This sample Surveillance of Disease Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Historical Development
In civil society, police and security systems are alert to abnormal incidents that may cause hazards in communities, nations, and perhaps the world. The information discovered and assembled by this system is transmitted to an authority responsible for setting up measures to eliminate the cause of hazard. The human body provides immunological surveillance, the body’s defenses that recognize foreign materials or malignant cells; thus surveillance information helps the body’s immunological mechanism destroy such foreign materials or cells.
In the early twentieth century, information gathering on infectious diseases and other hazards to humans was developed in parallel with the development of microbiological technology and epidemiology. The data thus collected were analyzed and the results were distributed to systems and individuals responsible for control actions. Epidemiological surveillance was the beginning of a new era of infectious disease control. In recent years, surveillance activities have been expanded from infectious diseases to chronic diseases and automobile accidents and other injuries; in addition, long-term data collection such as vital statistics and surveillance of health-related social or economic activities have been surveyed systematically. In this research paper, we discuss surveillance systems and activities on which public health control action is based.
Around the mid-twentieth century when infectious diseases were a major problem and menace to public health, two medical experts attempted to set up surveillance as an essential component of public health practice. Alexander Langmuir, from the Centers for Disease Control and Prevention (CDC), developed systematic surveillance mechanisms for infectious diseases and associated control programs. In 1963, he outlined surveillance as: (1) systematic and active collection of pertinent data of target disease (s); (2) assessment and practical report of these data; and (3) the timely dispatch of such reports to individuals responsible for formulation of action plans. It is important to note that surveillance would not be useful unless data are known and acted upon by individuals responsible for initiating action plans. A surveillance system, in principle, does not include the control measures within its system. A surveillance system is better if it is independent from the control system, because experience has shown that on some occasions, disease prevalence was artificially modified by individuals who were responsible for control measures and sought to gain seemingly better results than what was actually occurring. In the 1960s, Karel Raska, Communicable Disease Division at the World Health Organization (WHO) headquarters, further expanded the system’s definition, including epidemiological research in surveillance activities. He promoted a surveillance study, for example by strengthening smallpox surveillance and approving special research funds to the newly intensified eradication program in 1967; malaria surveillance was intensified when the effectiveness of malaria control was demonstrated with investigation of malaria prevalence rates in patients using or not using mosquito nets.
In the area of public health practice, we may need to rethink the boundary of surveillance systems. It may be wise not to expand it to a broad investigation or epidemiological research, which certainly interests many researchers or health officers but does not lead to practical public health action to reduce immediate hazard or risk. Thus, the surveillance tool as a public health action may be further refined and solidified.
The latest challenge in surveillance has been in terrorism, exemplified when a terrorist group attacked facilities in the United States, Spain, and England in recent years. Anthrax was also used as a bioweapon in the United States. Surveillance against bioterrorism with smallpox virus, Bacillus anthracis, and other agents is now being developed in the West.
Surveillance Methods
Target Disease
The target diseases for surveillance are key to defining the sensitivity, specificity, effectiveness, and efficiency of the systems used. Fever and rash diseases such as measles and chickenpox or neurologic diseases such as poliomyelitis or meningococcal meningitis may be discovered or suspected readily by surveillance and allied workers: Such reportable diseases require clinical and laboratory confirmation by experienced workers. Certain principles underlie identification of target diseases.
Usually surveillance systems aim at a particular disease or only a limited number of diseases. Those who work for surveillance should have clear ideas of clinical pictures, mode of transmission and its infectivity. Further, it is advisable to know probable frequency or prevalence of such diseases and if possible, the inhabitants attitudes’ to the diseases. It is important to note that some populations may feel it is necessary to conceal the patient’s presence in the family. On the other hand, populations may be pleased to collaborate with surveillance, willingly reporting the target diseases. Sometimes, the target disease can be reported to surveillance workers only as symptoms, such as jaundice (for hepatitis B), acute flaccid paralysis (poliomyelitis), and confirmation can be made after reporting.
The Surveillance System
The surveillance system usually is set up as a distinct section or organization within the national or regional health service system and has an independent function as described in the previous section. The method or function may consist of the two main functions discussed in the next sections.
Community-Based Surveillance
The main reporters are villagers or town inhabitants or health workers in a dispensary or private clinic contacting or seeing the patients with the target diseases. It is important that there be a public relations campaign through radio, television, the press, etc. to encourage reporting the disease to the nearest health center or some designated office, which will transmit the report to the supervisory level, as shown in Figure 1.
Hospital-Based Surveillance
The main reporters in this system are hospital physicians who diagnose the diseases. This system functions in parallel with community-based surveillance, but is also important in finding rare diseases or diseases that are difficult to identify by the public because of their rare occurrence and/or because the clinical manifestation is difficult to recognize. The advantage of this system is that if hospitals are fully cooperative, surveillance coverage is good. The hospital may need to assign a physician to take responsibility for such reporting. Needless to say, the hospital administration should be fully informed and understand the importance of such surveillance.
Nosocomial or hospital-induced, infection is a special surveillance target within hospitals to be handled by a special hospital committee. The hospital administration should be aware of the occurrence of nosocomial infections and work to develop its control.
Passive or Active Surveillance
Both community and hospital-based surveillance systems are in principle passive. If the health service controlling the surveillance report urgently needs a special report, it can organize active surveillance in which special teams are formed to make house-to-house or hospital-to-hospital visits to determine the occurrence of the disease either through direct communication with community members or hospital personnel and seeing the patients or examining the hospital records or the patients on location.
Special Surveillance
Effective surveillance requires innovative ideas to augment its sensitivity.
