This sample The UN Commission of Social Determinants of Health Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Rationale And Goal
Broad progress in global health since World War II has not been evenly distributed across populations. Indeed, recent breakthroughs in medical technology and gains in indicators such as global average life expectancy have been accompanied by widening health gaps between social groups, between and within countries. Health differences among population groups that could be avoided or remedied, and that are unfair, are called health inequities (WHO Equity Team, 2004). Epidemiological research shows that the bulk of the global burden of disease and the greatest portion of health inequities arise from the social conditions in which people live and work – referred to as the social determinants of health (SDH).
The Commission on Social Determinants of Health (CSDH) was created by the World Health Organization (WHO) to promote greater health equity. It aims to do so by catalyzing policy and institutional change to address the SDH within countries and among institutions working in global health, including WHO itself. The Commission was created by WHO Director-General Lee Jong-wook and is chaired by epidemiologist Sir Michael Marmot. It was launched in March 2005 and will submit its final report in May 2008.
Historical Background
The Commission builds on a historical tradition. Public health scientists have long observed that social conditions decisively influence health. The sanitary campaigns of the nineteenth century and the work of the founders of modern public health reflected awareness of the relationship between people’s social position, their living conditions, and their health outcomes. Rudolf Virchow (1985 [1848]) asked, ‘‘Do we not always find the diseases of the populace traceable to defects in society?’’ During the twentieth century, traditions of social medicine developed in several global regions, notably Latin America, linking health progress to processes of community self-empowerment and movements for political and social change (Tajer, 2003).
During recent decades, international health agendas have tended to oscillate between (1) an understanding of health as a social phenomenon, requiring intersectoral policy action and often linked to social justice agendas, and (2) approaches relying on narrowly defined, technology-based medical and public health interventions. WHO’s 1948 Constitution clearly acknowledges the impact of social conditions on health, and the need for collaboration with sectors such as agriculture, education, housing, and social welfare to achieve health gains. During the 1950s and 1960s, however, WHO and other global health actors emphasized technology-driven, vertical campaigns targeting specific diseases, with little regard for social contexts (Brown et al., 2006).
Alma-Ata And Health For All
A social model of health was revived by the 1978 Declaration of the Alma-Ata Conference on Primary Health Care and the ensuing Health for All movement. The Alma-Ata Declaration laid out a vision of equitable health improvement based on ‘‘development in the spirit of social justice’’ (WHO and UNICEF, 1978). Primary health care as defined at Alma-Ata included the creation of healthy living and working conditions through intersectoral programs.
Many governments embraced the principle of intersectoral action on SDH under the banner of Health for All. However, the market-liberalizing economic models that gained global ascendancy during the 1980s created obstacles to policy action on social determinants. In the health sector, these approaches mandated market-oriented reforms that emphasized efficiency over equity as a system goal and often reduced disadvantaged social groups’ access to health-care services (Hofrichter, 2003; Homedes and Ugalde, 2005). On the level of macroeconomic policy, the structural adjustment programs adopted by many developing countries under the guidance of international financial institutions mandated sharp reductions in governments’ social sector spending, constraining policy makers’ capacity to address key SDH (Werner and Sanders, 1997).
Renewing The Health Equity Agenda In The Twenty-First Century
During the late 1990s and the first years of the twenty-first century, evidence accumulated that existing health policies had failed to reduce inequities, and momentum for new, equity-focused approaches grew, at first primarily in wealthy countries. The CSDH builds on this momentum and aims to ensure that developing countries also benefit. The creation of the CSDH can be seen as part of a broader effort to revive WHO’s constitutional commitment to health equity and to rekindle the energy of Health for All. The architect of the Commission was WHO Director-General Lee Jong-wook. Lee saw significance in the fact that the Commission would submit its final report in 2008, the 30th anniversary of the Alma-Ata conference and 60 years after the adoption of the WHO constitution. Taking leadership of WHO in January 2007, Margaret Chan, Lee’s successor as director-general, is incorporating the CSDH in an effort to refocus global health work on primary health care.
