagonist, demonstrated any efficacy.
There are numerous other cessation treatments available worldwide. Many are herbal remedies, based upon the use of plant, animal, or mineral products. There are devices such as small cigarette packets incorporating a computerized reduction program, filters, paints, and powders that promise an aversive reaction if taken with smoking. There are pills and potions that promise to stop cravings.
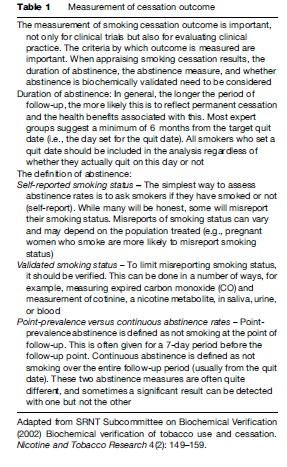
Most of the studies of these ‘alternative’ therapies are methodologically poor by today’s standard (Table 1). For example, definitions of abstinence are not provided, self-reports are not biochemically validated, studies lack adequate control groups, sample sizes are small, and follow-ups are not blind. In addition, it is difficult to blind the subjects and usually no attempt is made to minimize bias due to demand characteristics and expectations.
Cytisine
Cytisine, an alkaloid from the plant Cytisus laburnum (golden rain), is a nicotine analogue that acts as a partial nicotinic acetylcholine receptor agonist. It has a high affinity for the alpha-4 beta-2 receptor subtype, which is thought to be the main receptor that mediates the central effects of nicotine. Cytisine was introduced in several Eastern European countries as a smoking cessation medication in the late 1960s. Evidence suggests that cytisine might be useful for smoking cessation.
Glucose
It has been proposed that glucose might alleviate the urge to smoke by satisfying the need for carbohydrates and satiating appetite. It has also been investigated for its potential effect on withdrawal relief by way of a complex pathway involving serotonin, tryptophan, and insulin. On the available evidence, it is unlikely to be an effective smoking cessation agent when used on its own.
St. John’s Wort
St. John’s Wort (Hypericum perforatum L., SJW) extracts are known to have antidepressant properties and have been used for many years to treat mild to moderate depression, anxiety, and sleep disorders. The link between smoking and depression has been long recognized. There is a higher prevalence of smoking among people who have a history, or current diagnosis, of depression; smokers who are depressed find it more difficult to quit; some smokers become depressed when they stop smoking; and postcessation depression is related to relapse. To date studies have examined the use of SJW at doses up to 600 mg per day and there is no evidence that treatment helps smokers stop.
Acupuncture
There are two main acupuncture treatments for smoking cessation. The first involves needles inserted at points on the ear (e.g., lung and hunger auricular points) or on the face. Secondly, needles may be inserted into points in the ear and secured in place for 1–3 weeks. These can then be pressed whenever there is an urge to smoke. Small beads or seeds can be taped in place instead of needles. This is known as acupressure. Another variation of acupuncture uses low-level laser. Although there is no sensation on the skin, laser acupuncture is said to stimulate traditional acupuncture points in a similar way as other techniques. Current evidence does not show any benefit of acupuncture compared with sham (placebo) acupuncture in helping smokers to stop. Neither has acupuncture’s effect on withdrawal symptoms been proven.
Hypnosis
Hypnosis is one of the most widely advertised and best-known alternative treatments for smokers. It has been used by smokers for many years, and is said to work by placing the smoker in a heightened level of attention during which suggestions regarding the risks of smoking, the benefits of quitting, and the determination and commitment to stop can be imparted. The current body of evidence shows no benefit in smokers receiving hypnotherapy compared to those receiving a control intervention.
Rapid Smoking
Rapid smoking is an aversive treatment that links smoking with an unpleasant stimulus to reduce its desirability. Smoking cigarettes rapidly produces swift increases in plasma nicotine levels leading to a degree of ‘nicotine overdose’ and unpleasant symptoms such as nausea. In addition there are also irritant sensory effects of the tobacco smoke on the oral mucus membranes, throat, and airways. Although systematic reviews suggest some benefit of rapid smoking, the quality of the methodology used in some of the studies, which were state of the art at the time, do not measure up to current standards. The review concluded that rapid smoking cannot be considered a proven method, but there are sufficient indications of promise to warrant further evaluation.
