This sample Displaced Populations’ Health Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Introduction
Addressing the public health needs of displaced populations constitutes one of the greatest humanitarian challenges of the contemporary world. In this research paper we review evidence about the key health issues affecting displaced populations, the strengths and weaknesses of public health interventions, and strategies by which public health professionals may more effectively engage with communities and thereby promote more appropriate responses.
The importance of the problem of displacement has been recognized for more than half a century. In 1946, the opening statement of the Annex Constitution of the International Refugee Organization adopted by the United Nations General Assembly affirmed that ‘.. .genuine refugees and displaced persons constitute an urgent problem which is international in scope and character.’ (Resolution of the 67th plenary meeting, 15 December, 1946). In the years since this statement was written, the images of communities uprooted by natural disasters, civil unrest, and war have continued to proliferate and have brought global attention to the needs of displaced people. In spite of this, in many cases adequate responses to these needs are often lacking.
Displacement may occur in both developed and developing countries and may be caused by natural disaster, civil unrest, or war. In almost all cases, it exacts a heavy toll on individuals and communities and generates major social and public health problems. Often, both morbidity and mortality occur not directly from the primary events that caused the displacement but from its indirect and ongoing consequences. Displacement poses challenges to the individuals and organizations responsible for both national and global public health responses. The challenges range from the provision of food, clean water, sanitation facilities, shelter, and access to professional health care, to long-term preventive and health-promotion strategies, ultimately aimed at rebuilding communities and saving lives.
Despite good intentions, many efforts to provide assistance to displaced communities – particularly in times of natural disaster – are unsuccessful. Agencies often rush to provide quick-fix solutions to urgent, yet complex health and social needs. In many cases, this produces frustration at and disillusion with relief efforts (Silove and Zwi, 2005). Common mistakes of relief organizations include a lack of cultural, religious, and ethnic awareness; inadequate knowledge about political situations within regions; limited awareness of what other individuals, groups, or agencies may be providing; lack of consideration regarding long-term sustainability of public health and aid-based interventions; and inadequate consideration of the consequences of the departure of a donor agency or the fading of media attention (see Silove and Zwi, 2005 for discussion). Although Band Aid solutions to existing health needs may appear useful in the short term (e.g., Thomas and Thomas, 2004), there is invariably a need for intermediate and long-term public health prevention and educational strategies that are culturally appropriate, targeted to individual need, and that engage with and enable displaced communities full access to and participation in the new communities in which they find themselves.
Definitions Of Refugees And Internally Displaced Persons
One of the difficulties associated with attempts to analyze the health issues faced by displaced persons is the lack of precision with which the terms are sometimes used. This often makes collection and interpretation of data difficult and hinders assessment and comparison of programs and organizational strategies.
Refugees
The most widely accepted definition of refugee – and that which will be assumed in this research paper – is that of the United Nations, contained in the 1951 Convention on the Status of Refugees and expanded in the 1967 Protocol. This definition has been accepted by 145 countries and is the one most commonly used in international law and employed as a standard by which to compare groups. It provides a definition of a refugee and the kinds of basic rights, legal and other assistance refugees should receive. According to this Convention a refugee is someone who:
Owing to well-founded fear of being persecuted for reasons of race, religion, nationality, membership of a particular social group or political opinion, is outside the country of his nationality and is unable or, owing to such fear, is unwilling to avail himself of the protection of that country; or who, not having a nationality and being outside the country of his former habitual residence as a result of such events, is unable or, owing to such fear, is unwilling to return to it. (1951 UN Convention on the Status of Refugees and 1967 Protocol)
The term refugee specifically covers only people who have fled their homelands and sought sanctuary in other countries. The key points are:
- that refugees have to be outside of their countries of origin;
- that the reason for flight has to be a well-founded fear of persecution on the basis of race, religion, nationality, membership of particular social groups, or political opinion;
- that they have to be unwilling or unable to seek protection within their countries.
The term should not be confused with asylum seeker, economic migrant, illegal immigrant, or internally displaced people.
