This sample Military Health Issues Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Introduction
This research paper is organized into three sections: (1) military occupational infrastructure and health hazard issues surrounding military service during peacetime or garrison (at home) duty, (2) health hazard issues pertaining to mobilization and deployment, and (3) longer-term health issues. Content areas will draw primarily from U.S. military preventive medicine experiences, but it is recognized that a number of the issues and experiences are common within the international military communities.
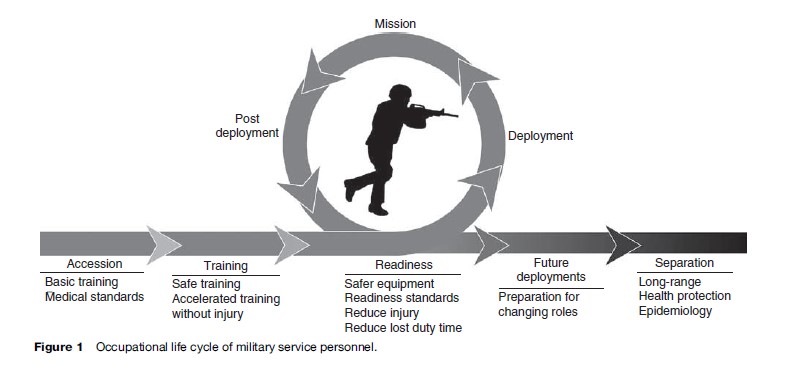
Over 2 million individuals are serving as active duty, Reserves, or National Guard members in the U.S. Armed Forces. For some, military service is a job held for only several years; for others, it is a career. As an occupation, military service is two-tiered; individuals perform duties in their respective occupational fields (e.g., as a nurse, mechanic, or truck driver), but they also respond in time of war, emergencies, or for humanitarian missions when required. Military occupational and environmental health encompasses the life cycle of military personnel, from the time of entry (accession) into the service, throughout training and readiness phases, over specific and potential multiple missions and deployment cycles, as well as when attending to long-range health and disease prevention needs (Figure 1).
In general, the multidisciplinary approach and principles of civilian occupational health that recognize, diagnose, treat, prevent, and control work-related diseases, injuries, and other conditions are applicable in the military environment. Moreover, occupational health management of military personnel in the United States adheres to methodological procedures of recognized civilian occupational health programs that manage health hazards assessment, industrial hygiene, and prevention and safety. However, due to its two-tiered status, there are a number of factors unique to military service that distinguishes it from the civilian occupational and environmental health experience. The identification of these factors and their impact on the occupational and environmental health of military personnel is the focus of this research paper.
Environmental And Occupational Health Hazard Issues Surrounding Military Service During Peacetime Or Garrison Duty
As a population, military personnel in the United States tend to be younger than the U.S. working population and maintain a higher level of health and physical fitness due to combat readiness and training requirements. Additionally, screening and elimination of individuals deemed unfit for service selects a distinctive population. For example, in 1995, during the period of initial entry and first six months of military service, the primary medical and disease reasons for disqualification of individuals were hearing-related, lower extremity orthopedic problems, asthma, and psychiatric problems (Kelley, 2003: 153). Because of these differences, those serving in the military can be considered a special group of workers with particular experiences, just as the occupational and environmental health issues of agricultural workers, construction groups, and health-care workers are sometimes addressed as selected groups (Levy and Wegman, 2000).
Although the population is distinctive, to a large extent, military jobs closely resemble or are the same as civilian jobs. Research efforts in 2000–01 determined that 72% of the total U.S. Army enlisted population was employed in a job with a corresponding civilian job title; similar results were observed in officers (both warrant and commissioned combined) (Sulsky, 2003). The overlap is significant in those jobs involving transportation and material moving, construction and extraction, and business and financial operations. Jobs categorized as involving installation, maintenance, and repair were more common in the Army than in the civilian workforce, while broad occupational groups inclusive of production and food preparation were more common in the civilian workforce.