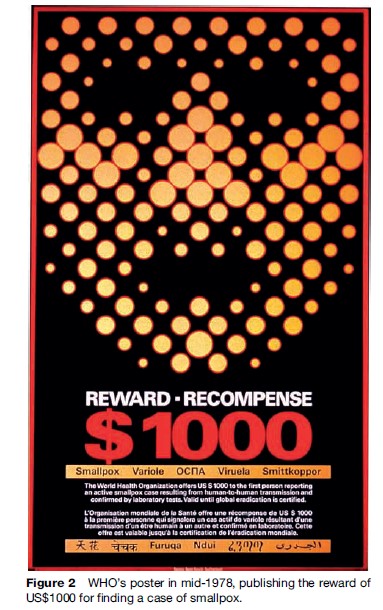
Rewards
Surveillance efficacy often depends on the public’s interest in reporting the disease. Reward is, in certain circumstances, a useful method for a health service to express the importance of reporting to the public. For example, a reward system was utilized to encourage reporting in many countries such as India and Somalia during the smallpox eradication program (1967–80). In 1978, when a probable world last case was discovered in Africa, WHO encouraged people or medical personnel throughout the world to report (Figure 2). The announcement was followed by many smallpox reports from West Africa, Indonesia, even Heathrow and Kennedy airports. All such reports were investigated by the WHO team with negative results.
Nil Report
Surveillance certainly receives positive reports of the target diseases, but often it is also important to receive nil reports indicating positive assurance that the disease did not occur during a particular time period such as a week. In other words, regular nil reports indicate that sensitive surveillance is continuing. The nil report is useful to see the situation of specifically suspected areas of occurrence such as influenza that may become pandemic or a dangerous pathogen requiring immediate action for public health measures in high-risk areas.
Measures To Handle Incomplete Surveillance Reports
Incomplete surveillance reports include mistaken reports due to the incompetence of technical personnel, active concealment of disease occurrence, or the combination of these two causes. Although these look like anecdotal episodes or events during surveillance, they often considerably influence the success or failure of control measures, which require high-quality surveillance data.
Particularly if such incomplete surveillance reports are made intentionally by health authorities, the results may become disastrous. Examples include the smallpox epidemic in the Horn of Africa during the last phase of the global smallpox eradication program in 1976–77, and the early phase of epidemics of severe acute respiratory syndrome (SARS) in East Asia, which subsequently formed a pandemic on other continents. How should such incomplete surveillance reports be treated? No standard remedy has been found so far. There have been trial and error attempts such as practical dialogue, development of collaborative research, political pressure and recommendation from a higher authority, and emphasis on moral obligation. Experience has shown that such incomplete surveillance reports from health services in the area or nation concerned often cause disastrous results that end in failing to control the epidemics thus incorrectly reported.
Laboratory Diagnosis And Surveillance System
Surveillance requires the collaboration of laboratories to confirm the diagnosis if initial reports are based on clinical diagnosis alone. Laboratory diagnostic measures may not be needed in some instances. For example, if there is a large number of cases with similar clinical manifestations, laboratory testing of only cases that are representative of the outbreaks may be satisfactory, provided that missing the correct diagnosis of other cases does not pose significant risk in developing control measures. This may be applicable to determining containment of outbreaks with vaccination in the case of measles outbreaks, a hepatitis A outbreak, etc.
The interval between the time the specimen is taken and the time when laboratory results are available to the surveillance office should be carefully determined, depending on the type of specimen testing such as serology, isolation, and specific tests such as strain differentiation. The reliability of the testing technique should always be assured with periodic assessment of the laboratory technique and testing the suitability of reagents by a reference laboratory.
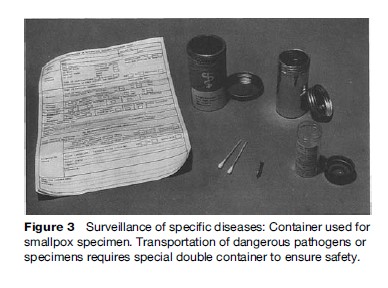
For surveillance of specific diseases such as poliomyelitis, measles, or influenza, international reference laboratories have been designated by WHO. In addition, national reference laboratories can be set up for collaboration by the individual government as the need arises. Figure 3 shows the special collection kits that were used for safe and easy handling of specimens during the WHO smallpox eradication program (1967–80). Some nations that do not have the appropriate laboratory facilities may be assisted by nearby reference laboratories, often through an arrangement with WHO. Safe measures for transportation of infectious specimens and infectious substance label are shown in Figure 4.
Collation Of Surveillance Data By Time, Place, And Person
Surveillance data collected and confirmed for its accuracy may be sorted by three major elements throughout the process at peripheral and central levels.
Time
Specimen collection date and patient dates reflecting information such as date of occurrence, course of clinical picture, etc. are necessary. Standard tabulation includes case serial number and deaths by week number 1 to 51 or 52. Monthly or daily records are also used, but weekly records are convenient, since the WHO Weekly Epidemiological Record (WER) and the US CDC Morbidity and Mortality Weekly Report (MMWR), etc. use week number for easy reference. Usually, the date of occurrence of the disease is the important date. The date of receipt of the report at health services is recorded to indicate the efficacy of the reporting system in some geographical areas.