Internally Displaced Persons
Internally displaced persons (IDPs) are different from refugees because rather than fleeing their countries they remain within their own national borders. The United Nations High Commission for Refugees (UNHCR) Guiding Principles on Internally Displaced Persons defines IDPs as:
Persons or groups of persons who have been forced or obliged to flee or to leave their homes or places of habitual residence, in particular as a result of or in order to avoid the effects of armed conflict, situations of generalised violence, violations of human rights or natural or human-made disasters, and who have not crossed an internationally recognised State border. (UNHCR Guiding Principles on Internally Displaced Persons)
IDPs may have been forced to flee their homes for the same reasons as refugees but unlike the latter have not crossed internationally recognized borders. While many IDPs are in similar situations to refugees and face the same kinds of problems, they are not protected by international refugee law. Rather, they remain subject to the sovereignty of their own governments and consequently may not have access to international aid and services that can be made available for refugees.
The Nature And Extent Of The Problem
While many advances have been made in the way we collect and interpret statistics about the numbers of displaced people, any statistics about displaced groups should be interpreted with a note of caution. Advances, such as the collection of detailed sociodemographic information, have also been met with continued obstacles. These include how displacement is defined, operational issues in collecting data, and of course political interests. This has led to a widespread recognition that collecting data is a difficult task and that statistics should be interpreted with caution. As such, one should not base responses on the rise and/or fall of the absolute numbers of displaced people, but the complex social forces behind these statistics, basing discussions not around ‘how many?’ but ‘why?’
Refugees
The number of refugees reported globally has fluctuated significantly in the last 10 years. These fluctuations have been influenced by the occurrence of conflicts globally, the locations of these conflicts and how they are viewed by external countries. Absolute numbers are difficult to determine, in part because of the different definitions employed in different countries, resulting in different data sets and criteria for the entry and repatriation of refugees. For this reason, official statistics must often be viewed with caution and regarded as providing only crude estimates of the true rates.
By the end of 2004, the number of refugees globally was approximately 9.2 million. According to the UNHCR, the main countries of origin were Afghanistan (2 084 000), Sudan (730 600), Burundi (485 600), Democratic Republic of Congo (462 200), Somalia (389 300), Palestinians (under UN mandate only) (350 600), Vietnam (349 800), Liberia (335 500), Iraq (311 800), and Serbia and Montenegro (250 600) (UNHCR, 2005).
Interestingly these numbers suggest a net decrease of approximately 356 000 over the previous 12 months, continuing a 4-year trend of falling numbers of officially reported refugees and contributing to an overall 24% decrease in numbers between January 2001 and January 2005 (UNHCR, 2005). This may be, in part, attributed to unprecedented levels of voluntary repatriation, including the repatriation of over 3.5 million Afghans from Pakistan and the Islamic Republic of Iran from 2002 to 2005 (UNHCR, 2005).
Internally Displaced Persons
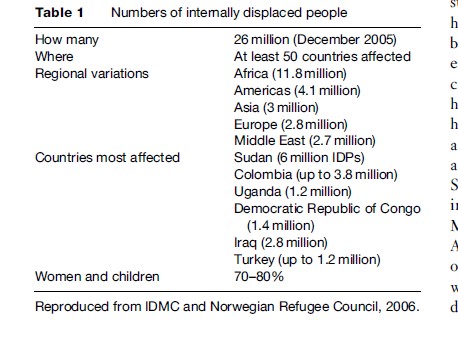
Accurate estimates of the number of IDPs are even more difficult to determine with any degree of accuracy. Official statistics may not include individuals displaced by natural disasters (e.g., the 1.2 million people left homeless after the South-Asian tsunami), and there may be political reasons for underestimating or exaggerating the numbers displaced by civil conflicts (Table 1).
Causes Of Displacement
The causes of displacement, both external and internal, are diverse and complex. Generally speaking, individuals flee when the integrity of their persons is threatened and they move toward countries or regions where they expect conditions to be better. It is useful to distinguish between the root and proximate causes of displacement. Root causes are those that initiate a conflict or disaster and displacement, while proximate causes are immediate factors that trigger people to move. For the most part, the root causes of the flight of refugees and IDPs are similar, as are the occurrences, circumstances, and experiences before fleeing from their homes. Common causes for flight or migration include persecution, violence, civil war, and other forms of armed conflict. Natural events such as earthquakes, droughts, and tsunamis and other factors related to industrialization and development, such as deforestation and pollution, also contribute. Proximate causes include exhaustion or availability of food supplies, access to shelter, outbreaks of disease, and attacks by militia groups.