Military Service Characteristics
In other countries (and earlier in U.S. history when a draft was in operation), certain entry-level requirements were not always in place and military service was considered mandatory for all at a certain age. In the United States under the volunteer system, there exist levels of initial screening and selection processes at accession and during initial enlistment stages in terms of medical and psychological health, physical performance standards, weight and body fat standards, aptitude determinations, and the requirements to maintain optimal readiness (in terms of health and ability to perform job tasks). From accession into the U.S. military services, occupational and environmental health programs and initiatives are in place. These include standard assessments of initial physical fitness levels and administration of appropriate immunizations; attention to the levels of attrition due to medical conditions; prevention, management, and treatment of training-related injuries (such as stress fractures) during entry training. Prevention programs are also in place to monitor exertional heat illnesses, screening and management of mental and behavioral health issues, eating disorders, weight management, and smoking cessation.
These requirements exist within infrastructures unique to the various military organizations and have an effect on outcomes of occupational and environmental programs. Military infrastructure is strongly hierarchical and execution at command level impacts program results: leadership responsibility and accountability play prominent roles. For example, in the Israeli Army, a case of heat illness is considered a court martial offense for the unit leader, and not for the individual heat casualty (Pandolf and Burr, 2001: 37).
Additionally it is important to note that in the United States and in other countries as well, some members of the military may be serving on a part-time basis (in the Reserves and National Guard) while holding a civilian job. Most commonly, these individuals work a full-time civilian job and then spend one weekend every month and 2 weeks a year performing their military job duties. At other times, they may be called up for ‘active duty service’ and deployed for peacekeeping, humanitarian, combat, or stabilization missions around the world. They also can be called to serve in an emergency response capacity at state or national levels, for example, to help evacuate civilians and provide medical assistance, as was the case during Hurricane Katrina, or to perform clean-up operations after the destruction at the World Trade Center in New York City and the Pentagon following the events of September 11, 2001, or to provide extra security during large public events, such as occurred at the 2002 Winter Olympics in Salt Lake City, UT.
Military Occupations: Training And Advancement
In peacetime and during the duty rotation when stationed at the unit’s home base (in garrison), classroom training and simulated training exercises and drills are conducted to maintain combat readiness. These training exercises are generally distinct from those designed to further develop job skills within one’s designated occupational field. These training exercises may be carried out under extreme environmental conditions of hot and cold climates in desert and mountain terrains and require high levels of physical workload. They may also involve simulated combat or peacekeeping scenarios to provide opportunities for learning and practicing new skills as well as maintenance of cohesion of group-level operational roles.
Achievement of training goals as well as maintenance of health and physical fitness standards are intimately related to continued advancement in the military structure. Target weight standards and physical fitness levels, job advancement skill sets, combined with training requirements tailored to military occupations are an integral part of military service personnel’s responsibilities throughout their service and are important determinants of advancement within the profession.
Occupational And Environmental Health Hazard Issues Pertaining To Mobilization And Deployment
Each mission and deployment scenario presents its own set of risks and hazards, not all of which are predictable. Certain missions may present with more obvious hazards (such as combat deployment). However, peacekeeping, humanitarian, training, and stabilization and/or rebuilding missions each may pose unique hazards.
One of the major challenges to military occupational health is that to a large degree, specific hazards and health issues during mobilization and deployment are inevitable because their occurrence cannot be avoided. Also, optimal exposure prevention tactics (removal from the area) cannot always be practiced and the continual weighing of the threats from multiple combinations of risks on human health and lives necessitates trade-offs in terms of focusing on the more adverse medical threats. The goal of military operational research efforts is to better understand these risks (alone or in combinations) to enable better preparation for and prevention of these risks and to develop and test proactive protection procedures.
Within the U.S. military, particularly since the 1991 Persian Gulf War, risk management system processes have been continually tested and reworked to best provide commanders with methods to evaluate and act on risks presented by operational hazards during deployment or specific missions (including a framework for management of occupational and environmental hazards). The operational risk management system outlines a process for identifying, assessing, and controlling risks, and includes a mechanism of evaluating the effectiveness of the control measures put in place.