Future Challenges For Smoking Cessation
Harm Reduction
Public health programs should consider how to reduce harm from smoking for smokers who remain unable to stop smoking or stop relapsing, without compromising smoking cessation, which remains the primary goal.
Who To Treat
Tobacco control resources are usually limited and strategies have to be prioritized for funding. Resources for smoking cessation come either out of the tobacco control (public health) budget, or out of primary (personal) health-care budgets, both of which are hotly contested and subject to political will. We suggest the following groups of smokers should be considered a priority for cessation assistance:
- Pregnant women – immediate health gain to baby, less pregnancy complications, and improved health for the woman.
- Parents of young children – parental smoking is increasingly linked with uptake of regular smoking among children and young people. Helping parents to quit decreases children’s exposure to secondhand smoke also.
- People suffering from smoking-related illnesses are typically harder to treat, but they have high motivation and stand to benefit immediately from quitting, improving their prognosis.
Smoking Cessation Interventions In Special Populations
Efficacy can be improved by designing cessation approaches for different cultural groups, including groups that have their own subculture, such as youth. The following section discusses the unique needs of some groups of smokers. To be relevant and attractive, cessation approaches and materials should address the unique needs and experiences of the groups. For example, pregnant women have a need to quit smoking as quickly as possible even if only for the relatively short term of the pregnancy. Religious and ethnic groups may have culturally specific beliefs and protocols that can be used to strengthen the delivery of cessation messages and techniques.
Pregnant And Breastfeeding Women
The ideal may be to get women to stop smoking for the long term but most women who stop smoking for pregnancy return to smoking after the birth of their child or when they stop breastfeeding. Because of the immediate and significant health gain to the baby and the reduction in risk for the pregnancy, all pregnant women who smoke should receive clear and consistent messages to stop smoking all together as early in the pregnancy as possible. Advice should be followed up with the offer of cessation assistance or referral to a cessation provider.
Many pregnant women quit smoking within weeks of finding out that they are pregnant. Those women that continue to smoke throughout their pregnancy are typically more nicotine dependent and may need assistance. Because of the urgency to reduce the baby’s exposure to the toxins from tobacco smoke, intensive behavioral support programs and even intermittent delivery forms of NRT should be considered.
Interventions that employ the stages-of-change model or motivational interviewing have not demonstrated efficacy. Furthermore, it seems that to be effective, interventions need to be delivered by people whose sole purpose is to help people stop smoking, as opposed to being an additional task of an already busy health-care professional.
Cessation approaches that promote a reduction in cigarette consumption as a forerunner to total abstinence are only useful when the pregnant woman is unable to quit using preferred methods and she is a heavy smoker. Any health gain to the baby from cutting down from 12 to 9 cigarettes, for example, is likely to be offset by titration.
Smoking Cessation In Secondary Care
Smoking is directly responsible for many hospital admissions and subsequent medical procedures and surgical operations. Being admitted to hospital brings people into direct contact with health-care professionals who, in theory, are in a good position to advise on giving up smoking and offer help to those who want it. For the smoker the admission might provide a teachable moment in which the consequences of smoking are directly relevant. In addition, hospitalization brings the smoker into an environment that is, increasingly, smoke free, with few smoking cues, and for some there will be less desire to smoke when feeling ill.
Preoperative Smoking Cessation
Smoking is an important risk factor for perioperative complications and so smokers have an increased risk of cardiopulmonary complications as well as being more likely to have poor wound and bone healing, as well as a greater chance of being transferred to other hospital departments and a longer length of hospital stay.
The preoperative period is an opportunity to encourage smoking cessation, not just for the immediate perioperative period but for the long term as well. The available evidence confirms that interventions aimed at assisting smokers to stop prior to surgery are effective. However, the timing of cessation appears to be important in determining the presence of postoperative complications. Stopping at least 8 weeks prior to hospitalization appears to be an optimum time period.