Consequences Of Displacement And Impact On Health
Estimates Of Mortality
Mortality rates for displaced people are often compared with the emergency threshold, which is calculated as twice the normal mortality rate for the region. There is some evidence that displacement increases mortality rates to at least double normal baseline rates in the population before any displacement activity. The most critical phase is the emergency phase, which is when mortality is greater than one death per 10 000 people in a single day (Spiegal et al., 2002). Mortality rates for critical emergency phases (6–12 months) and postemergency phases of displacement are often poorly measured and are often based upon hospital and burial data and population estimates, all of which may be inaccurate. Mortality rates are therefore often likely to be underestimated among displaced populations. A rapid epidemiological assessment in 2004 of mortality rates in 137 000 internally displaced people (IDPs) in South Darfur, Sudan, aimed to inform relief efforts. The study occurred in three sites in South Dafur (Kass, Kalma, and Muhajiria). Mortality rates (expressed as deaths per 10 000 a day) were 3.2 in Kass, 2.0 in Kalma, and 2.3 in Muhajira. The mortality rates for children under 5 years of age were 5.9 in Kass, 3.5 in Kalma, and 1.0 in Muhajiria. The study reported that violence was reported to be responsible for 72% of deaths predominantly in younger males. However, in camps, diarrheal disease caused between 25% and 47% of deaths (Grandesso et al., 2005).
Causes of death and death rates vary between and within displaced groups. Some evidence suggests that if displaced populations remain in their new homes for sustained periods of time their mortality will level out as health patterns stabilize and health-care needs become better identified and more satisfactorily addressed. However, it is also possible that some displaced populations continue to have higher rates of mortality and poorer health outcomes as compared with individuals from the host communities (Hargreaves et al., 2004). Hargreaves and colleagues, in their study of Mozambican refugees and their hosts in a rural subdistrict in the northeast of South Africa, showed that while there were no differences in infant mortality between children from former Mozambican refugee households and those from South African homes (adjusted (for changes in mortality rate over the study period) rate ratio, 1.02), mortality levels were higher among former Mozambican refugee children during the next 4 years (adjusted rate ratio, 1.91). Within the Mozambican group, those refugee children residing in refugee settlements had higher mortality rates than those residing in more established villages both in the first year (adjusted rate ratio, 1.50), and next 4 years of life (adjusted rate ratio, 1.34). These disparities in findings emphasize the need for continued surveillance and health monitoring to ascertain changes in the health status of displaced populations over time.
Health Risks
A variety of factors can make displaced people susceptible to health risks. For many displaced people, movement merely means a shift from one poor and vulnerable situation into another similar one. Because not every forced flight satisfies the legal criteria defined by international law, inequities in access to humanitarian relief and protection for internally displaced people may result. In addition, inaccurate estimates of the expected duration of displacement may also lead to delays in the provision of aid or to its absence altogether.
The vulnerability of displaced persons can be categorized according to specific stages or phases of the process of displacement: Namely preflight, during flight, and postflight. While each displaced person’s flight experience is unique, there are common features between the experiences of different groups (e.g., Thomas and Thomas, 2004; Grove and Zwi, 2006).
It is important to recognize that the people who are forced to leave their homes, whether as a result of conflicts or natural disasters, are more often than not the poorest, most marginalized members of society, as a result of which prior to displacement they invariably had preexisting unmet health needs. Many have lived in conditions of poverty with inadequate nutrition and housing and limited access to education and health services. Preventive health measures such as vaccination against infectious diseases may have been especially lacking. Their health status may therefore already have been compromised before the onset of flight. Such factors need to be taken into account when considering the potential impact on the health-care services of the country or region of destination and the design and management of subsequent health and social interventions. Health and social interventions should not only aim to address those health problems that may result from displacement, but should also consider those health needs that existed prior to displacement. An assessment of these needs may lead to a reprioritization of public health interventions or a refocusing of strategies to assess and address needs.
Preflight Health Issues
The preflight phase refers to the period prior to flight from homes, communities, and countries. For those fleeing conditions of conflict, the most common health problems may be those associated with violence. A study of unaccompanied asylum-seeking children in the United Kingdom reported that their preflight experiences often included the death or persecution of family members, persecution, forced recruitment, and trafficking (Thomas et al., 2004).