In general, preventive medicine personnel are responsible for carrying out the process of identifying the occupational and environmental hazards, assessing the level of medical or health threat associated with the hazards, characterizing the associated risks of the threat(s) and the proposed control action(s), and then transmitting the risk assessment information and recommended control measure options to the commander. Preventive medicine personnel also are instrumental in implementing the control action(s) decided upon by the commander, evaluating the effectiveness of the action in controlling the threat(s), and documenting follow-up reassessments of the action and lessons learned for future deployments.
Within the U.S. military’s hierarchy of occupational and environmental chemical hazards, those that contribute to health and medical threats require evaluation (TG230, 2003: 18–23), but by definition, they may represent different levels of importance to the military operation at hand. A health threat is one that can cause negative health effects to the individual serviceman or woman. For example, hereditary conditions that present in adulthood, individual exposure to industrial chemicals, other injuries or conditions, or physical and psychological traumas that affect an individual but not the whole unit are considered health threats. Medical threats are more severe and have the potential to adversely affect unit or mission accomplishment or effectiveness. In the broadest sense, medical threats include all ongoing potential enemy actions, environmental conditions, disease conditions, and nonbattle injuries that degrade unit effectiveness. Military exposure guidelines and an outline of the U.S. Armed Forces approach to operational risk management are given in several technical guides (TG 230, 2003; TG 248, 2001). Applying a risk matrix, which evaluates the probability of exposure combined with the hazard severity ranking, provides an estimate of the risk level associated with the hazard of concern.
Exposure to occupational and environmental hazards during deployment situations may be transient or of limited duration but might be present at very high levels that could impact individual health and/or the mission. Other scenarios may involve lower levels of exposure but be continuous and possibly put military personnel at higher risk for possibly delayed or longer-term health problems. Thus, the frequency, intensity, and duration of the exposure(s) are evaluated when estimating the level of risk. Environmental monitoring results from the deployment area of operation are used to make the determination of the hazard severity by making a comparison of the detected military exposure levels to guidelines and standards (e.g., TG 230, 2003; TG230D, 2003; TG 248, 2001).
Occupational And Environmental Health Hazards
There are three classes of military occupational and environmental health hazards that have the potential to cause injury, illness, disease, adverse health conditions, or death and thus may be considered health and/or medical threats.
- Chemical hazards include contaminants in the air, water, soil, and food as well as exposures to industrial chemicals such as lead, solvents, pesticides, and chemical warfare agents.
- Physical hazards include climate conditions such as excessive heat and cold and physical environmental concerns such as operating at high altitudes and under conditions with high noise levels.
- Situational hazards may include physical threats (accidents, explosions), traumatic events (witnessing combat events), operational demands (high physical work demands, restricted sleep, limited food and water intake, prophylactic medications), and environmental living conditions.
Obviously, such situational threats as armed enemies present grave risks and often require the highest priority. Although certainly important in their ability to cause severe medical threats during deployment operations, infectious disease vectors, biological and nuclear warfare agents, and parasitic/entomological concerns are not described in this section.
Chemical Hazards
Over the years and with each conflict, environmental exposures to chemical hazards have occurred. A variety of different classes of chemical hazards present in a deployment or mission-specific environment have the potential to cause both acute and chronic health problems.
Chemical Warfare Agents
There is evidence that mustard gas (blistering agent) was present during World War I and the Iran–Iraq war in the mid-1980s. During the 1991 Persian Gulf deployment, potential exposure to low levels of sarin and cyclosarin either from the bombing of storage facilities or the destruction of stored munitions at Khamisiyah, Iraq, were described, although there were no documented reports of measured exposure or evidence of acute medical threats from these agents. Depending on the chemical warfare agent type, each has the capability to cause severe morbidity and mortality. Low-level exposures to these agents and related potential heath effects are not well characterized. Agents such as sarin and cyclosarin operate with similar toxic mechanisms to those of the organophosphate pesticide class, and therefore lower-level exposures have been hypothesized to result in central and peripheral nervous system symptoms in humans. Differences in specific brain tissue volumes and neurobehavioral functioning several years following the 1991 Persian Gulf deployment have been found to be associated with estimated exposure levels to sarin and cyclosarin (based on modeling efforts) (Heaton et al., 2007; Proctor et al., 2006).