The Social Production Of Health Inequities
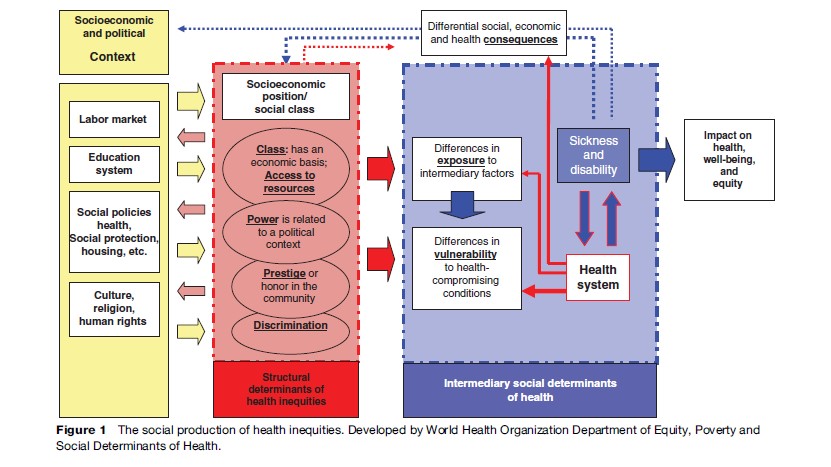
Many social factors influence people’s health, but not all determinants are equally important. The CSDH has chosen to focus primarily on factors that contribute to creating and maintaining health inequities. Under the broad category of health determinants, the CSDH distinguishes between the determinants of health inequities (structural determinants) and intermediary determinants of health.
Structural And Intermediary Determinants
Structural determinants are those that produce stratification within society. Structural determinants are rooted in key socioeconomic and political institutions. Structural factors establish a set of socioeconomic positions within hierarchies of power, prestige, and access to resources. The most important structural stratifiers include income, social class, education, occupation, gender, and race or ethnicity. The fundamental mechanisms that produce and maintain (but that can also reduce or mitigate) this stratification include governance; the education system; labor market structures; and redistributive welfare state policies or their absence (Navarro et al., 2006). The structural mechanisms that shape social hierarchies and assign individuals to differential social positions according to the key stratifiers are the root cause of inequities in health (Diderichsen et al., 2001).
In shaping individual health status and outcomes, the underlying social determinants of health (SDH) inequities operate through a set of intermediary determinants of health. The main categories of intermediary determinants of health are material circumstances, psychosocial circumstances, behavioral and/or biological factors, and the health system itself as a social determinant. Material circumstances include factors such as housing and neighborhood quality, consumption potential (i.e., the financial means to buy healthy food, warm clothing, etc.), and the physical work environment. Psychosocial circumstances include psychosocial stressors arising from living circumstances and relationships, along with social support and coping styles. Behavioral and biological factors include nutrition, physical activity, and tobacco and alcohol consumption, which are distributed differently among different social groups.
Figure 1 illustrates the social production of health inequities. Reading from left to right, the figure shows how the configuration of key economic, social, and cultural institutions, including the labor market and the education system, gives rise in each society to a hierarchically ordered set of socioeconomic positions that people can occupy. Groups are stratified according to the economic status, power, and prestige they enjoy, for which we use social class, income levels, education, occupation status, gender, race or ethnicity, and other factors as proxy indicators. The structural mechanisms of social stratification shape health through more specific, intermediary determinants (blue column in Figure 1). Based on their respective social status, individuals experience differences in exposure and vulnerability to health-compromising conditions. The diagram also highlights the feedback effects through which illness may affect individual social position.
The Health System As A Determinant
The CSDH model departs from many previous approaches by conceptualizing the health system itself as a social determinant of health. The role of the health system becomes particularly relevant through the issue of access to health services. Different social groups (for example, higher and lower income groups, women, and men) have different opportunities to access health services. Health systems can be more or less enabling and responsive in creating conditions that facilitate access for vulnerable and excluded groups. The health system also plays an important role in mediating the differential consequences of illness in people’s lives. The social, economic, and other consequences of specific forms of illness and injury vary significantly, depending on the social position of the person who falls sick. To the extent that the health system incorporates mechanisms to mitigate these differential consequences, or fails to do so, the system itself operates as a determinant of health.
