This sample National Health Systems Research Paper is published for educational and informational purposes only. If you need help writing your assignment, please use our research paper writing service and buy a paper on any topic at affordable price. Also check our tips on how to write a research paper, see the lists of health research paper topics, and browse research paper examples.
Introduction: What Is A National Health System?
There is no single definition of what might comprise a ‘national’ health system. According to the World Health Organization (WHO, 2000), for example, it comprises ‘‘all activities whose primary purpose is to restore and maintain health … improving the health of the population they serve, responding to people’s expectations, and providing financial protection against the costs of ill-health’’ (WHO 2000: 5–8). The activities (health actions, according to WHO) of a national health system are thus characterized by the expressed intent of those within it to improve health. The definition is a useful one in that it recognizes that any health system is a combination of resources, organizations, and financing and management arrangements that ultimately culminate in the delivery of health services to a population. Therefore, every country can be said to have some form of national health-care system, regardless of how unstructured or unsystematic its operation.
Building an effective and affordable national health system is a major preoccupation of governments around the world as they attempt to bring together – whether by contractual incentives or through publicly delivered services – the necessary components that are needed to improve health status and provide accessible and responsive services to the needs of individuals, families, and communities. A major difference, therefore, between a health system and a ‘national’ health system is the involvement of the state (governments and legislative bodies). Consequently, the nature of a national health system is characterized as much by predominant political motivations as it is by the opportunities and/or limitations imposed by the availability of financial and human resources.
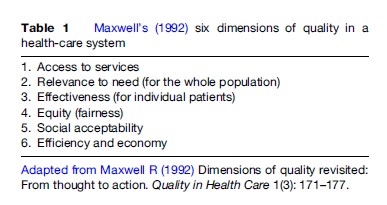
As Maxwell (1992) discusses in his six dimensions of quality (Table 1), the principles of all national healthcare systems are broadly the same yet the combination of these principles can lead to competition, both politically and financially, depending on which principles are regarded as more or less important. If one was to think of a national health system as an automobile, for example, there are trade-offs to be had between choosing a model that is eco-friendly and economical with one that has a high-performance engine and a higher specification of internal comfort. What aspects of care make a national health-care system more or less effective can, therefore, depend on individual circumstances or point of view. It is because of this that national health systems can be seen to have varying degrees of success in living up to these different principles and are so readily influenced by political objectives.
The Functions Of A National Health-Care System
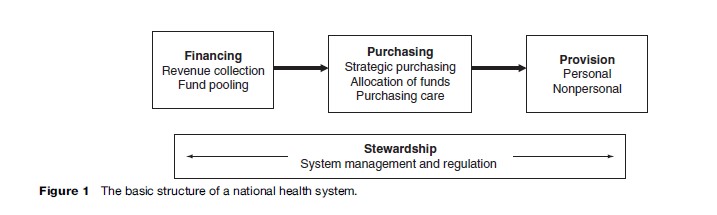
The basic structure of a national health system can perhaps best be illustrated in Figure 1. It reveals that all national health systems are split into four principal functions: financing, purchasing (or resource allocation), service provision, and stewardship. Within each principal function are a number of important subfunctions. For instance, the financing element to a national health-care system requires not only the ability to collect revenue but also a process of managing that revenue collection through, typically, the pooling of resources to ensure that the risk of having to pay for health care is shared across a population rather than by each contributor individually. Similarly, the provision of services can be usefully split between personal services (services that people receive from a health agent, such as a doctor or dentist) and nonpersonal services (programs manifested in public health measures to promote healthy lifestyles or public works that improve water quality and reduce the prevalence of disease). Stewardship, which is represented as a theme working across the three main delivery elements of the system, represents the important process of managing and/or regulating the national health system. This is an important aspect because it is the responsibility of the system to protect the people by ensuring their money is used wisely. Stewardship of the system, through regulation and governance of activities, can also promote efficiency and quality in care delivery practice and may also help to engender a sense of national citizenship. These four principal functions of national health systems are performed very differently internationally. The following sections will illustrate these variances using case examples.
Formal Care And Lay Care
Before embarking on an analysis of the different functions of a national health system, it is important to make a quick distinction between formal and lay (or informal) care. When considering the components that make up a national health-care system, it is tempting to think immediately of doctors and nurses, of surgeries and hospitals, or of educational and health promotional interventions. However, it is a fact that the majority of health care (over 80%) is administered by one’s self (self-care), family members, friends, and ‘lay carers.’ This is true regardless of a country’s level of development. Hence, while a national health system encompasses a wide range of activities with a health improvement goal, the major part of care is provided in the informal setting and is unpaid.