Combustion Products
The potential for exposure to petroleum combustion products is widespread during deployment due to the many transportation vehicles, aircraft, and ships that operate on diesel, gasoline, and jet fuel. Also, during the 1991 Persian Gulf deployment, exposure to these combustion products occurred when oil wells were set on fire and burned for a number of months casting black smoke and particulate matter throughout the area of operation and when unvented tent heaters were used in enclosed areas.
Depleted Uranium
Both a heavy metal and source of radiation, depleted uranium is what remains after the more radioactive isotopes U234 and U235 are removed from uranium ore to make enriched uranium for nuclear reactor fuel. It is used as both armor on tanks and in certain munitions because of its ability to pierce or penetrate armor made with less dense metals. It was first used on a large scale during the 1991 Persian Gulf deployment. Depleted uranium may enter the body through inhalation, after combustion and aerosolization from explosive impact, or as a piece of shrapnel. Its primary target of toxicity is considered to be the kidney.
Solvents
During deployment missions, as within garrison occupational settings, and depending on military occupation, exposures to solvents such as jet fuel, degreasing agents, CARC paints, and decontamination solutions can be commonplace. Exposure to solvents has been found to result in increased health risks and symptoms, particularly to the central and peripheral nervous systems.
Pesticides
DEET, permethrin, and organophosphate pesticides are routinely used when U.S. military personnel deploy to more tropical regions in which mosquito or other insectborne diseases are endemic. While these compounds are used to help prevent diseases that have the potential to disrupt mission operations, they also may produce significant central and peripheral nervous system symptoms when exposure occurs at high doses or at chronic, lower-level exposures.
During the Vietnam War, the U.S. military sprayed herbicides from United States and South Vietnamese military transport planes to defoliate large areas of jungle during the war. These spraying missions started in 1962 (with Agent Purple) and continued for the next 9 years with different combinations of chemicals, including Agent Orange. Each combination of these herbicides contained the long-lived contaminant 2,3,7,8-tetrachlorodibenzopara-dioxin (TCDD), which has been associated with chloroacne and other more severe health problems, including certain cancers.
Physical Hazards
Noise
In the current deployment environment (as well as during routine training exercises), hazardous noise levels are pervasive due to machinery and firepower. Hearing loss is one of the most prevalent health outcomes associated with military service. As a result, hearing protection devices are issued to all service personnel and U.S. Army standards require these devices be worn during training practice when steady-state noise is above 85 dB or when impulse noise exceeds 140 dBP sound pressure level. In an actual combat setting, hearing protective devices may not be feasible except when firing weapons outside the immediate zone of fighting or during transportation in tracked wheeled personnel carriers, trucks, helicopters, or other aircraft.
Harsh Environments (Extreme Heat, Cold, And High Altitudes)
Military personnel continue to be deployed to locations in which the physical environment and climates may present health hazards, such as areas with extreme heat (e.g., South-West Asia) or cold weather and high altitudes (e.g., Afghanistan).
Mission requirements may require cold exposure and certain military occupational experiences may be exacerbated. For example, personnel handling petroleum products may be exposed to a high risk of frostbite as these substances remain liquid at very low temperatures ( 17.7 C [0 F]) and may cause immediate freezing of skin and mucous membranes on contact or reduce the insulation factor associated with clothing layers if allowed to saturate uniform material(s). Also, cold weather may modulate with the exposure risks associated with nuclear, biological, and chemical warfare agents as well as affecting the performance of mission duties due to requirements of wearing chemical or environmental protective gear.