Health Issues During Flight
People who flee directly before or soon after conflict situations and natural disasters often leave their homes on short notice with little time for planning. For many displaced people, fleeing from the settings in which they have lived all their lives is itself a difficult, turbulent, and uncertain process. Grove and Zwi comment:
The journeys of refugees from home to final destination may include multiple border crossings, arduous land journeys, and protracted stays in formal or informal camps. They are typically marked by ongoing fear of violence and persecution: from militants, from authorities in the host country, from those who control the camps and from other refugees. Those charged with protecting such refugees may abuse their role: United Nations peacekeepers, NGO workers, and local camp staff may exploit vulnerabilities, demanding sex, for example, in exchange for access to basic supplies. (Grove and Zwi, 2006: 1932)
The process of displacement can itself lead to health related difficulties, particularly for vulnerable groups such as the infirm, children, women, and the elderly. Health risks associated with flight commonly include a lack of basic necessities required to sustain life or health such as food, shelter, water, emergency health care, and adequate sanitary conditions (e.g., Thomas and Thomas, 2004).
Postflight Health Risks
People adversely affected by the displacement process and those with existing health conditions are most vulnerable to difficulties after arrival at their destinations. All displaced persons need basic housing, food, water, and sanitation. The extent to which these needs can be met, let alone specific needs arising out of their particular experiences or as a result of different cultures or religions, are determined largely by the nature and capacity of the receiving state, province, or country. It should also be noted here that the places that refugees and IDPs flee to may not be developed in a traditionally westernized sense and therefore may not be ready or prepared to deal with a sudden influx of people. Therefore, in these circumstances, additional complications arise, as discussed in the section titled ‘Specific health needs of displaced persons.’ This is particularly problematic for IDPs, as they would not routinely have access to aid and support services that may be available in other countries for international refugees.
In a systematic review of the pre and post displacement factors affecting the mental health of refugees and displaced peoples, Porter and Haslam (2005) reported that materially secure conditions, indexed by economic opportunities and permanent private accommodation, are associated with good mental health or were moderators of mental ill health. Psychopathology reflected contextual factors that could be significantly reduced by generous material support on the part of governments and agencies in the new country of residence.
Specific Health Needs Of Displaced Persons
While evidence about specific rates of disease or illness in displaced peoples remains limited, there is a vast collective knowledge obtained by health workers and relief organizations concerning the nature and scope of the health needs of displaced persons. Several key areas require consideration, including infectious diseases and other acute physical illnesses, chronic illnesses, and mental and reproductive health problems.
Infectious Diseases And Other Acute Physical Illnesses
Infectious Disease
Infectious diseases, such as malaria, parasitic infections, HIV, hepatitis A, B, and C, and tuberculosis, are among the main causes of disability and death of displaced persons. The public health implications of these conditions are often difficult to address, both in developed and developing countries.
Infectious diseases are particularly prevalent among displaced populations because of the physical conditions in which they find themselves as a result of the conflict or other adverse events that precipitated their flight and a frequent lack of basic health knowledge and education. Displaced persons living in camps are at particularly high risk because of a lack of basic health necessities such as housing and shelter, food, availability of adequate supplies or quality of water, sanitation and hygiene, immunization and personnel with experience in acute or preventive health care or first aid.
A further compounding factor is that these conditions often occur together or in parallel with one another and may lead to a heavy disease burden and increased mortality in particularly vulnerable groups, such as women, infants, and children. If the duration of conflict or displacement is prolonged, additional problems may arise associated with the collapse of social and health-care structures and deterioration in environmental conditions. Such conditions place individuals at a much greater risk of persistent, emerging, and re-emerging infectious diseases, malnutrition, and war-related injuries, further shaping the disease profile of poverty.
The environmental conditions that follow natural disasters also increase the risk of infectious diseases in displaced populations. In the acute phase after the event, skin and respiratory infections and diarrhea are particularly prevalent, while a month or so later water and foodborne diseases tend to appear.
Other Acute Health Risks
In addition to infectious diseases, nutritional deficiencies are common among displaced populations, especially deficiencies in iron (causing anemia), vitamin A (ophthalmological damage and blindness), vitamin C (scurvy), niacin or tryptophan deficiency (pellagra), and thiamine (beriberi). The risk of physical injuries and the effects of violence, exposure to poisons and envenomation (such as insect bites), and dental health problems are also greatly increased.
Chronic Diseases
Refugees experience a wide range of chronic illnesses, such as hypertension, heart disease, and diabetes, in proportions similar to the rest of the community (Harris and Telfer, 2001). Nonetheless, these largely preventable and treatable conditions are often exacerbated by malnutrition and may be complicated by psychological factors. In certain settings – for example, among asylum seekers kept in detention centers – this may be further compounded by continuing, sometimes prolonged lack of access to primary health care, which causes additional delays in access to much-needed treatment.