In the United Kingdom, for example, about one-eighth of adults act as ‘health carers’ to some extent (not including routine parenting such as care for a sick child). Whereas much of this is social care (feeding, washing, dressing, and providing emotional support) the system has begun to invest in ‘expert carers’ that, for instance, enable more lay people to provide care advice, dress wounds, or give intravenous drugs. That the services provided by lay carers in the UK crosses the boundary with formal care provides recognition that there is a significant gray area in distinguishing between the formal (within the system) and the informal (out of the system).
Financing Health Care
Financing a health-care system is critical to its sustainability and key challenges are faced in ensuring that the necessary organizational and institutional arrangements are in place to raise revenue from which to reward and motivate health-care providers. There are two principal functions to financing: (1) revenue collection, the process by which a national health system receives money, and (2) pooling resources, the process by which this revenue is managed to ensure that individual contributors are not exposed to the high costs of having to pay for health care through risk sharing with other members of the pool. According to the World Health Organization (2000), differences in how these functions are administered impact directly on the relative performance of national healthcare systems, yet the mechanisms through which financing systems operate can vary dramatically between nations.
In an excellent analysis of the advantages and disadvantages of different funding options, Mossialos et al. (2002) show that revenue can be collected from a range of sources, through varying collection mechanisms, and by different collection agents. Examples of funding sources, contribution mechanisms, and collection agents (and their various combinations) can be seen in Figure 2. This reveals that the sources of funds – or who pays for health services – can vary from individuals, households, employees, and employers (firms and corporate bodies) to loans, grants, and donations from foreign governments, nongovernmental organizations (NGOs), and charities. In most national health systems, however, funds derive primarily from the population (by individuals and/or those that employ them).
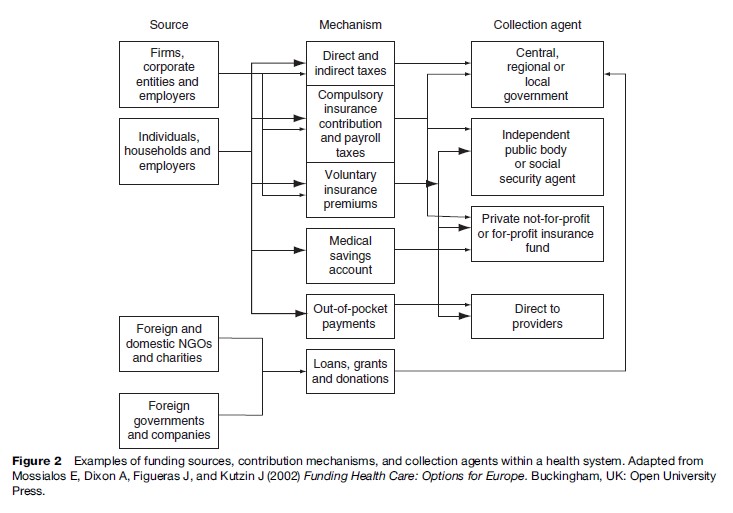
Methods Of Revenue Collection
As Figure 2 shows, there are many different approaches to collecting revenue including taxation, social health insurance, private health insurance, out-of-pocket payments, and loans and donations. National health systems are often defined by their dominant revenue collection. Thus, health systems in France and Germany are known as social health insurance systems because it is that method that generates the principal source of funding. In a similar way, countries such as the United Kingdom or Sweden are often referred to as tax-based systems while in the United States it is private health insurance within a business model of health-care provision that predominates.
In many low-income countries, however, economic hardship means that their ability to collect prepayments by way of social health insurance or tax revenues is limited, so their systems rely on out-of-pocket charges and donor contributions. Indeed, in lower-income countries around the world, revenue collection methods tend to be less able to finance care through forms of prepayment. For example, in Latin America, most countries employ a mixed model of social health insurance, private health insurance, and taxation for public health services with a higher percentage of out-of-pocket expenditure. In sub-Saharan Africa, out-of-pocket payments are the principal source of revenue, exposing individuals to the risks associated with meeting health-care costs that prepayment schemes that pool funds for a defined population do not.