Extreme heat effects such as exertional heat illnesses (EHI) result from the combination of environmental and behavioral or mission-specific factors, namely ambient air temperature, air motion or ventilation, relative humidity, radiant temperature, amount of metabolic heat being produced (physical workload), and degree of insulation and water permeability permitted within clothing or equipment worn (Pandolf and Burr, 2001: 6). The latter two factors are largely driven by physical workloads of mission requirements and the necessity and degree of protective equipment worn. For example, during the 1991 Persian Gulf deployment, while U.S. military personnel were operating in a hot desert environment, they periodically were required to wear chemical protective clothing, that is, mission-oriented protective posture, level 4 (MOPP4) gear.
In addition to EHI, cold freezing (such as frostbite) and nonfreezing injuries, and hypobaric hypoxia at high altitudes operating in these extreme environments, may adversely influence cognitive functioning, with negative effects on mission accomplishments (Pandolf and Burr, 2002: 734–735).
Situational Hazards
The potential combination of multiple hazardous experiences during a deployment or mission also raises the risk of adverse consequences. For example, it would be anticipated that military personnel will be confronted with operational occupational scenarios during deployment that include high levels of witnessing of traumatic events and may be required to function on little sleep, with inadequate hydration, in adverse environments (hot, cold, altitude, etc.), while carrying heavy loads of gear and wearing protective gear (such as MOPP4 gear).
Physical Threats (Accidents, Explosions)
Vehicle and other transportation accidents due to both battle and nonbattle related events are common causes of injury and death during deployment missions. The occurrence of improvised explosive devices (IEDs), suicide bombers, mines, and rocket-propelled grenades, in addition to the full complement of more traditional artillery, rocket, and mortar rounds have been prevalent in recent deployment missions. The ensuing pressure waves induced by these explosions have the potential to produce severe health effects on particular body organs, even without obvious embedding of shards of metal or other debris.
Although newer battlefield measures have improved war-zone survival, the success in preventing fatalities has produced higher rates of injuries that impact the healthcare delivery systems assigned to handle these adverse physical and mental health consequences.
Traumatic Events
During deployment missions, military service personnel may be exposed to highly stressful and life-threatening experiences. These may include injury from violence, traumatic loss, or witnessing death and suffering of unit members or civilian populations. Depending on circumstances during the exposure event and period of recovery, development of acute psychological and somatic symptoms and/or longer-lasting mental health consequences such as posttraumatic stress disorder (PTSD), anxiety, or depression may result.
Operational Demands
During most deployment missions there are periods of time when the operational tempo (optempo) is increased. At these times, military personnel may be expected to carry out their duties and responsibilities under circumstances involving increased physical work demands, at critical cognitive performance levels, and with restricted sleep, and/or limited nutrient and water levels. Depending on the situation, they may also be taking medications (e.g., caffeine or benzodiazepines to combat jet lag; pyridostigmine bromide as a nerve agent pretreatment, or atropine as a chemical agent antidote) or wearing additional chemical protective clothing (e.g., MOPP gear).
Living Conditions
To maintain and support operational forces during a deployment, supplies of sufficient and adequate drinking and bathing water are necessary. Also, adequate wastewater controls, food sanitation, ambient air quality, and field sanitation management and monitoring are required. Upon entry into a military field setting, it is largely the role of the environmental science or (public) health officer and other environmental health military personnel to establish water supply and sanitation systems and monitor health and environmental quality indicators that might indicate a breakdown between environmental health and sanitation, such as disease and health symptom outbreaks, food preparation irregularities, changes in potable water quality, and individual use of personal protective measures (e.g., insect repellents, appropriate clothing, adequate hydration).