There is currently a lack of evidence for the efficacy of preoperative smoking cessation interventions on long-term abstinence. There is no reason to suggest that smoking cessation interventions that are effective in the general population would not be effective in this group. However, a number of factors may need to be considered: (1) those smokers with a smoking-related disease may be more dependent smokers and find it more difficult to quit; and (2) some of the smokers that do manage to stop preoperatively may have only committed to abstain for a short period of time.
Inpatients
Smoking cessation interventions have been tested in this setting and in some hospitals have been implemented as routine practice. To be effective, smoking cessation interventions (i.e., interventions aimed at helping smokers to stop as opposed to brief advice to stop) delivered within secondary care need to be more than a single one-off intervention delivered by a health-care professional with many other responsibilities. Furthermore, they need to include a number of follow-up contacts for at least a month postdischarge.
When looking at the effect of smoking cessation between smokers with different diagnoses, those with CVD seem to achieve better outcomes than those with respiratory illness. The evidence for this is weak, but it can be argued that smoking cessation for respiratory patients might be harder because of comorbidities that are more common in this group (e.g., depression, which is also a negative prognostic factor for smoking cessation) and the more chronic onset of the disease compared to the sudden onset of a myocardial infarction.
Pharmacotherapies should be provided as part of any inpatient smoking cessation intervention. Concerns have been raised regarding NRT use in smokers with CVD, mainly because of the known adverse effects of nicotine on the cardiovascular system (CVS). However, nicotine is not the only constituent of tobacco smoke that affects the CVS. Carbon monoxide, for example, contributes to a hypercoagulable state and alone has been shown to reduce exercise performance in patients with coronary artery disease. The evidence to date, along with expert opinion, suggests that any risks associated with NRT are small. NRT can be used safely in smokers with stable CVD. For those with unstable CVD who cannot stop smoking without medication NRT can be considered. It is recommended that a risk/benefit assessment be undertaken when prescribing NRT to these smokers. Such assessment will very likely point to a recommendation to use NRT.
Programs targeting parents of children who are admitted for bronchial, asthma, meningitis, pneumonia, glue ear, and the myriad of other smoking-related illnesses that affect children, generally have not been found to be effective in reducing exposures to SHS or increasing quit rates among parents.
Mental Health Service Users
Smoking prevalence is typically higher in people with mental health illness. Tobacco companies have actively targeted marginalized groups such as this, and smoking is well imbedded into the culture of many mental health institutions. Nevertheless, it cannot be overlooked that people with mental health illness suffer smoking-related disease and many do want to stop smoking. There are a number of factors that may make cessation more difficult in the group including higher levels of nicotine dependence and lower levels of social support.
It has been hypothesized that one of the reasons that people with mental health illness are more likely to smoke is that smoking may attenuate some psychiatric symptoms. However, stopping smoking does not lead to deterioration in mental health and indeed there may be improvement. There are limited data showing the effectiveness of smoking cessation treatment programs for smokers with mental health illness. The U.S. smoking cessation guidelines recommend that these people be offered those treatments that are of proven effectiveness in the general population.
Finally, a practical point, stopping smoking may alter the plasma concentrations of a number of psychiatric medications. Components of tobacco smoke are known to induce the liver enzyme cytochrome P450 1A2 that is responsible for the metabolism of a number of medications. Stopping smoking causes a slowing of metabolism of these medications and subsequently blood levels may rise. Clozapine is a drug in particular that requires monitoring following smoking cessation.