Place
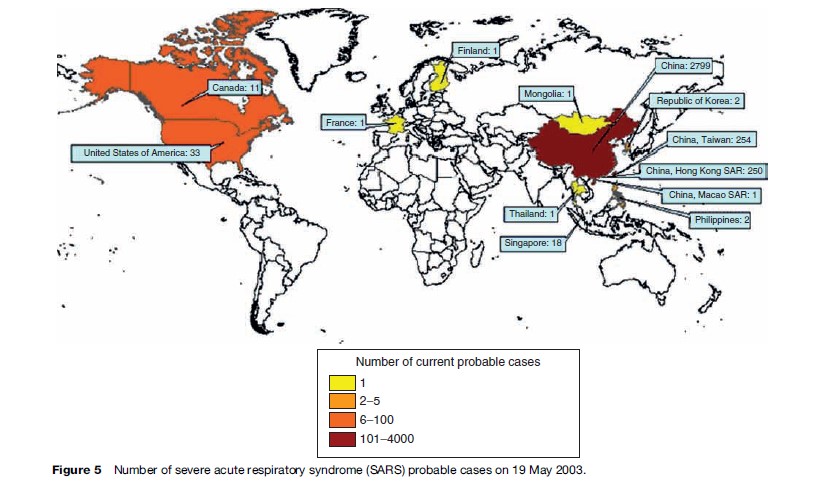
It is important to record the geographical areas where cases occurred or were discovered. Usually the place where the case occurred is important because there is the risk of spread. The movement of patients before the onset of the disease and during the course of the disease is also important to estimate the source of infection as well as the potential spread of the disease. In today’s rapidly developing travel, the movements of patients are very rapid and distant, suggesting rapid transmission of the pathogen across the continents, as seen in the SARS pandemic in 2002–03.
Person
In addition to the information mentioned above, important patient information includes gender, age, occupation, and the patient’s movement and activities during the incubation period and the estimated time and place in relation to the exposure to the patient of the infectious source, whether human, animal objects, or other sources.
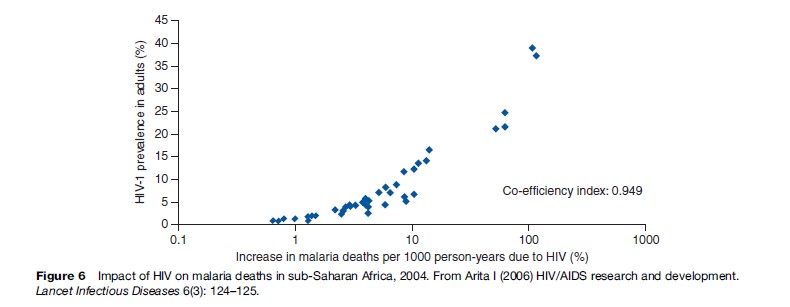
This information is sorted and collated to form a report that will be sent to the system or individuals who plan and initiate control measures. Additionally, the information is further analyzed with simple statistical methods or elaborated mathematical methods (Figure 5). Figure 6 shows co-relation between HIV prevalence and malaria mortality. These are discussed elsewhere. It is important to stress that simple raw data from sensitive surveillance are very useful for planners to initiate strategy formation.
Salient Surveillance Experiences: How It Works
International Sentinel Surveillance
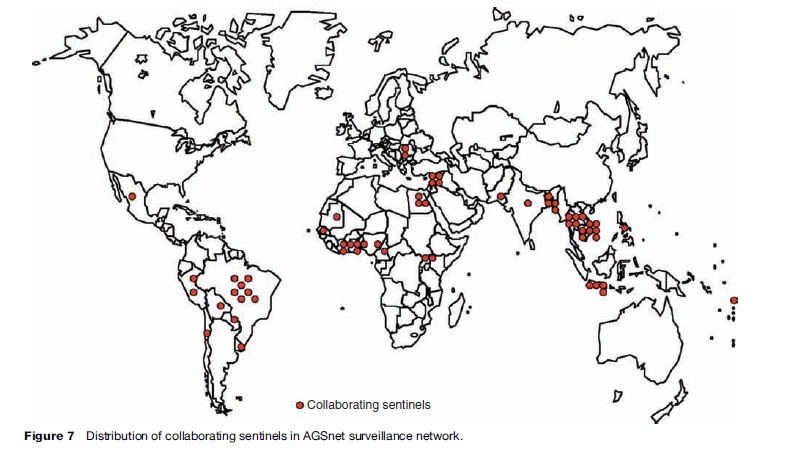
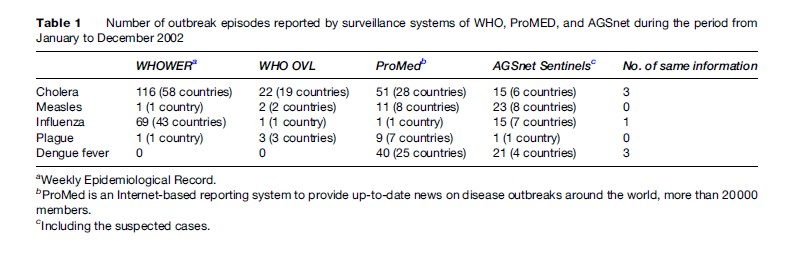
Sentinel-based surveillance may help to improve weaknesses by monitoring an area’s situation more closely and directly. For example, global surveillance on certain diseases may have certain weaknesses because adequate information is not available from areas because of political unrest, disinterest, poorly developed infrastructure, etc. The Agency for Cooperation in International Health (ACIH), a Japanese nongovernmental organization, has developed a voluntary sentinel surveillance system for selected target diseases, covering South America, Africa, and Asia. Its aim is to add more disease information and thus contribute to global epidemiological surveillance headed by WHO. The AGSnet (Alumni for Global Surveillance network) was organized in 1998. It consists of selected experts and managers who participated in several infectious-disease courses that were sponsored by the Japan International Cooperation Agency (JICA) and organized by ACIH. As of May 2006, the group consisted of 59 sentinel sites in 32 countries (Figure 7). Sentinels are divided into three categories: Hospitals and clinics, laboratories, and blood transfusion centers. Feedback from ACIH consists of selected epidemic information in the media and WHO and various surveillance articles published by medical journals. Despite a limited geographical coverage, the system seems to supplement disease information being obtained by global surveillance, as described in Table 1. The system has found unreported infectious diseases of international importance, including cholera, plague, and influenza. The surveillance data on prevalence of hepatitis B and C, HIV, and syphilis in blood donors from blood transfusion centers is unique, not usually available in the global surveillance network. It should be noted, however, that such a network in no way replaces or negates the need for strong national surveillance and alert and response mechanisms.