Taxation
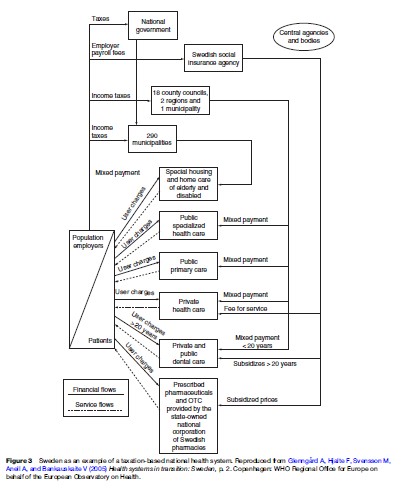
Taxation methods of raising revenue for health systems can vary a great deal. For example, taxes may be raised for general purposes (the proportion allotted to health care to be determined later) or hypothecated such that a certain proportion is earmarked for health purposes. The potential advantage of the latter is that it directly links tax and spending, making it more transparent to the public where tax money is spent. A key disadvantage, however, is that it reduces the ability to be flexible in the prioritization of government tax revenue and limits the range of tax sources that governments may use to obtain health funding. Taxation may also be ‘direct’ – for example, levied on individuals through an income tax or on businesses by a company tax – or ‘indirect’ such as taxes on goods and services that people buy, import, and export. Whereas direct taxes have the advantage over indirect taxes in their ability to be progressive (high-income earners pay relatively more yet health benefits are available to all) rather than regressive (fixed amounts, e.g., for a vehicle license), certain direct taxes can have the benefit of influencing consumer behaviors. Taxing goods such as tobacco or alcohol may deter consumption of goods regarded to do harm to health and so help improve health itself. Taxes that go to health care are often also raised locally as well as nationally – an approach that is argued to improve accountability and responsiveness to local people because the system provides more transparency since health-care expenditure in a local tax system is usually the largest percentage of what a local authority spends (e.g., up to 70% in Sweden). However, in systems without adequate redistributive mechanisms of tax income between rich and poor localities, inequalities in health-care provision inevitably arise.
A good example of a national health system that is predominantly funded through taxation is Sweden (Figure 3). In Sweden, there are three independent government levels involved in health care: the national government, the county councils, and the municipalities. All three levels play an important role in the welfare system and are represented by directly elected bodies that have the right to levy taxes on the population to finance their activities. Overall goals and policies are set at a national level by the Ministry of Health and Social Affairs, while both the financing and provision of healthcare services are primarily the responsibility of the county councils. According to Sweden’s three basic principles for public health and medical care – the principle of human dignity, the principle of need and solidarity, and the principle of cost-effectiveness – care should be provided on equal terms, according to need, and it should be managed democratically and financed on the basis of solidarity (Glennga˚rd et al., 2005).
Social Health Insurance
Social health insurance is a system of contributions (usually compulsory) shared between employee and employer who pay a percentage of income to a government-sanctioned insurance fund. Like taxation-based funding, a key advantage is the process of prepayment into a large risk pool (discussed later), and like taxation-based funding, there is tremendous variance in the methodologies employed internationally to collect the insurance payments. Hence, in Germany, ‘sickness funds’ are created both by geographical locality and by occupational group, while in France and the Netherlands, the system is organized through smaller independent funds that provide the population with choices on the types and levels of care coverage they would prefer.
Single national insurance funds are also common, such as those that existed in Croatia and Slovakia.
Social health insurance systems are often regarded as preferential to taxation models of funding since budgetary and spending decisions are ring-fenced (that is, funds are reserved specifically for expenditure on health care). In theory, this protects health-care funding from political interference. Moreover, a key element to such systems is the development of social solidarity since the system guarantees the entitlement to individuals of a set level of health-care coverage at a cost that is highly visible to them. However, as Goodwin et al. (2006) note, the system is not without its disadvantages. For instance, since eligibility is based on employment, there is the potential for restricted access to the elderly and unemployed. Also coverage tends to focus primarily on personal health care, rather than on the nonpersonal elements of a health system that emphasize public health interventions. Significantly, as costs of health systems in all Western countries rise, social health insurance is less able to adapt to the rising costs of provision. Indeed, as the example of the French health-care system shows (Figure 4), social health insurance systems often include significant elements of taxation-based subsidies, additional voluntary insurance, and various user charges that help to bridge the gap between revenues collected and expenditure.