Health Gaps And Gradients
In all societies for which data are obtainable, health follows a clear social gradient. It is not simply that the rich live longer, healthier lives than the poor do. Rather, life expectancy, incidence rates of major diseases, and virtually all other significant measures of population health precisely mirror the steps of the social ladder (Marmot and Wilkinson, 2006). When people are ranked on a socioeconomic scale (by income quintile, for example), each group exhibits better health than does the group below it and poorer health than the group above.
A crucial question then arises about how the objective of public policies on health equity should be formulated. Three broad approaches to reducing health inequities can be identified, based on (1) targeted programs whose objective is simply to improve health among disadvantaged populations, without reference to what is happening with other groups; (2) closing health gaps between worse-off and better-off groups; and (3) addressing the social health gradient across the whole population, that is, improving health for all groups, but with the fastest gains in the lower portions of the social spectrum. The CSDH maintains that a consistent equity-based approach to SDH must ultimately lead to a gradients focus. However, strategies based on tackling health disadvantage, health gaps, and gradients are not mutually exclusive. They can complement and build on each other (Graham and Kelly, 2004).
CSDH Structure And Ways Of Working
The CSDH seeks to distinguish itself from some other commissions whose activity was limited to desk research and the production of a report. CSDH results should include demonstrable progress in catalyzing policy and institutional change, as well as the publication of high-quality reports and research.
The main components of the CSDH include the 20 commissioners, evidence-gathering Knowledge Networks, partner countries, and civil society organizations. The Commission also works in close partnership with a number of global institutions, most prominently WHO. The commissioners are 20 people chosen for being innovators in science, public health, policy making, and action for social change. The group includes leading health experts but also economists such as Nobel laureate Amartya Sen and political leaders, including Ricardo Lagos, former President of Chile, and Pascoal Mocumbe, former Prime Minister of Mozambique.
Knowledge Networks
The bulk of the Commission’s scientific work is undertaken by nine Knowledge Networks. Their mandate is to go beyond describing the problem of health inequities to identify effective policies to reduce them. Each Knowledge Network includes scientists, policy makers, civil society representatives, and practitioners from developing and developed countries who work together to compile knowledge on interventions to overcome the social barriers to health. Networks have between 10 and 20 members.
The Knowledge Networks are structured by themes:
- Early child development
- Employment conditions
- Globalization
- Health systems
- Measurement and evidence
- Priority public health conditions
- Social exclusion
- Urban settings
- Women and gender equity.
Each network generates knowledge products that support the Commission’s policy dialogue with countries and that feed into CSDH publications and reports.
Action In Countries
The CSDH learns from policy innovations in countries and provides a platform for disseminating solutions. The CSDH will collaborate with countries in a variety of ways. These include creating awareness and understanding of SDH among political leaders and stakeholders, capacity building and implementing specific interventions, and helping countries adopt comprehensive health and development policies oriented toward the SDH. To be fully effective, social determinant policies require action across a range of sectors, such as finance, labor, education, and transportation, as well as health. The CSDH describes this as a whole-government approach to tackling health inequities through action on determinants.
While working with all interested countries, the CSDH is building intensive partnerships with a particular group of countries committed to comprehensive, cross governmental action on social determinants. Examples of action in countries include the following:
- Brazil: Brazil has created its own National Commission on Social Determinants of Health, linked to the CSDH. The Brazilian Commission seeks to (1) improve the quality of sociodemographic data collected in the country in order to facilitate the monitoring of health inequities, (2) include the SDH and the consequences of inequity in the training of health professionals, (3) mobilize civil society to safeguard equity as a principle and ensure its implementation in public policies, (4) create intersectoral fora to debate and establish ways of tackling social determinants, including short-, medium-, and long-term policies, and (5) finance research and support the training of researchers in the area of SDH.
- . Canada: In partnership with the CSDH, Canada has undertaken a review of experiences in intersectoral action to identify success factors, barriers, best practices, and unresolved issues and to develop recommendations. Canada is systematizing knowledge about tackling social determinants using an intersectoral approach in the development and implementation of social policies.