In some deployment situations, maintenance of sanitary living conditions is not possible or is disrupted due to mission threats. In addition to the expected health hazards that might occur due to poor or inadequate human waste disposal, unsanitary food preparation conditions, or diminished potable water availability, research efforts indicate that a malevolent living environment during a deployment situation (defined as difficult living conditions and distress related to daily life, perhaps in an unfamiliar culture or extreme climate) was associated with greater vulnerability to stress reactions among Vietnam veterans (King et al., 1998) and related to other mental health outcomes (as described by Litz et al., 1997 relative to the Somalia peacekeeping mission).
Role Of Risk And Resilience Factors
Not everyone who experiences occupational and environmental health hazards during deployment experiences acute or lasting health problems, even if the exposure circumstances are the same for all individuals. There are other factors that must contribute to the outcomes. Although not precisely known, these factors may include preexisting demographic characteristics or health status, degree of training and readiness preparation for potential experiences, and aspects of the postexposure deployment and recovery environment. In the PTSD literature, these factors are termed risk and resilience factors: risk factors are those that are associated with increased risk of PTSD or adverse health outcomes; resilience factors are those associated with a decrease in or absence of adverse health consequences.
Research efforts since the Vietnam War have recognized that the level of social support, in the form of both personal relationships and from leader support and unit-level cohesion, is a strong predictive factor of PTSD and other mental health symptoms, both when present at the time of the warzone experience and during periods of recovery.
Longer-Term Health Issues
Postdeployment Health And Injury Issues
Upon return home from the 1991 Persian Gulf deployment, a number of U.S. servicemen and women, as well as Canadian, Australian, French, and Danish cohorts, reported an increased rate of symptoms and adverse health problems. Considerable research and clinical care initiatives have been focused on whether the experiences or events during the 1991 deployment may have led to a unique syndrome of illness. Among most clinical and research circles, the current conclusion is that modern wars throughout history have been associated with syndromes of unexplained health symptoms and these postdeployment symptoms are most likely a response to a combination of the physical and psychological factors inherent in the war environment.
Studies have been undertaken to historically review individual medical records of persons serving in all major conflicts since the mid-nineteenth century, specifically since the Boer War ( Jones et al., 2002) and the U.S. Civil War (Hyams et al., 1996). Results suggest that common symptoms of fatigue, headaches, difficulty concentrating, rapid heart rate, shortness of breath, and increased gastrointestinal distress were present after almost every conflict. Analyses by Jones and colleagues (2002) suggest a pattern to the clustering of these symptom groups that was related to the era of the conflict. That is, they have identified three types of somewhat overlapping postwar syndromes or symptom clusters, each being more prevalent during a particular period of history. Persons returning from wars prior to 1918 reported symptoms termed as a debility syndrome consisting of fatigue, weakness, shortness of breath, and difficulty completing tasks, with few psychological or cognitive symptoms. Somatic complaints that primarily focused on cardiac functioning, such as rapid heart rate, shortness of breath, fatigue, and dizziness were reported primarily by those serving in World War I. Neuropsychological and psychological symptoms, such as fatigue, headaches, depression, difficulty sleeping, and difficulty completing tasks, were more frequently associated with serving in World War II and the 1991 Persian Gulf deployment.
A single cause of these seemingly unexplained illnesses has not been identified. That these overlapping postwar subjective health symptoms were present following multiple wars and among different populations suggests that these are not new or unique syndromes. Moreover, not all returning deployed service members report these debilitating clusters of symptoms. It may be that the health symptoms or illnesses reflect an individual’s psychological stress reaction to particular events during a war while, for others, the symptoms may be related to a particular environmental experience, or may be related to a combination of circumstances dependent on the nature of the deployment.
Since the diagnosis of PTSD was clinically identified and defined, after the Vietnam War, mental health outcome consequences of war have become increasingly better recognized. More recent research and clinical efforts have addressed the incidence and prevalence of these debilitating disorders in post-2001 Iraq and Afghanistan conflicts and are also tracking their longer-term impacts on health-care utilization and functional outcomes such as absenteeism (Hoge et al., 2007). Postwar motor vehicle and other accident rates have been observed to increase among subgroups of returning servicemen and women, but appear to fluctuate over time.