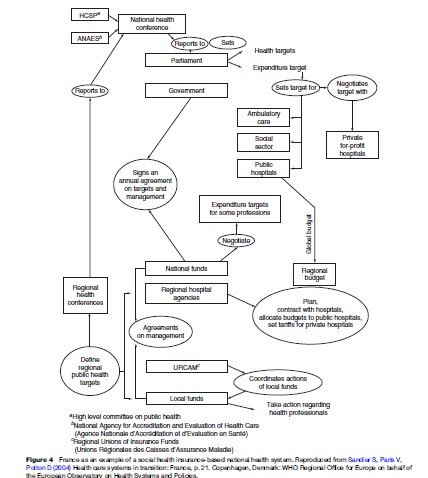
The French health-care system (see Figure 4) was inspired by the Bismarckian (German health system founded by Bismarck) model, with health insurance funds under the supervision of the state. It relies on a combination of public and private supply, even in the hospital sector. Patients benefit from easy access to care (freedom of choice, direct access to the specialists) and an abundant supply of self-employed doctors, in particular. Complementary voluntary health insurance to cover the cost of statutory copayments is widespread (Sandier et al., 2004). The financial sustainability of the French healthcare system is a perpetual source of concern, particularly due to the fact that actual expenditure consistently exceeds the targets set. Until now, the high cost of the health-care system has been accompanied by high levels of access to health care, but the demographic change expected within the health professions may lead to an increase in explicit rationing in future years. Nonetheless, the French health-care system was ranked the best in the world in the World Health Report 2000 for its effective combination of responsiveness to demands and social equality (WHO, 2000).
Private Health Insurance
Unless you live in the United States, private health insurance is usually of a second order of significance in the funding of your national health system. In low-income countries, for example, private insurance accounts for less than 2% of total health expenditure whereas in high-income countries it rarely exceeds 15%. Private health insurance is obviously least affordable to those on the lowest incomes yet is not necessarily the domain of the most affluent. For example, in both social health insurance and tax-based national health systems, private health insurers are often used by individuals to fill gaps in service coverage that are otherwise excluded from the nationally funded system. This form of private insurance is thus complementary to existing entitlements and is sometimes known colloquially as a top-up policy.
There are two other main forms of private health insurance: supplementary and substitutive. Supplementary insurance takes the form of an additional payment to receive enhanced benefits in addition to those offered through a social health insurance scheme. Hence, it may allow for quicker access to care, can be located in more comfortable surroundings, or be exempt from the costs of copayments such as those levied on drugs or inpatient stays. As Table 2 shows, more than 90% of individuals in the French health system take out supplementary private insurance to protect against the high level of copayments involved in accessing the nationally funded system.
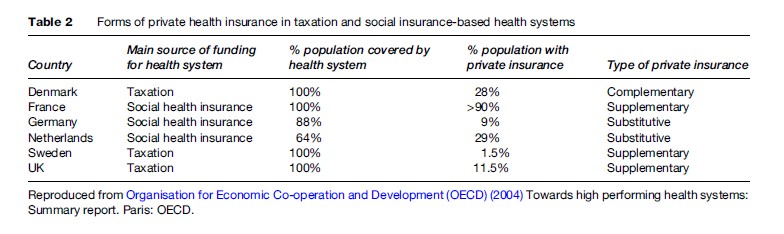
Substitutive private insurance, as the name implies, is an alternative to social health insurance and is taken up by those who may be excluded from public cover. In Germany and the Netherlands, for instance, employees earning above a certain income are excluded from care provided by the social insurance scheme (though not exempt from making payments) and are required to take out ‘compulsory voluntary’ insurance to get the care they require. Depending on their level of income and personal choice, individuals may opt back into the national system of social insurance health coverage or seek a private insurance agent. As Table 2 shows, supplementary, substitutive, and complementary private health insurance tends to be prevalent in certain types of national health systems.
The United States remains the only Western healthcare system whose primary source of funding comes through private health insurance. It is also the only country among the most developed nations without universal health-care coverage. Often referred to as a business model, the health system in the United States comprises a complex array of competing company-based and private for-profit and not-for-profit health insurance agencies offering a range of care plans to consumers and/or their employers. Providers of care, often working in large group practices and/or associations, contract with insurance agents (sometimes exclusively) and are generally paid on a fee-for-service basis. Cost inflation in the U.S. health system – influenced by the predominance of fee-for-service provision, investment in medical technologies, the high cost of medical malpractice claims, and high consumer demands – has resulted in the most expensive healthcare system in the world (16% of GDP in 2004).
Such rising costs have led to a growing number of citizens who are underinsured or without any health insurance coverage, despite a significant tax-funded component manifest in Medicare (for the elderly) and Medicaid (for the poor and disabled). To counteract these system failures, local managed care systems run by health maintenance organizations (HMOs) developed in the 1980s to provide enrollees with comprehensive care packages through an exclusive and integrated network of providers. However, antitrust legislation and consumer demands for lower-priced health plans have all but led to the demise of the HMO movement.