Smallpox Eradication And Its Surveillance System
The intensified smallpox eradication program was initiated in 1967 and succeeded in identifying the last chain of natural transmission in 1977 and the continuing program certified that the world was free of smallpox in 1980.
The first task of the program was to provide effective reporting of cases from the village/town level through the district to the national level and then the WHO regional level and finally to WHO HQ level.
In practice, the surveillance was divided into two areas: Smallpox-endemic countries (30 countries) and smallpox-free countries (or smallpox-imported countries). The former had a less effective system with significant problems of unreported cases and the latter had accurate reports; both operated following the International Health Regulation, which makes smallpox reporting obligatory, where smallpox occurrence in a smallpox-free nation should be regarded as a national emergency for immediate report and containment measurers. In both groups, also, the global program insisted that national health services and WHO should have the report weekly, including nil reports from endemic nations.
The measures to keep this principle workable specifically in the smallpox-endemic group are listed hereafter.
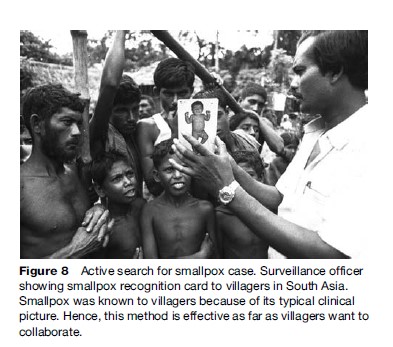
- Smallpox has no subclinical infection and its clinical manifestation is distinct. This increased the sensitivity of surveillance greatly. The picture cards, termed smallpox recognition cards, were invented by the Indonesian surveillance program as shown in Figure 8. Villagers immediately understood what disease was being searched for and that it had to be reported to the surveillance agent. The method was used in the entire smallpox eradication program.
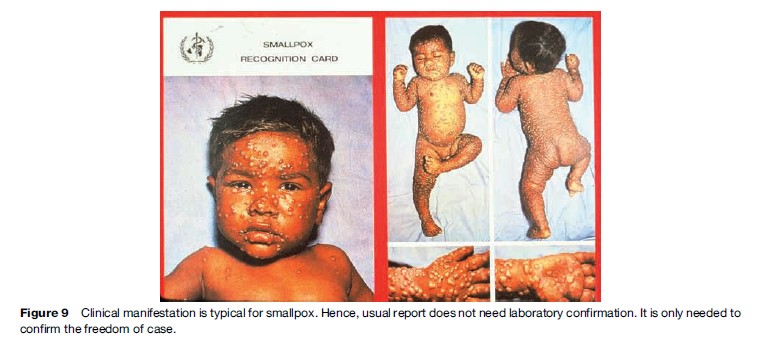
- This clear clinical manifestation did not require laboratory diagnosis procedures when the disease was known to be endemic (Figure 9). Only when the disease became rare was laboratory confirmation needed. This greatly simplified the surveillance procedures.
- As mentioned earlier, rewards were offered to the public who reported suspected smallpox and when it was confirmed by laboratory diagnosis.
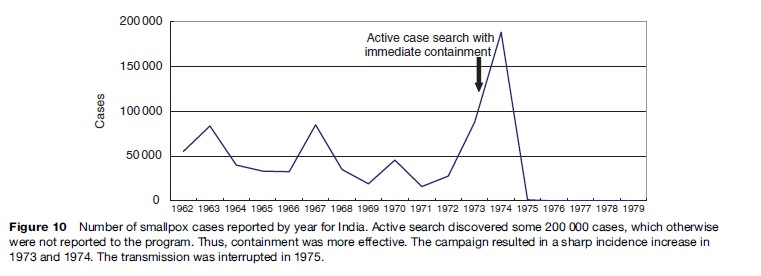
- In India, despite their intensive national vaccination program with the target of 100% coverage of the entire population for more than 5 years, transmission continued (Figure 10). Then the prime minister instructed all the health center staff (more than 200 health centers) to stop work for 1 week once a month and go to the villages to actively search for smallpox cases, and if found, immediately vaccinate the population of only the village where the case was found. This special campaign, termed the autumn campaign, started in September 1973 and the final case occurred in May, 1975. The evidence showed how surveillance combined with focused containment was effective. Since then (as of June 2006), there has been no smallpox case in India for a population of one billion.
During the 2-year certification period, every surveillance method was employed to search for hidden foci in the previously smallpox-endemic countries and their adjacent countries, with special house-to-house visit surveillance. Two years were determined to be the necessary period of such surveillance, based on the fact that it was known that 9 months had been the longest period between a false date of a last case and a true date of a last case in Africa. For safety, the 9 months were doubled to roughly 2 years.
In sum, the effectiveness of smallpox surveillance was proved by the fact that since the last case’s date of onset (October 26, 1977) in Somalia, there has been no occurrence of smallpox to date (as of 2006) except for the laboratory-infected case in the United Kingdom in 1978.
Surveillance Of Influenza Pandemics
As of June 2006, when this research paper was written, the world was close to a new influenza pandemic since the world experienced the last major pandemics in 1918, 1957, and 1968. This new threat is characteristic, with possible devastating effects on the world’s population with its severe pathogenicity to humans, perhaps comparable to the 1918 pandemic.