Indigenous People
There are over 320 million indigenous people living in over 70 countries and many of them have two to three times higher smoking prevalence than the colonizing population. Indigenous peoples’ beliefs about and experience with tobacco have not been the same. For example, varieties of the tobacco plant, indigenous throughout South and North America were used in different traditional ways by the indigenous peoples throughout those lands. Tobacco control goals promoting smoke-free environments, for instance, are in conflict with indigenous peoples’ goals to return to traditional tobacco use practices. The Maori of New Zealand, however, were a smoke-free people prior to colonization. Their history with tobacco has been devastating, resulting in Maori women having the highest rates of lung cancer in the world for women and at least 40% of Maori women smoking during pregnancy. Maori goals are not to merely control tobacco, but to ban it altogether from New Zealand. This desire conflicts with the ruling government’s softer tobacco control stance.
Effective promotion and delivery of effective cessation interventions to indigenous peoples are best done by the indigenous communities themselves. Indigenous peoples need to be supported to develop their capacity to respond in culturally appropriate ways to their usually disproportionately higher rates of morbidity and mortality due to tobacco use. Two by-Maori, for-Maori smoking cessation programs in New Zealand provide examples of culturally appropriate interventions. One smoking cessation program took smokers to stay on a marae (a traditional meeting place) for 7 days. The residential program followed traditional protocols, used traditional healing practices, and many activities that would be recognized as contemporary behavioral modification techniques. Another program used NRT and motivational interviewing but was delivered by Maori in a way consistent with Maori values and beliefs (Ministry of Health, 2003). For instance, nicotine dependency is understood and treated using a bio-psycho-social-spiritual (Te Whare Tapa Wha) framework that supports the use of pharmacotherapy (bio), education and skills development and motivational interviewing (psycho), content being delivered to smokers and their families (social), while respecting and practicing traditional protocols relating to (spiritual) practices, such as performing karakia (prayer) (Glover, 2005).
Cessation interventions designed by indigenous people can use appropriate language and culturally meaningful imagery and stories. Respecting indigenous peoples’ goals for self-determination and recognizing that they need to identify culturally appropriate strategies to reduce cigarette smoking is important if indigenous environments are to become smoke free.
Young People
There is good evidence that many adolescent smokers inhale cigarette smoke and show signs of nicotine dependence near the beginning of their smoking experience. Furthermore it is incorrect to think that young smokers do not want to quit. Almost half would like to stop smoking and two-thirds have tried to stop unsuccessfully.
Cessation interventions for young people need to be designed to be age-appropriate and culturally appropriate to increase the likelihood of the materials being relevant. An example of an effective peer-led program is the Florida Truth Campaign. (For more information about the Florida Truth campaign, see the section titled Relevant Websites).
There are limited data to support the efficacy and safety of NRT use in smokers under 18 years of age. Those data that are available show that there are no major safety concerns and these young smokers do want to use NRT. Furthermore there is emerging evidence for the delivery of cessation support and NRT to adolescent smokers. This suggests that it is important to make cessation services, including the provision of NRT, accessible and acceptable to adolescent smokers, especially as this group tends not to use conventional health services.
Relapse Prevention
Improvements in smoking cessation treatments have led to a general increase in abstinence rates, although these are rarely above 20–30% at one year. Given the current relapse rates following short-term smoking cessation, interventions aimed at helping people to remain abstinent over the long term are extremely important. Typically relapse prevention (RP) programs help recent ex-smokers to recognize high-risk situations and smoking triggers and teach behavioral modification and other skills, such as refusal skills to help them resolve the temptation. Other programs have used cue exposure techniques, aversive smoking, exercise, extending the duration of the treatment period, and ongoing pharmacological treatment. However, little evidence for the effectiveness of relapse prevention programs has been found (Hajek et al., 2005). Much of the evidence was constrained by a number of factors including inadequate samples size, testing of brief interventions, and focusing mainly on the traditional skills-based approach.
Smoking Cessation Training
As there is evidence that training family doctors to deliver brief advice can make a measurable difference in practice, tobacco dependence and its treatment should be included in the training of all health-care professionals. Furthermore, keeping up to date with the latest evidence of effectiveness and new smoking cessation treatments needs to be offered as part of continued professional development.