Out-of-Pocket Payments
Unlike in the previous three prepayment models, where it is possible to pool funds and spread risks among a population, a health system in which people must pay out of their own pockets for a substantial part of the costs of health services clearly restricts access to the more expensive forms of care. In most low-income countries, where prepayment systems are unavailable, out-of-pocket payments are often the only way to raise revenue and cover costs – leaving those who cannot afford treatment at higher health risks. Community financing is a method often promoted in such countries in an attempt to create pools of funds and reduce risks. For example, the Bamako Initiative – promoted in many parts of Africa since 1987 – helps provide local access to essential primary care services by decentralizing revenue collection and decision making to local communities. The basis of this approach to health system funding is to levy a small out-of-pocket charge when a drug or basic care is provided and then invest this in a fund from which local people prioritize investment into their community’s health needs. The approach has been moderately successful and has led to relative improvements in coverage, affordability, and use of care in many parts of Africa (McPake et al., 1993).
In high-income countries, where prepayment models exist, copayments and user charges are often employed as a form of both income generation and also demand management by health system architects faced with the prospect of rising health expenditures resultant from growing consumer needs and demands. Depending on the level at which these user charges are set, and on the use of exemption strategies for at-risk populations, such fees have been criticized for dissuading the poor from using services. They also do not appear to raise revenue to enable sustainable improvements to care and are inequitable.
Loans, Grants, And Donations
External aid is a substantial source of funding for the health sector in many low-income countries where it can account for as much as 90% of the overall health budget. Aid is most often provided by bilateral agencies (donors from a particular country) such as USAID (United States), DANIDA (Denmark), and DFID (UK). Multilateral agencies (pooled donor resources between countries) are also prevalent and include organizations like the World Bank and the United Nations Development Fund (UNDF). Aid from such organizations is often provided as loans or grants to which a set of conditions concerning their use is established by donors; in most cases, these are linked to specific projects that are developed and delivered separately between donors and national governments. While many projects have been successful, project-based approaches have been seen to lead to fragmentation and duplication of effort and/or time and effort from national governments in responding to the priorities of donors rather than concentrating on wider health sector programs. Moreover, grants do not necessarily lead to greater expenditure in the health sector as governments may view the funding as a substitute for their own expenditure, or as an opportunity to channel resources toward other priorities. Loans, grants, and donations, if not managed carefully, may thus do more harm than good. Aware of this, many donors and governments are beginning to embrace longer-term and strategic support programs; such sector-wide approaches have been seen to be successful in countries such as Bangladesh, Ghana, and Pakistan.
Pooling Resources
Fund pooling is the sharing of risk between contributors. The ability to prepay for care services and to pool funds has significant advantages for a national health system because it enables the equalization of contributions among members, regardless of their risk of needing to use services. Moreover, the approach has the benefit of economies of scale, thus allowing for cross-subsidization. Table 3 gives examples of how different countries can approach risk pooling, for example, from the development of social insurance funds (sometimes called sickness funds) to smaller community-based pools. As the examples imply, a range of agents might be involved in the pooling process from which a larger central pool is developed or, conversely, pooling might be devolved on the basis of risk-adjusted allocations to regional or local agencies who are then enfranchised to address local health-care needs and priorities.
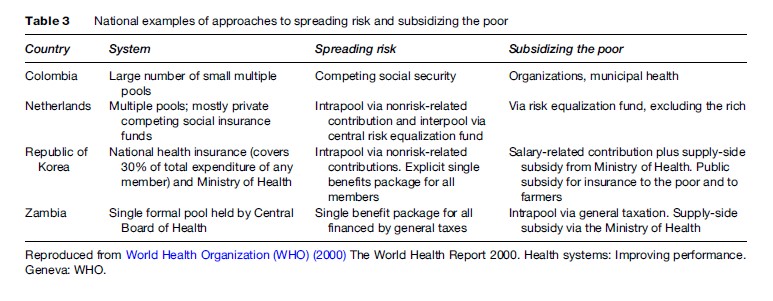
Larger risk pools are obviously better than small ones because they can increase the overall availability of funds to improve and develop health services, enable economies of scale in administration, and reduce the levels of contribution to protect individuals against uncertain need. From Table 3, it might be predicted that Colombia’s fragmented system of small organizations would damage the performance of the health system in these three areas. Evidence from Argentina pre-1996, in which there were more than 300 small pooling organizations in the system – most with fewer than 50 000 members – would support this proposition. The many small pools of funds meant that available health-care packages were very limited (especially in poor areas where low wages limited contribution levels). In West Africa, community financing initiatives to raise local pools of funding to plan and deliver drugs and care to local people have in many cases provided some protection from the risks of out-of-pocket payments, but the low level of pooled resources means such approaches are beset with problems of financial sustainability (Goodwin et al., 2006).