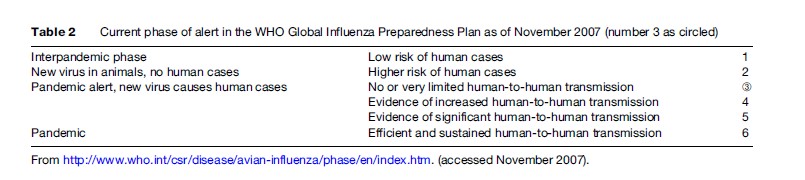
Furthermore, in view of an increased world population (two billion in 1918, six billion in 2006) as well as the increased speed and frequency of travel, once a pandemic occurs, the virus will spread rapidly throughout the world, possibly reaching all continents in less than 3 months. To prepare for such a pandemic virus, continuous global surveillance of influenza should be the key. WHO issued a series of recommended strategic actions for responding to the influenza pandemic threat and, based on these, each national authority has been preparing the National Influenza Pandemic Plans, as illustrated in Table 2.
Recognizing The Event
Epidemiological signals, such as an increase in the number of persons with unexplained respiratory illness with high mortality in an area over a short period of time, are likely to be the most sensitive and reliable indicators of a suspected pandemic event. Surveillance should focus on hospitals and communities with occurrences of respiratory infections and pneumonia. This may also be related to epidemics in poultry or bird populations, as will be discussed in the next section. Following detection of a cluster of suspected cases, an investigation should be started to characterize patients by person, place, and time and investigate the source or reservoir. Laboratory testing of samples to identify the causative agent should ideally be completed within 48 h following detection of the cluster.
Surveillance Of Animal Influenza
WHO issued the WHO Manual on Animal Influenza Diagnosis and Surveillance in collaboration with the World Organization for Animal Health (OIE: Office International des Epizooties). The aims of surveillance in lower animals such as pigs and birds are intended to complement the human surveillance network, to understand the ecology of influenza viruses that are relevant to human and animal health, and to determine the molecular basis of host range transmission and spread in new hosts.
Notification To National Health Authorities
Local health authorities should respond with a high level of suspicion and notify national health authorities as soon as preliminary information suggests that the cluster of cases is either unusual or different.
Reporting To WHO
Under the 2005 International Health Regulations, the national health authority should notify WHO within 24 h of detection of an epidemiological/virological signal suggestive of sustained human-to-human transmission of a new influenza virus. The national authority is requested to provide WHO with all relevant information, including the clinical, epidemiological, and laboratory data and the actions undertaken to contain the outbreak. Following the initial notification, the national authority should continue to report to WHO in a timely manner.
As of 4 July 2006, WHO had reported 229 cases including 131 deaths throughout the world since 2003. While the risk assessment with surveillance will continue (assuming the human pandemic has not yet occurred), it is essential for the world research efforts to concentrate on the geographical areas of risk where the favorable mutation of the virus is likely to occur, regardless of national boundaries. This tentatively includes East Asia, known to have a large concentration of the world avian population. Multi and bilateral organizations are anticipated to join such efforts, which may lead to swift preventive vaccine production.
Polio Eradication Surveillance
WHO global eradication of poliomyelitis was launched in 1988 with the target year of 2000, but in 2005, 2000 cases were reported in 16 nations in Africa and South Asia. Intensive surveillance and mass vaccination of children under 5 years are continuing.
Acute Flaccid Paralysis Surveillance
All acute flaccid paralysis (AFP) cases under 15 years of age should be reported immediately and investigated within 48 h. Because the causes of flaccid paralysis include not only poliomyelitis but also other diseases such as Guillain-Barre´ syndrome and transverse myelitis, AFP surveillance takes human power, time, effort, and skill to sort out true poliomyelitis cases. In China and elsewhere, hospital-based surveillance was useful for searching for patients by checking the medical records in the hospitals. To cover the problem nationwide, investigation was needed for all medical institutes, including large hospitals in urban areas and dispensaries in rural areas. In Africa’s rural areas, where health facilities are sparse, community based surveillance is conducted to detect polio cases. It is useful to have support from community leaders, such as senior members of the community and faith healers.
Laboratory Surveillance
For confirmation, two stool specimens should be collected 24–48 h apart and within 14 days of the onset of paralysis; viral isolation is performed in a laboratory. As poliovirus is excreted in feces during the acute period of illness, it is desirable to take samples at the early stage (less than 14 days from the onset of paralysis). The temperature should be carefully controlled during transportation of specimens (2–10 C with refrigeration). The results of laboratory diagnosis should be reported to the proper clinical/public health facilities without delay so that necessary action can be taken.
Surveillance Performance
AFP surveillance requires the following criteria: (1) one case per 100 000 children under 15 years of age (in 2006, WHO augmented this one AFP case to two cases because the recent intensified surveillance has resulted in two to three AFP cases when the surveillance was intensified due to reduced number of polio cases); (2) two adequate specimens collected from at least 60% of detected AFP cases; and (3) all specimens processed in a WHO-accredited laboratory. Currently, it is anticipated that this surveillance system will continue in the foreseeable future until WHO recommends discontinuing it.
Measles And Rubella Surveillance
Measles is the most transmissible viral disease. Until the vaccine was introduced in 1963, practically every child got measles. The primary purpose of measles surveillance is to detect, in a timely manner, all areas in which measles virus is circulating, but not necessarily detect every case. This requires the notification mainly of health units and timely case investigation of all suspected measles infections. Laboratory investigation for anti-measles IgM antibodies of suspected measles cases is important to confirm or exclude measles virus infection. A single serum specimen collected within 28 days of rash onset is used for the diagnosis. In previously vaccinated persons, there may be a small increased risk of not detecting an IgM response to measles when specimens are collected more than 2 weeks after rash onset due to the increased rate of IgM decay. There is some increased sensitivity if the sample is taken on or after day 3 of rash onset (though taking the sample at first contact is recommended).
Measles surveillance may need to be community based in areas where health units are nonexistent. It may be necessary to establish a system and procedures for collecting and testing blood samples from cases of acute fever and rash (AFR). Some other diseases whose main symptoms include fever or rash, such as rubella and parvovirus B19 infection, exist. In the surveillance of AFR, these patients are also reported and blood specimens are taken.