Mental Health Problems
Displaced people are at high risk of developing mental health problems during each of the preflight, flight, and postflight phases of displacement. Research into the mental health of refugees has traditionally focused on the psychological implications of trauma, and in particular on posttraumatic stress disorder (PTSD) as a reaction to violence or torture. In addition to this last condition, the most common psychological reactions to displacement are depression (as a reaction to loss), somatization, and existential dilemmas (where belief patterns have been challenged) (Thomas and Thomas, 2004). Evidence suggests that although in most cases mental health symptoms improve over time, in a minority they remain significant over the long term (Steel et al., 2002). In their study of Australian Vietnamese refugees, Steel and colleagues’ (2002) reported that after 5 years, the frequency of mental illness was the same in those who reported one to two traumatic events and those who reported no trauma. Whilst the frequency of mental illness also progressively decreased over time for those who reported three or more traumatic events, this group had an increased risk of mental illness.
Some investigations of culturally specific sequelae such as social isolation, adjustment, and acculturation have shown that not all refugees and IDPs present with symptoms of psychiatric distress immediately on arrival in their new homes. Instead, psychiatric distress may present days, weeks, months, or even years after flight. While researchers have tended to focus on PTSD as the major mental health problem among displaced populations, evidence now suggests that public health interventions should focus equally on other common mental disorders such as depression (Komesaroff and Sundram, 2006). As discussed in the section titled ‘Public Health Responses,’ it is important that mental health programs take into account other public health issues such as nutrition, employment, and education.
Reproductive Health Issues
Reproductive health concerns the effects of social and sexual relationships and behavior on health. In the last decade, it has been recognized that conflict and displacement have a major impact on reproductive health needs. Specific reproductive health issues during situations of insecurity may include sexual violence, increased fertility rates and obstetric risk of pregnancies close together, unsafe abortions, increased spread of sexually transmissible diseases, including HIV, lack of access to health-care facilities, and increased sexual risk-taking behaviors.
The key guiding principle of the Interagency Field Manual on Reproductive Health (1999) states that:
Reproductive health care should be available in all situations and be based on the needs and expressed demands of refugees, particularly women, with full respect for the various religious and ethical values and cultural backgrounds of the refugees while also conforming with universally recognised international human rights. (UNHCR, 1999: 1)
Reproductive health services for displaced populations must take into account sociocultural, religious, and political contexts as well as the diverse and intimate nature of reproductive beliefs and practices (Bartlett et al., 2004). In some contexts, this is a long process that can only be developed with community involvement and consultation, in which communities themselves develop and implement processes for change. In general, only limited data are available concerning the reproductive health of displaced peoples. Accordingly, this is an area in which there is a pressing need for more research and collaboration with communities.
Public Health Responses
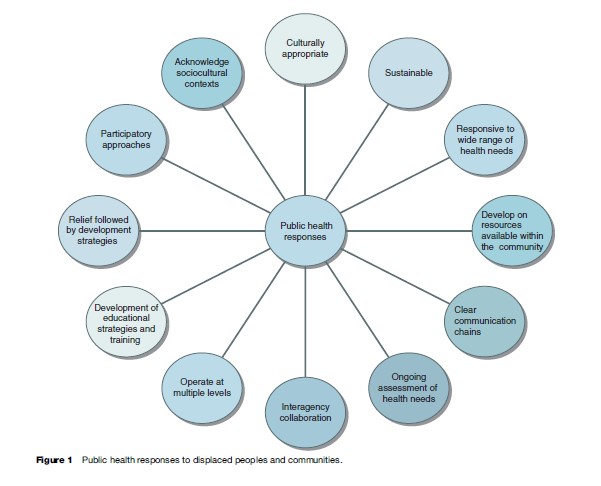
Governments have an obligation to protect and improve the health of all their citizens. National and international responsibilities to protect vulnerable people or groups from persecution are widely accepted. The need for health services within national settings to address ‘issues of access, acceptability, responsiveness and availability of services to refugees .. .’ is increasingly acknowledged (Grove and Zwi, 2006). In the case of displaced persons, collective, intersectoral action involving health professionals, nongovernmental organizations, governments, UN agencies, philanthropic funders, and most importantly the displaced communities themselves, conducted in a culturally sensitive way, will ensure sustainable and effective responses to health needs.