The key lesson to be learned from this section is that the ability of a national health system to prepay for health care, and to develop large resource pools to cross-subsidize care between high and low-risk people, is fundamental to a national health system’s sustainability and operational effectiveness. It should be noted that it is not the number of pools that is the issue, but their size relative to population health-care needs.
Purchasing Health Services
The management of purchasing is essential in ensuring that providers of services meet the goals of a national health system. As Goodwin et al. (2006) discuss, purchasers of health services face three fundamental challenges: which packages of care to buy, from whom to buy them, and how to buy them. Size is important for purchasing organizations because larger purchasers not only have administrative advantages in terms of economies of scale, but also have more bargaining capacity over both price and quality.
Which Packages Of Care To Buy: The Role Of Strategic Purchasing
Strategic purchasing requires a continuous search for the best interventions and care packages to purchase. This can be seen to occur at two levels in national health systems – first, at a societal and political level, the extent of healthcare coverage and the goals of the system (related to the section entitled ‘Stewardship’ later in this research paper); and second, the identification of those services and interventions that will meet these goals best. The latter implies responsibility for allocating resources and/or creating incentives and negotiating with providers.
Many countries, especially low-income countries, cannot afford to provide comprehensive health-care benefits for the entire population and face major imbalances in resource allocation – for example, between rural and urban regions, and between rich and poor communities. Defining priorities to achieve maximum health gain for the money that is available to purchase services becomes a key task. Many countries address this through a policy of essential care packages (ECPs) aimed at purchasing services with the greatest potential of reducing the burden of disease. The policy of ECPs has been promoted internationally as the most effective way of channeling scarce resources into interventions with the highest health impact.
How Health Systems Purchase Services
The mechanism through which care is bought – that is, how to purchase services – is crucial because the method of payment establishes different kinds of incentives that providers will react to and the subsequent cost and quality of the services they provide. As Goodwin et al. (2006) describe, there are three main methods by which health systems purchase services:
- Full retrospective reimbursement for all expenses incurred, manifest in fee-for-service payments;
- Reimbursement for all activity based on a fixed schedule of fees using a tariff, based on a system of health or diagnostic-related groups (HRGs and DRGs); and
- Prospective funding based on the expected future expenditure using a fixed budget, manifest in salaried employment, directly managed and/or devolved budgets, and capitation.
Retrospective reimbursement is a payment scheme whose level is determined only after services have been provided. It may involve per diem payments, a cost-per-case, or a direct service payment. To health systems, the main problem with this model of purchasing is the inability to control provider costs effectively due to weak forms of audit and control of activity. In the United States, for example, the cost of Medicare and Medicaid services (tax-based funding for the old and poor) that began in the 1960s could not be maintained beyond 1983 because federal government income did not provide enough revenue to cover costs. It was known as the blank-check era since providers received payment for all care deemed ‘customary, usual, and reasonable.’ As the number of people on Medicare rapidly climbed and costs spiraled the system was replaced with DRG-based funding; a similar policy shift occurred in Germany’s social insurance system in the early 1990s.
Prospective payment requires a tariff to be set to charges agreed in advance with providers, the most common being the DRG. DRGs categorize patients based on their primary and secondary diagnoses, primary and secondary procedures, age, and length of stay. The categories establish a uniform cost, enabling funders to set a maximum amount payable for a suite of care to a patient. Under this system, providers are given the incentive to keep their costs down as they would experience a profit (or surplus) if their costs are below the tariff in the DRG category. National health systems, therefore, benefit from more efficient providers and provider competition based on quality rather than cost. Such as system, called payment by results, has recently been established in the English National Health Service (NHS) to replace traditional capitation-based funding.
Prospective funding is a system that many national health-care systems have in place. Under this system, a global budget for health-care spending is often set within which envelope care can be purchased. Funding agencies acting on behalf of governments then allocate a fixed proportion of that budget to providers. The method of allocation can vary, for example, from political negotiation (a settlement), to provider competition (a bid), or by way of historic precedent and activity. Most countries use more sophisticated combinations of the three, for example, devolving resources to local purchasing agencies based on the needs of local populations based on their demographic profiles (capitation). This approach is favored in most high-income countries of Europe where a fair share of resources through capitation-based formulae is generally mixed with historic local expenditures and political negotiations. Variations to the approach are, therefore, commonplace. For example, budgets in Italy are renegotiated retrospectively; local taxes are raised in Sweden to supplement the national allocation; care is rationed in Norway through waiting lists or entitlement changes; and in most countries, such as Finland, copayments are levied to raise revenue and manage demand.