Conclusion
Smoking cessation has an important place in any tobacco control strategy. Most smokers wish to stop smoking, but they are often confronted by an array of treatments, many of which are not effective. Health-care professionals have a crucial role to play in triggering their patients who smoke to quit and in assisting them to select effective treatments. Unfortunately, health-care professionals are not immune to common misconceptions or misunderstandings of tobacco dependence and its treatment.
Evidence-based smoking cessation treatments are very cost-effective and have the potential to improve the quality of life and increase longevity of many smokers. Health-care professionals need to implement systems that ensure that advice to stop smoking is delivered to all smokers, whether they wish to stop or not. For smokers who do wish to stop smoking, assistance should be provided so that they have the best chance of stopping for the long term. Smoking cessation that combines multisession counseling with pharmacotherapy (e.g., NRT, bupropion, and varenicline) typically produces the best outcomes.
The treatment of tobacco dependence is an evolving field. To provide the best care for their patients who smoke, health-care professionals need to receive training to enable them to do this. If the global public health community is to make inroads into lowering smoking prevalence then tobacco control, which must include tobacco dependence and its treatment, need to be seen as important components of both undergraduate and postgraduate education.
Bibliography:
- Glover M (2005) Analysing smoking using Te Whare Tapa Wha. New Zealand Journal of Psychology 34(1): 13–19.
- Godfrey C, Parrott S, Coleman T, and Pound E (2005) The costeffectiveness of the English smoking treatment services: Evidence from practice. Addiction 100 (supplement 2): 70–83.
- Hajek P, Stead LF, West R, Jarvis M, and Lancaster T (2005) Relapse prevention interventions for smoking cessation. Cochrane Database of Systematic Reviews (1): Art. No.: CD003999. DOI: 10.1002/14651858.CD003999.pub2.
- Hoffmann D, Hoffmann I, and El-Bayowny (2001) The less harmful cigarette: A controversial issue. A tribute to Ernst. Wynder. Chemical Research in Toxicology 14(7): 767–790.
- Hughes JR, Stead LF, and Lancaster T (2007) Antidepressants for smoking cessation. Cochrane Database of Systematic Reviews (1): Art. No.: CD000031. DOI: 10.1002/14651858.CD000031.pub3.
- Lancaster T and Stead LF (2004) Physician advice for smoking cessation. Cochrane Database of Systematic Reviews (4): Art. No.: CD000165. DOI: 10.1002/14651858. CD000165.pub2.
- Ministry of Health (2003) Evaluation of culturally appropriate smoking cessation programme for Maori women and their whanau: Aukati Kai Paipa 2000. Wellington, New Zealand. http://www.moh.govt.nz/ moh.nsf/7004be0c19a98f8a4c25692e007bf833/50be7bea182bcb5bcc256d6c000c5408OpenDocument (accessed September 2007).
- Prochaska JO and DiClemente CC (1983) Stages and processes of self-change of smokings toward an integrative model of change. Journal of Consulting and Clinical Psychology 51(3): 390–395.
- Raw M, McNeill A, and West R (1998) Smoking cessation guidelines for health professionals. A guide to effective smoking cessation interventions for the health care system. Health Education Authority. Thorax 53 (supplement 5, Pt 1): S13.
- Silagy C, Lancaster T, Stead L, Mant D, and Fowler G (2004) Nicotine replacement therapy for smoking cessation. Cochrane Database of Systematic Reviews (3): Art. No.: CD000146. DOI: 10.1002/14651858.CD000146.pub2.
- Stead LF, Perera R, Lancaster T, et al. (2006) Telephone counselling for smoking cessation. Cochrane Database of Systematic Reviews (3): Art. No.: CD002850. DOI: 10.1002/14651858.CD002850.pub2.
- United States Department of Health Human Services (USDHHS) (2000) Treating Tobacco Use and Dependence. Rockville, MD: USDHHS, Agency for Healthcare Research Quality.
- West R (2006) Theory of Addiction. Oxford: Blackwell.
- McEwen A, Hajek P, McRobbie H, and West R (2006) Manual of Smoking Cessation: A Guide for Counsellors and Practitioners. Oxford, UK: Blackwell.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