The health needs of displaced people are complex, diverse, and multifaceted and are complicated by severe constraints on access to basic health services and on decision making about health, health care, and well being. It is important that public health interventions are developed through close communication with the affected communities themselves in a manner that is culturally appropriate (including sensitivity to religious beliefs) and responsive to specific needs. They must also be based on participatory approaches and genuine community engagement in order to foster expanding collaborations and sustainable programs ultimately under local control.
Figure 1 summarizes the factors that should be taken into account in the planning and delivery of public health services to displaced people. This section reviews some key concepts in developing public health responses to the health needs of displaced people.
Relief Followed By Development: Building Sustainable Solutions
The needs of displaced communities for health-care programs is not limited to the acute, emergency phases surrounding displacement. As mentioned in the section titled ‘Postflight health risks,’ many long-term needs persist after the immediate period of conflict or disaster has subsided. For example, a recent report of five epidemiological surveys in the Democratic Republic of Congo has shown that despite the restoration of peace, mortality rates had either failed to improve at all or had actually worsened and that access to basic health-care services remained seriously limited.
Releasing Community Capacity: Capacity Building And Participatory Approaches
Programs devised to respond to the health needs of displaced communities should be sustainable after the emergency phase has subsided. Because health needs change over time, public health initiatives also need to evolve and adapt, subject to available resources. There are two stages in the formation and development of such sustainable solutions: Capacity building (perhaps better regarded as the fostering and development of existing capacity – or releasing community capacity) and participatory approaches.
Capacity building has been described as, ‘the cornerstone of reconstruction and development programs’ (Silove and Zwi, 2005). However, building capacity is dependent upon well-designed participatory approaches, whereby health professionals and communities share, learn, and communicate with one another. Komesaroff and Sundram (2006) state that the needs of communities during times of disaster vary greatly according to cultural, economic, and geographical conditions, and the most effective way to determine these needs is through community consultation. Collaborative community partnerships must underpin public health responses to displaced groups.
The incorporation of participatory approaches is recognized as a key element of effective long-term health-care planning for displaced communities. Displaced populations should be directly involved in the planning and delivery of services and programs to facilitate wide participation and a sense of ownership by those individuals who will be directly affected by interventions. The process of engaging communities in discussion and problem solving about their own health issues may not be straightforward. However, effective community participation makes possible the development of programs in conjunction with existing resources and capacity that are sensitive to the cultural needs of specific populations.
Collaborative efforts among health-care agencies, professionals, and communities also enhance the quality of decisions, facilitate identification of areas of greatest need, foster open dialogue about culturally sensitive issues, contribute to a sense of community ownership over the process, build trust and rapport between the community and health professions, and ultimately improve the long-term sustainability of the interventions. The long-term benefits of cooperation therefore clearly justify it over both the short and long terms.
Ongoing Assessment And Responsiveness To Wide Range Of Health Needs
The provision of comprehensive, enduring public health responses to meet the needs of displaced communities presents a significant challenge. Enduring programs must make provision for ongoing assessments of the needs of displaced communities rather than single episodes of screening. In addition to the traditional focus on infectious disease, immunization, and trauma-related mental health problems, there is an ongoing need for other types of health-care delivery. Most notably, these include reproductive health services, injury prevention, and dental health services. Because communities differ widely and circumstances, including the availability of resources, programs must remain flexible and be able to evolve over time.
Although there are overlaps, there are also major differences in the issues facing health-care providers between developed countries and developing countries. Nonetheless, in both cases, engaging the community and establishing links with local services will help to build platforms for further assessment of need. For example, Komesaroff and Sundram (2006) discuss the case identification of the second wave of psychiatric problems, including grief reactions, major depression, substance use disorders, phobic and anxiety disorder, and trauma responses, after the South-Asian tsunami. They propose a multitiered approach using and facilitating local community-based capacity, which includes community awareness programs, education of community workers (such as teachers), and the training of primary healthcare workers and medical staff to oversee treatment. They also acknowledge that limiting psychiatric morbidity will only occur if initiatives addressing other public health needs, such as nutrition, education, employment, and social reconstruction, are undertaken. Long-term health and social surveillance programs will help monitor the long-term effects of displacement and the effectiveness and efficacy of interventions.