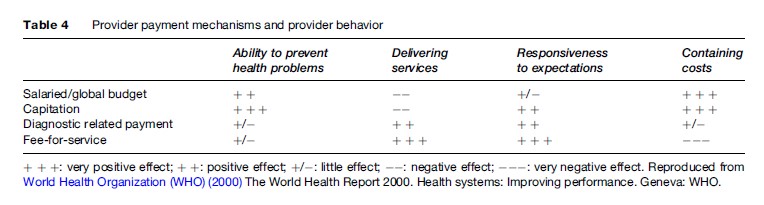
Types of provider payment mechanisms, therefore, produce different system incentives (Table 4). Fee-for-service and prospective payment mechanisms provide strong incentives to meet consumer demands and deliver timely services, but are weaker in containing costs and do not necessarily invest in services that prevent health problems. France is a classic example, and the rising costs of the system has led the French to reconsider its strategic priorities including limiting entitlements, increasing the use of copayments, and introducing capitation payments as a way of controlling costs. By contrast, the English NHS, historically highly cost-effective in service delivery terms due to its capitation-based system and primary care-led system of gatekeeping, has encouraged the move to a DRG-style system of funding to encourage providers to become more responsive to patient demands and so reduce waiting lists and improve access. National health systems, therefore, need to combine payment mechanisms if they are to achieve all their objectives. The French and English diversions away from their historical positions show how countries have attempted to change provider behavior to meet system needs – choice and responsiveness (in England) and cost containment (in France).
In national health systems, purchasing needs to be actively managed since the process of making strategic investment priorities can impact on equity and efficiency in provision. The performance of a health system is likely to fall short of its potential if resources are not allocated and spent wisely to gain the best mix of responses from providers that help to satisfy needs and improve care quality.
Providing Health Care
Referring back to Figure 1, health-care provision can usefully be split between personal and nonpersonal services. Personal services are those that people receive from a health agent, such as a doctor or dentist, while nonpersonal services are manifest in wider health promotion and disease prevention activities such as public health programs to promote healthy lifestyles or improve local environmental health.
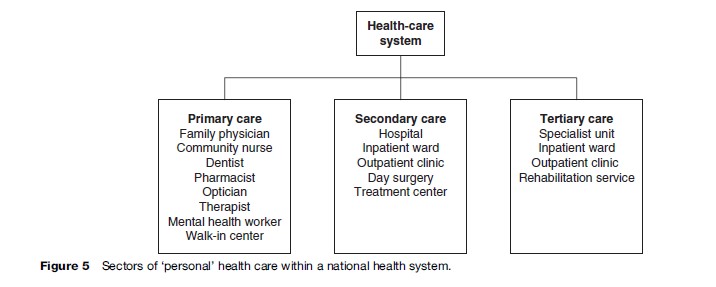
The provision of personal health-care services within a national health system has most often been categorized through a threefold classification – primary, secondary, and tertiary care (Figure 5). Primary care is regarded as the first level of contact between individuals, the family, and/or communities with the health system itself. The purpose of primary care services is to bring basic health care as close as possible to where people live and work. Primary care can be delivered by way of a wide range of community-based health professionals, such as family physicians, pharmacists, therapists, and dentists. Primary care forms an integral part of most country’s health systems and, as this research paper will show later, having an effective system of primary care providers is of crucial importance to overall national health system effectiveness. Secondary care, often referred to as the acute sector due to its predominant basis in hospital institutions, can be described as the episodic treatment provided for an illness or health problem and is primarily curative in nature. Often, secondary care services are accessed through referrals from family physicians and/or through direct access for accident and emergency care. Tertiary care takes the form of more specialized care often within a specialist center serving a larger population or even the whole country.
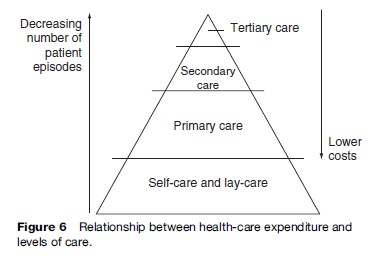
Across a national health system, the number of patient contacts and episodes decreases as one moves from informal lay care to primary, secondary, and tertiary sectors. Despite the reduced number of patients accessing care in each sector, the proportion of costs of health services provision to the system as a whole tends to rise exponentially. This can be seen in Figure 6. However, making generalizations about the structure of health-care provision using the general classifications discussed previously is invidious. In reality, the boundaries between care sectors are often ambiguous and blurred since care can shift seamlessly from one sector to another.