Surveillance Of Ebola Virus Hemorrhagic Fever
Since the 1976 discovery of the disease in Central Africa, the disease has been the focus of national and international surveillance because its spread has increased through recent frequent travel in Africa as well as intercontinental travel. Ebola is often characterized by the sudden onset of fever, intense weakness, muscle pain, headache, and sore throat. This is often followed by vomiting, diarrhea, rash, impaired kidney and liver function, and in some cases, both internal and external bleeding. Specialized laboratory tests on blood specimens detect specific antigens and/or genes of the virus. Antibodies to the virus can be detected, and the virus can be isolated in cell culture. For patient management, supportive care is to be given. No specific treatment or vaccine is yet available.
Surveillance is aimed at early detection of cases in order to avoid possible spread of the disease. Suspected cases should be isolated and strict barrier nursing techniques implemented. Contact tracing and follow-up of people who may have been exposed to Ebola through close contact is essential. All hospital personnel should be briefed on the nature of the disease and its routes of transmission. Communities affected by Ebola should make efforts to ensure that the population is well informed, both about the disease itself and about necessary outbreak containment measures, including burial of the deceased. People who have died from Ebola should be promptly and safely buried. As the primary mode of person-to-person transmission is contact with contaminated blood, secretions, or body fluids, any person who has had close physical contact with patients should be kept under strict surveillance. Ebola surveillance is a typical model that surveillance and containment are highly interrelated.
Surveillance Of Noncommunicable Diseases
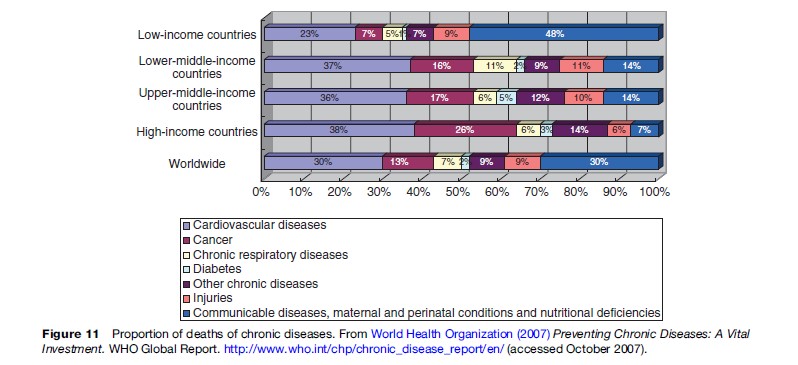
Public health surveillance has been extended not only to areas of communicable diseases but also surveillance of noncommunicable diseases. Although deaths caused by communicable diseases account for half of the total deaths in low-income countries, the proportion of deaths by chronic diseases has been significant, changing and increasing as the world economy changes (Figure 11). A few examples of how surveillance has elucidated analysis of the status and risk of specific noncommunicable diseases are given in the next sections.
Surveillance On Risk Factors For Noncommunicable Diseases
WHO developed the stepwise approach to surveillance of noncommunicable disease risk factors, termed STEPS (STEPwise approach to chronic disease risk factor surveillance), as part of a global surveillance strategy, aiming to monitor emerging patterns and trends worldwide and contain and reduce noncommunicable diseases. The STEPS approach is based on the concept that noncommunicable disease surveillance systems need to be simple, focusing on a minimum number of risk factors that predict disease, before placing too much emphasis on costly disease registries that are difficult to sustain over the long term, especially in low and middle-income countries. STEPS is a sequential process, starting with the gathering of information on key risk factors by the use of questionnaires (sociodemographic features, tobacco use, alcohol consumption, physical inactivity, and fruit and vegetable intake); then, taking simple physical measurements (height, weight, waist circumference, and blood pressure); and lastly, collecting blood samples for biochemical assessment (measurement of lipid and glucose levels).
Epidemiological Surveillance Research On Stroke And Cardiovascular Diseases
In Hisayama Town (population 7000), Japan, three cohort studies were conducted targeting residents aged 40 years or over in 1961, 1974, and 1988 after screening examinations. The cohort populations have been undergoing longitudinal observations by repeated health examinations (follow-up rate, 99%). When the subjects died, autopsy examinations were performed (mean autopsy rate, >80%). First, it aimed to study the prevalence of stroke and its risk factors, but later the study was expanded, targeting stroke, cardiovascular diseases, cancer, senile dementia, diabetes, and lifestyle-related diseases. The fourth study has been started, adding the molecular epidemiological study to find the genomic risk factors. The results have been reflected in national policy formation on the prevention.
Cancer Registries
Cancer registries are part of the surveillance system. Population-based registries provide information on incidence cases and incidence trends, whereas hospital-based registries provide information regarding diagnosis, stage distribution, treatment methods, and survival. For example, in Japan, cancer occurrence is monitored through population-based and hospital-based cancer registries by the Japanese Association of Cancer Registries in collaboration with 34 prefectural governments, supported and maintained by the Research Center for Cancer Prevention and Screening, National Cancer Center. Hospitals and clinics are encouraged to report the occurrence to the prefectural government, which summarizes and analyzes their reports.