Conclusion
The public health problems raised by displacement are complex and diverse. The exact scale of these problems is uncertain because of variable definitions and data quality. However, it is clear that, at the present time, the numbers of refugees and internally displaced persons are in the tens of millions. There is conclusive evidence that displaced populations are exposed to greatly increased health risks and suffer increased death rates. Health problems vary according to circumstances, including the causes and duration, of displacements and the preexisting health status of displaced persons. Infectious diseases, psychological trauma, physical injuries, nutritional deficiencies, and various chronic conditions and reproductive health issues are, however, common. Vulnerable populations, such as those with preexisting health conditions, women, children, and the elderly, are especially at risk.
Effective responses to these problems may be impeded because of the difficult physical settings of the displaced populations, lack of resources, and cultural and political factors. It is important for health workers to communicate closely with the members of displaced communities to identify their needs and to develop programs that are appropriate to their needs, including cultural and religious sensitivities. The provision of adequate housing, sanitation, and nutrition must be linked with educational and capacity-building strategies. Direct participation of displaced persons in the development and management of health-care programs is essential if sustainable, long-term outcomes are to be achieved.
Bibliography:
- Bartlett LA, Purdin S, and McGinn T (2004) Forced migrants – Turning rights into reproductive health. Lancet 363(9402): 76–77.
- Grandesso F, Sanderson F, Kruijt J, Koene T, and Brown V (2005) Mortality and malnutrition among populations living in South Darfur, Sudan: Results of 3 surveys, September 2004. Journal of the American Medical Association 293(12): 1490–1494.
- Erratum in: Journal of the American Medical Association 293(18): 2212.
- Grove NJ and Zwi AB (2006) Our health and theirs: Forced migration, othering, and public health. Social Science and Medicine 62(8): 1931–1942.
- Hargreaves JR, Collinson MA, Kahn K, Clark SJ, and Tollman SM (2004) Childhood mortality among former Mozambican refugees and their hosts in rural South Africa. International Journal of Epidemiology 33(6): 1271–1278.
- Harris MF and Telfer B (2001) The health needs of asylum seekers living in the community. Medical Journal of Australia 175(11–12): 589–592.
- Internal Displacement Monitoring Centre (2006) Internal Displacement: Global Overview of Trends and Developments in 2005. Geneva, Switzerland: Norweigan Refugee Council.
- Komesaroff PA and Sundram S (2006) Challenges of post-tsunami reconstruction in Sri Lanka: Health care aid and the Health Alliance. Medical Journal of Australia 184(1): 23–26.
- Porter M and Haslam N (2005) Predisplacement and postdisplacement factors associated with mental health of refugees and internally displaced persons: A meta-analysis. Journal of the American Medical Association 294: 602–612.
- Silove D and Zwi AB (2005) Translating compassion into psychosocial aid after the tsunami. Lancet 365(9456): 269–271.
- Spiegal P, Sheik M, Gotway-Crawford C, and Salama P (2002) Health programmes and policies associated with decreased mortality in displaced people in postemergency phase camps: a retrospective study. Lancet 360: 1927–1934.
- Steel Z, Silove D, Phan T, and Bauman A (2002) Long-term effect of psychological trauma on the mental health of Vietnamese refugees resettled in Australia: A population based study. Lancet 360: 1056–1062.
- Thomas SL and Thomas SD (2004) Displacement and Health. British Medical Bulletin 69: 115–127.
- Thomas S, Thomas S, Nafees B, and Bhugra D (2004) ‘I was running away from death’ – The pre-flight experiences of unaccompanied asylum seeking children in the UK. Child Care Health and Development 30(2): 113–122.
- UNHCR (1999) Reproductive Health in Refugee Situations. An Interagency Field Manual. Geneva, Switzerland: UNHCR.
- UNHCR (2005) 2004 Global Refugee Trends. Geneva, Switzerland: UNHCR Division of Operational Support.
- http://www.msf.org – Me´ decins sans Frontie` res (Doctors Without Borders).
- http://www.unhcr.ch – UNHCR United Nations Refugee Agency. Address by United Nations Secretary-General Kofi Annan as delivered to the 51st session of the Executive Committee of the High Commissioner for Refugees, held at the Palais des Nations on 2 October 2000; resolution of the 67th plenary meeting, 15 December, 1946; discussion of these different types of refugee groups.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