- Mozambique: The CSDH is working in a multisectoral process with Mozambique’s ministries of labor, public housing, planning, and education, among others, to develop a national work plan on SDH.
Civil Society Engagement
The political sustainability of social determinants policies at the national level depends on the support of civil society and communities. The CSDH has asked networks of civil society organizations to develop strategies for civil society collaboration with the Commission in all global regions. These strategies are being shaped through consultative processes involving a broad spectrum of civil society and grassroots groups. They will help ensure that the CSDH agenda reflects communities’ needs and knowledge and that informed social demand supports the policy change process in countries (Solar and Irwin, 2006).
Public Policy Approaches On Social Determinants
The CSDH has identified key directions for public policy on social determinants. Three of the most important are tackling both structural and intermediary determinants, mobilizing multiple sectors, and ensuring social participation and empowerment.
Arguably the single most significant lesson of the Commission’s analysis is that government action to reduce health inequities must not be limited to intermediary determinants but must include policies crafted to tackle underlying structural determinants. Because they engage the core institutions that distribute power and resources within society, policies on the structural determinants of health inequities must be designed with careful attention to contextual specificities, which should be rigorously characterized using methodologies developed by social and political science. Analyses of context must include global as well as national dimensions.
Tackling the structural determinants of health inequities requires intersectoral policy making because structural determinants can be addressed only by policies extending beyond the health sector. The CSDH aims to (1) identify successful examples of intersectoral action on SDH in jurisdictions with different levels of resources and administrative capacity and (2) characterize in detail the political and management mechanisms that have enabled effective intersectoral programs to function sustainably.
Participation of civil society and affected communities in the design and implementation of policies to address social determinants is essential to success. Genuinely empowering social participation provides both ethical legitimacy and a sustainable base to take the social determinants agenda forward after the Commission has completed its work. With the help of its civil society partners, the CSDH is identifying positive examples of social participation in policy-making processes, while also diagnosing and analyzing the barriers that often prevent participation.
Tackling the social determinants of health inequities requires enlarging the definition of health policy. Health equity policies do not come from the health sector alone. The health sector must support other sectors, such as transport and labor, to incorporate health equity as a goal and monitor the health equity impact of policies and programs. This approach also changes the health sector itself. A health system responsive to the determinants of health equity moves beyond traditional health promotion interventions targeted at individual risk factors. Equity in access to services becomes a key system priority, with implications for financing and budgeting; program design, monitoring, and evaluation; and other aspects of health system performance.
CSDH Legacy And Future Agenda For Action
The CSDH signals a renewal of WHO’s constitutional commitment to health equity. At the national level, it fosters comprehensive, cross-governmental action on social determinants. After 3 years, the Commission aims to leave the following legacy: (1) Social determinants will be incorporated into national health policy processes in a growing number of countries, particularly in the developing world; (2) the opportunities for health policy action on social determinants, and the costs of not acting, will be more broadly known and understood; (3) scientific knowledge on pathways between social factors and health equity will be consolidated, knowledge gaps clarified, and appropriate directions for ongoing research identified; and (4) social determinants and health equity will be incorporated as priorities in WHO’s General Programme of Work 2007–2015, the long-range planning document that sets the organization’s strategic directions.
Beyond May 2008, the agenda for action on social determinants will be taken forward by other actors. The Commission’s ultimate impact will depend on its success in engaging, during its lifetime, those constituencies that can sustain future action on social determinants. National governments are the main agents with responsibility for health equity. Accordingly, the Commission has sought to broker connections among health policy makers in countries pursuing action on social determinants. It has created platforms for knowledge sharing and collaboration among countries. But because governments and their priorities shift with the pressures of electoral politics, a social determinants perspective must be anchored in international institutions that serve as stable partners and trusted sources of policy guidance to countries over time. That is why the CSDH has also worked to promote change in WHO itself.