Surveillance Of Accidents And Self-Inflicted Injuries
Injuries constitute a major public health problem. According to WHO data for 2000, an estimated 5 million people die each year as a result of some form of injury, comprising almost 9% of all deaths worldwide. Road traffic and self-inflicted injuries are the leading causes. The costs of injury mortality and morbidity are immense in terms of lost economic opportunity, demands on national health budgets, and personal suffering. Nevertheless, few countries
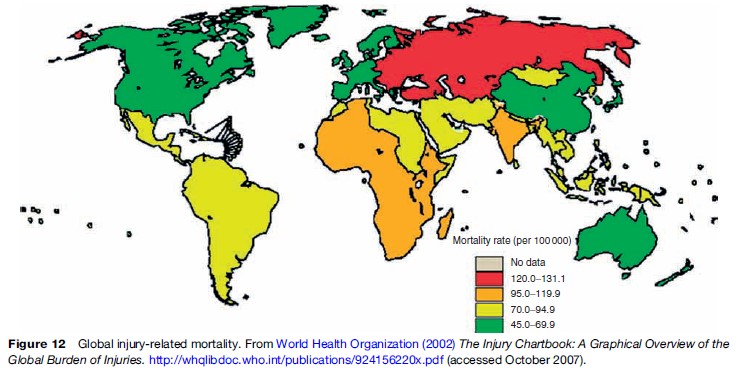
have surveillance systems that generate reliable information on the nature and frequency of injuries. Aiming to collect better information and, in turn, to develop effective prevention programs, the WHO, in collaboration with the U.S. CDC, produced manuals on how to set up surveillance systems for collecting, coding, and processing data. In active surveillance, injury cases are sought out and investigated; injured persons are interviewed and followed up. For example, active surveillance of child abuse cases would involve identifying and locating cases through a variety of sources, such as police reports, social agencies, and educational authorities. It might involve seeking out the abused children, their parents, and/or the appropriate authorities, conducting interviews and follow-up. In passive surveillance, relevant information is collected in the course of doing other routine tasks. For example, doctors are routinely required to fill out death certificates for legal purposes, but it is possible to extract information entered on those certificates to obtain data on deaths from injuries. Forms filled out by doctors or nurses for medical insurance purposes can also be used for surveillance purposes. Other potential sources of data on fatal injuries include autopsy/ pathology reports and police reports, and on severe nonfatal injuries, trauma registries, and ambulance or emergency medical technician records. In Japan, the statistics on fatal and nonfatal injuries, including accidents and suicide, are available based on police reports, the Population Survey Report, and death certificates. In addition to a hospital-based surveillance system, community-based surveys may provide a complement to capture further reports on injury events and deaths in the community. Those treated outside the formal health sector or those with minor injuries that do not necessarily require hospital attention might be missed by a hospital-based surveillance system, so that community-based surveys are one way of obtaining injury events within a community. Surveillance on this type of health hazards will become an important surveillance function in today’s world, depending upon the level and extent of the health hazard in individual nations (Figure 12).
Global Surveillance Network
International surveillance on epidemic diseases or diseases of international importance has been carried out by different organizations under WHO’s Global Outbreak Alert and Response Network (GOARN) (Figure 13).
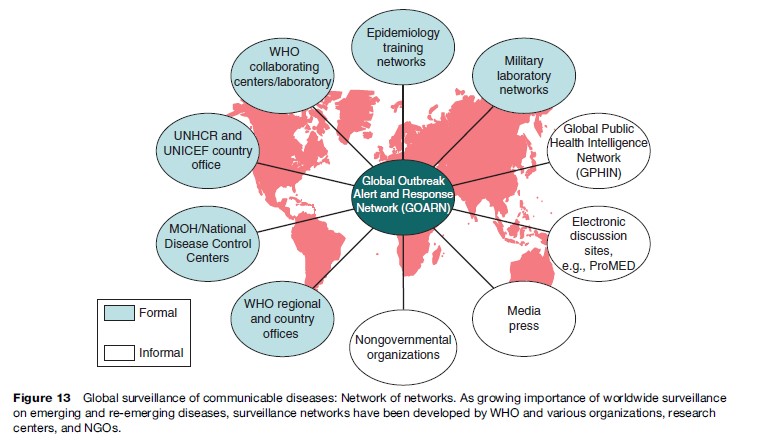
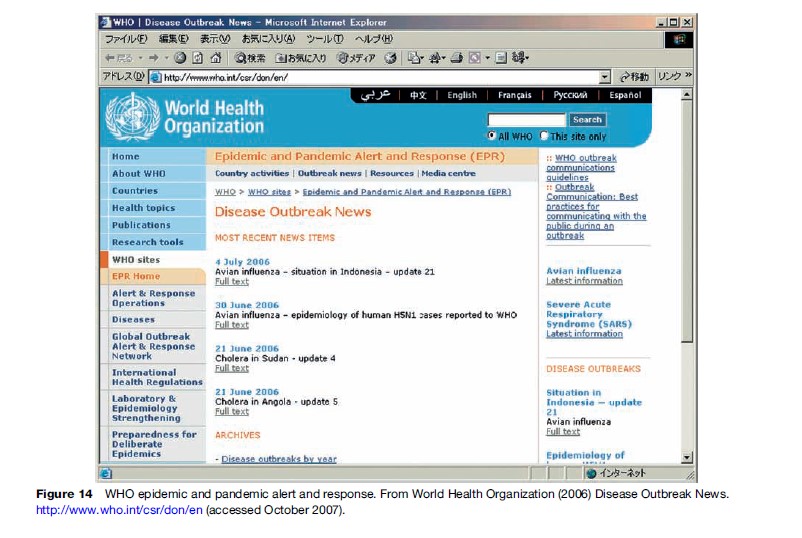
The office covering GOARN is situated in WHO headquarters in Geneva and every week through the electronic network dispatches assorted surveillance data to all nations and individual institutions for their review and necessary action (Figure 14).
In 2005, WHO and the member states renewed the International Health Regulations whose purpose is ‘‘to ensure the maximum protection of people against the international spread, while minimizing interference with world travel and trade.’’ The diagram of the surveillance system is shown in Figure 15.