Each deployment operation and mission presents unique as well as similar inherent hazards that military personnel encounter. As summarized above, for each conflict throughout history, postwar health symptoms have been reported but they do not always present with the same cluster of symptoms, most likely because not all operational environments present the same set of hazards and not everyone deployed will be exposed to them in the same manner or degree. For example, when comparing the operational environment during the 1991 Persian Gulf deployment with that of the Operation Iraqi Freedom (OIF) conflict, major differences are obvious despite the fact that both operations occurred in the same region of the world. The actual ground war during the 1991 Persian Gulf deployment lasted less than one week, while the OIF conflict exceeds four years. It is anticipated that observed postwar health and injury consequences will be different than those posed by the 1991 Persian Gulf deployment.
Long-Term Health
Several recent epidemiological studies provide evidence that those serving in the military in general or during a certain era may be at increased risk for certain diseases later in life. This includes an increased risk of amyotrophic lateral sclerosis (ALS) in persons serving in the 1991 Persian Gulf deployment (Horner et al., 2003) or military service in general (Weisskopf et al., 2004). Other studies have identified associations between PTSD and cardiovascular disease among a group of older military veterans (Kubzansky et al., 2007). Research also suggests that type 2 diabetes, selected cancers (non-Hodgkin’s lymphoma, soft tissue sarcoma, multiple myeloma), and such birth defects as spina bifida (among offspring of those exposed) are associated with Agent Orange exposure during the Vietnam War.
Prospective research and increased health monitoring and surveillance initiatives put in place in the United States (and a number of other countries including Canada, the United Kingdom, and Australia) since the 1991 Persian Gulf deployment, within both the Department of Defense and Department of Veterans’ Affairs, are providing mechanisms to better track the health of military personnel over the life cycle (Figure 1). Similar to the U.S. Department of Health and Human Services, Centers for Disease Control and Prevention Morbidity and Mortality Weekly Report, the Army Medical Surveillance Activity publishes the Medical Surveillance Monthly Report (MSMR), which summarizes trends in disease and illness outbreaks, field and case reports, and summaries of current pre and postdeployment health surveillance statistics across the U.S. Armed Forces. An ongoing research effort to track the health status of over 100 000 U.S. military servicemen and women over a 22-year period (see the section ‘Relevant websites’) will also help to provide better understanding of the long-term health consequences of particular military occupational and environmental experiences.
Bibliography:
- Heaton KJ, Palumbo CL, Proctor SP, Killiany R, Yurgelun-Todd D, and White RF (2007) Quantitative magnetic resonance brain imaging in U.S. army veterans of the 1991 Gulf War potentially exposed to sarin and cyclosarin. Neurotoxicology 28: 761–769.
- Hoge CW, Terhakopian A, Castro CA, Messer SC, and Engel CC (2007) Association of posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq War veterans. American Journal of Psychiatry 164: 150–153.
- Horner RD, Kamins KG, Feussner JR, et al. (2003) Occurrence of amyotrophic lateral sclerosis among Gulf War veterans. Neurology 61: 742–749.
- Hyams KC, Wignall S, and Roswell R (1996) War syndromes and their evaluation: From the U.S. Civil War to the Persian Gulf War. Annals of Internal Medicine 125: 398–405.
- Jones E, Hodgins-Vermaas R, McCartney H, et al. (2002) Post-combat syndromes from the Boer War to the Gulf War: A cluster analysis of their nature and attribution. British Medical Journal 324: 1–7.
- Kubzansky LD, Koenen KC, Spiro A, Vokonas PS, and Sparrow D (2007) Prospective study of posttraumatic stress disorder symptoms and coronary heart disease in the Normative Aging Study. Archives of General Psychiatry 64: 109–116.
- Kelley PW (ed.) (2003) Textbook of Military Medicine. Military Preventive Medicine: Mobilization and Deployment vol. 1. Washington, DC: U.S. Department of the Army, Office of The Surgeon General, Borden Institute.