Political action on health equity will not occur without the pressure of organized social demand. The CSDH engagement with civil society reflects an effort to grapple with this challenge. The commitment to involve civil society organizations as active partners distinguishes the CSDH from many previous United Nations and WHO processes. Yet the extent to which the Commission is actually able to inform and empower civil society constituencies to drive action on social determinants remains to be seen. The extent to which the findings and recommendations of the CSDH are taken up by civil society and community organizations in their advocacy will be an important indicator of the Commission’s success and a predictor of its long-term relevance.
Bibliography:
- Brown T, Cueto M, and Fee E (2006) The World Health Organization and the transition from international to global public health. American Journal of Public Health 96(1): 62–72.
- Diderichsen F, Evans T, and Whitehead M (2001) The social basis of disparities in health. In: Evans T, Whitehead M, Diderichsen F, Bhuiya A and Wirth M (eds.) 2001. Challenging Inequities in Health, pp. 12–23. New York: Oxford University Press
- Graham H and Kelly MP (2004) Health Inequalities: Concepts, Frameworks and Policy. London: NHS Health Development Agency.
- Hofrichter R (ed.) (2003) Health and Social Justice: Politics, Ideology, and Inequity in the Distribution of Disease. San Francisco, CA: Jossey-Bass.
- Homedes N and Ugalde A (2005) Why neoliberal health reforms have failed in Latin America. Health Policy 71: 83–96.
- Marmot M and Wilkinson R (2006) Social Determinants of Health, 2nd edn. Oxford, UK: Oxford University Press.
- Navarro V, Muntaner C, Borrell C, et al. (2006) Politics and health outcomes. Lancet 368(9540): 1033–1037.
- Solar O and Irwin A (2006) Social determinants, political contexts and civil society action: A historical perspective on the Commission on Social Determinants of Health. Health Promotion Journal of Australia 17(3): 180–185.
- Tajer D (2003) Latin American social medicine: Roots, development during the 1990s, and current challenges. American Journal of Public Health 93(12): 2023–2027.
- Virchow R (1985 [1848]) Collected Essays on Public Health and Epidemiology. Canton, MA: Science History Publications.
- Werner D and Sanders D (1997) Questioning the Solution: The Politics of Primary Health Care and Child Survival. Palo Alto, CA: Healthwrights.
- World Health Organization Equity Team (2004) Glossary of key terms. Unpublished working paper.
- World Health Organization UNICEF (1978) Declaration of Alma-Ata. Geneva, Switzerland: World Health Organization.
- Evans RG, Barer ML, and Marmor T (1994) Why Are Some People Healthy and Others Not? The Determinants of Health of Populations. New York: A de Gruyter.
- Evans T, Whitehead M, Diderichsen F, Bhuiya A, and Wirth M (eds.) (2001) Challenging Inequities in Health. New York: Oxford University Press.
- Krieger N (2001) A glossary for social epidemiology. Journal of Epidemiology and Community Health 55(10): 693–700.
- Lalonde M (1974) A New Perspective on the Health of Canadians. Ottawa, Canada: Ministry of Health and Welfare.
- Lee JW (2005) Public health is a social issue. Lancet 365: 1005–1006.
- Mahler H (1981) The meaning of health for all by the year 2000. World Health Forum 2(1): 5–22.
- Marmot M (2005) Social determinants of health inequalities. Lancet 365: 1099–1104.
- Marmot M, Rose G, Shipley M, and Hamilton PJ (1978) Employment grade and coronary heart disease in British civil servants. Journal of Epidemiology and Community Health 32: 244–249.
- Raphael D (ed.) (2004) Social Determinants of Health: Canadian Perspectives. Toronto, ON: Canadian Scholars Press.
- Rosenfield P (1985) The contribution of social and political factors to good health. In: Halstead S, Walsh J and Warren K (eds.) Good Health at Low Cost, pp. 173–185. New York: Rockefeller Foundation
- Tarlov A (1996) Social determinants of health: The sociobiological translation. In: Blane D, Brunner E and Wilkinson R (eds.) Health and Social Organization, pp. 71–93. London: Routledge
- World Health Organization (1948) Constitution of the World Health Organization. Geneva, Switzerland: World Health Organization.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