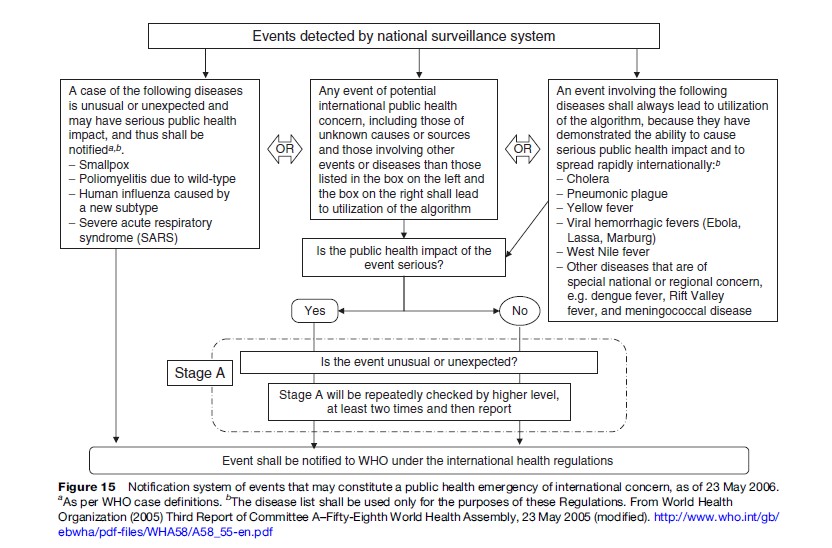
This purpose certainly requires a well-organized surveillance network, as shown in Figure 14. The diseases that the system would handle are shown in Figure 15. In 2006, the World Health Assembly (WHA) further amended the International Health Regulations (IHR) to strengthen surveillance on the possible avian influenza pandemic.
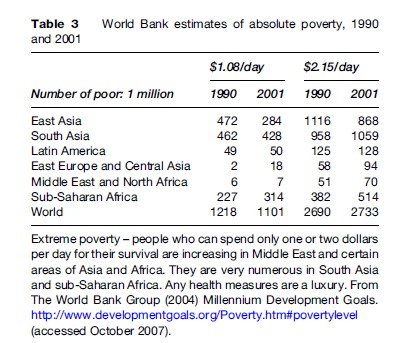
The performance of international surveillance has been significantly affected by the unprecedented technology development in the last and this century. For example, electronics technology has prompted the real-time reporting and molecular biology has led to the discovery of the pathogen source in distant or unthinkable circumstances such as the spread of polio virus or SARS virus cases. On the other hand, a rapid increase in the global population (4 billion at the end of the nineteenth century, 6 billion at the end of the twentieth century) and increasing frequency of travel by air, sea, and land accelerates disease transmission. The situation is further worsening by expanding inequality. Of 6 billion people in the world, 1.5 billion (15%) live at a level of poverty of $1–2 per day (Table 3). Thus, in sub-Saharan Africa, for example, extreme poverty and the prevalence of severe diseases cause a vicious cycle and pose a threat to neighboring geographical regions. The situation makes conducting surveillance ineffective and complicated, coupled with the inadequacy of health services under the strain of limited resources and in some areas of political unrest. In these circumstances, the importance of global collaboration to strengthen area-wide surveillance was increasingly recognized in the late twentieth century and early in this century.
The surveillance system mentioned above requires the collaboration by all WHO member states. WHO Assembly, as necessary, reviews and makes recommendations on how the member states and experts concerned contribute to the effective performance of international surveillance in different geographical regions. It is important to note that the surveillance activities in areas of extreme poverty require substantial cooperation from rich nations. Such cooperation contributes in turn to the development of effective global surveillance.
Ethical And Legal Aspects Of Surveillance
Surveillance activities often involve surveillance workers handling communities, people, and institutions in terms of health hazard investigation, collection of technical as well as originally private information, and publication of the collected information. It is important that the purpose of surveillance should be known or fully explained as needed to the community or individuals so that surveillance teams can obtain needed information with good cooperation on the part of the community or individuals. When it is planned, surveillance should ensure that individuals’ and agencies’ right to privacy will not be violated. In some cases, however, this is not simple, because the right to privacy and the right to know scientific information conflict.
Bibliography:
- Arita I, Nakane M, Kojima K, Yoshihara N, Nakano T, and El-Gohary A (2004) Role of a sentinel surveillance system in the context of global surveillance of infectious diseases. Lancet Infect Diseases 4(3): 171–177.
- Dowdle WR, Hopkins D, and Hopkins DR (eds.) (1998) Dahlem Workshop on the Eradication of Infectious Diseases. London: John Wiley.
- Fenner F, Henderson DA, Arita I, et al. (1988) Smallpox and Its Eradication. Geneva, Switzerland: World Health Organization.
- Heymann DL and Rodier GR (1998) Global surveillance of communicable diseases. Emerging Infectious Diseases 4(3): 362–365.
- Teutsch SM and Churchill RE (2000) Principles and Practice of Public Health Surveillance. 2nd edn. New York: Oxford University Press.
- The World Bank Group (2004) Millennium Development Goals. http:// www.developmentgoals.org/Poverty.htm#povertylevel (accessed October 2007).
- World Health Organization (1999) WHO Recommended Surveillance Standards, 2nd edn. WHO/CDS/CSR/ISR/99/2/EN, Geneva, Switzerland: World Health Organisation.
- World Health Organization (2002) The Injury Chartbook: A Graphical Overview of the Global Burden of Injuries. http:// whqlibdoc.who.int/publications/924156220x.pdf (accessed October 2007).
- World Health Organization (2007) Preventing Chronic Diseases: A Vital Investment. WHO Global Report. http://www.who.int/chp/chronic_disease_report/en/ (accessed October 2007).
- http://www.polioeradication.org/– Global Polio Eradication Initiative.
- http://www.who.int/csr/en/– World Health Organization, Epidemic and Pandemic Alert and Response.
- http://www.who.int/csr/ihr/en/– World Health Organization, International Health Regulation (2005).
- http://www.who.int/wer/en/– World Health Organization, Weekly Epidemiological Record.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