- King LA, King DW, Fairbank JA, Keane TM, and Adams GA (1998) Resilience-recovery factors in post-traumatic stress disorder among female and male Vietnam veterans: Hardiness, post-war social support, and additional stressful life events. Journal of Personality and Social Psychology 74: 420–434.
- Levy BS and Wegman DH (eds.) (2000) Occupational Health: Recognizing and Preventing Work-Related Disease and Injury. 4th edn. Philadelphia, PA: Lippincott Williams & Wilkins.
- Litz BT, King LA, King DW, Orsillo SM, and Friedman MJ (1997) Warriors as peacekeepers: Features of the Somalia experience and PTSD. Journal of Consulting and Clinical Psychology 65: 1001–1010.
- Pandolf KB and Burr RE (eds.) (2001) Textbook of Military Medicine. Medical Aspects of Harsh Environments vol. 1. Washington, DC: U.S. Department of the Army, Office of the Surgeon General, Borden Institute.
- Pandolf KB and Burr RE (eds.) (2002) Textbook of Military Medicine. Medical Aspects of Harsh Environments vol. 2. Washington, DC: U.S. Department of the Army, Office of the Surgeon General, Borden Institute.
- Proctor SP, Heaton KJ, Heeren T, and White RF (2006) Effects of sarin and cyclosarin exposure during the 1991 Gulf War on neurobehavioral functioning in U.S. Army veterans. Neurotoxicology 27: 931–939.
- Sulsky SI (2003) On occupational health and safety research in the U.S. Army: Comparability with civilian employee cohorts. Journal of Occupational and Environmental Medicine 45: 220–221.
- USACHPPM Technical Guide 230 Chemical Exposure Guidelines for Deployed Military Personnel (TG230); version 1.3 – updated May 2003 with January 2004 Addendum.
- USACHPPM Reference Document (RD) 230, A Companion Document to USACHPPM TG 230 (TG230D); version 1.3 – updated May 2003.
- USACHPPM Technical Guide 248 Guide for Deployed Military Personnel on Health Risk Management (TG248); August 2001.
- Weisskopf MG, O’Reilly EJ, McCullough ML, et al. (2004) Prospective study of military service and mortality form amyotrophic lateral sclerosis. Neurology 64: 32–37.
- Committee on Gulf War and Health (2003) Gulf War and Health, Volume 2: Insecticides and Solvents. Literature Review of Pesticides and Solvents. Washington, DC: National Academies Press.
- Committee on Gulf War and Health (2005) Gulf War and Health, Volume 3: Fuels, Combustion Products, and Propellants. Literature Review of Selected Environmental Particulates, Pollutants, and Synthetic Chemical Compounds. Washington, DC: National Academies Press.
- Committee on Gulf War and Health (2006) Gulf War and Health, Volume 4: Health Effects of Serving in the Gulf War. A Review of the Medical Literature Relative to the Gulf War Veterans Health. Washington, DC: National Academies Press.
- Deeter DP and Gaydos JC (eds.) (1993) Textbook of Military Medicine. Occupational Health: The Soldier and the Industrial Base. Washington, DC: U.S. Department of the Army, Office of the Surgeon General, Borden Institute.
- DeKoning BL (ed.) (2007) Textbook of Military Medicine. Recruit Medicine. Washington, DC: U.S. Department of the Army, Office of the Surgeon General, Borden Institute.
- Fulco CE, Liverman CT, and Sox HC (eds.) (2000) Gulf War and Health, Volume 1: Depleted Uranium, Pyridostigmine Bromide, Sarin, Vaccines. Committee on Health Effects Associated with Exposures During the Gulf War, Division of Health Promotion and Disease Prevention. Washington, DC: National Academies Press.
- Mitchell AE, Sivitz LB, and Black RE (eds.) (2007) Gulf War and Health, Volume 5: Infectious Diseases. Committee on Gulf War, Health: Infectious, Diseases. Washington, DC: National Academies Press.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