Care Pathways And Disease Management: The Emergence Of New Health System Models
There is a constant pressure to address increasing healthcare costs in most national health systems by attempting to develop more efficient and appropriate care practices. For example, many national health-care systems have taken the opportunity to redesign and streamline the care process to reduce the number of contacts with the different parts of the system, minimize the numbers of handovers and referrals between providers, and so make more appropriate (and cost-effective) the use of each sector. Purchasing and/or commissioning care delivery across a redesigned care pathway has been claimed to be more efficient in terms of resource use, enabling patients quicker access to treatment and maximizing long-term health outcomes.
An alternative, often linked, approach is based on the greater ability of the system to promote good health and/or enable the management of illness without recourse to the need for the more expensive forms of care. Indeed, most countries, whether high or low income, seek to promote health and manage illness outside of institutionalized structures. As a consequence, patients are increasingly being prescribed integrated care packages across the previous dimensions of care (such as a disease management program) and/or investment is made in the capacity of primary care providers, and indeed of people themselves (‘self-care’) to promote good health and provide effective and early interventions that limit the need for people to access the more expensive forms of care.
Disease management as the basis for a health systems design is a concept developed in the United States during the 1990s and has been a growing phenomenon in health systems around the world, although its specific forms strongly depend on the health-care system in which it is applied. A number of definitions for this model of care exist, but roughly it encompasses a systematic, population-based approach to tackling specific diseases and health problems by developing programs of care to advance health system quality, efficacy, and health outcomes. In the United States, disease management programs mainly focus on reduction of costs by targeting short-term interventions to patients currently in relatively good health yet at high risk of using secondary and tertiary care in the near future. In Europe the use of disease management mechanisms is accelerating. For example, in Spain, Insalud (the Spanish National Health Service) has contracted out disease management programs for heart failure and diabetes in Barcelona and Madrid. In Germany, national government has by law introduced disease management programs as a lever to break up the traditional authority of physicians while seeking to reduce rising long-term costs.
Figure 7, adapted from the ‘Kaiser Triangle’ disease management model of the U.S. managed care organization Kaiser Permanente and later adopted by the Department of Health in England (Department of Health, 2004), describes the type of health-care system that should be provided to people suffering from, or at high risk for, chronic disease. Unlike the care triangle described in Figure 6, the health system model is not based on institutional sectors (i.e., primary, secondary, and tertiary care), but on different approaches to manage patients’ needs. At the top of Figure 7 lies case management (the top 5% of people with chronic disease) for people with advanced and acute conditions who require intensive and actively managed care by professionals. At the second level – disease management (the next 15% of cases) – proactive case management by multiprofessional and integrated teams is required, perhaps following specified pathways of care, but including a high degree (about 50%) of support to self-care. For the majority of patients (about 80%), chronic disease remains a condition (or a risk) that does not require active professional intervention but can, through the right support, be addressed by engaging patients to be active in the self-management of their conditions and so prevent any deterioration. Given the numbers of people in this part of the triangle (about 80% of cases, or 48% of the whole population) one can see that effective self-care strategies are crucial to the overall effective support for people with long-term conditions (i.e., reducing the numbers of people subsequently moving up the triangle) (Department of Health, 2004).
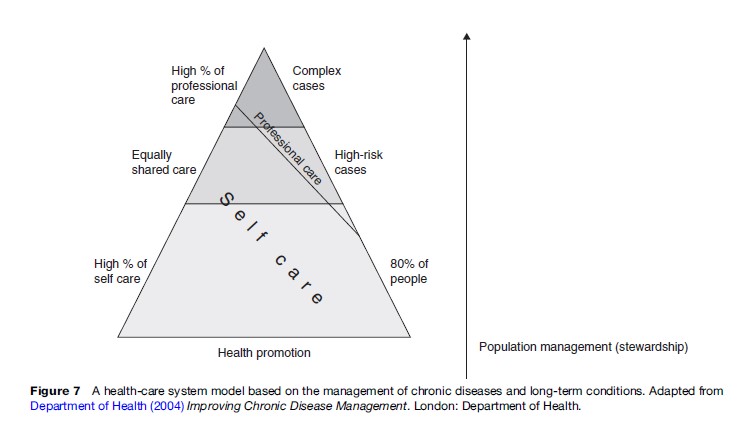
Figure 7 also shows that for such a health-care system based on disease management to be effective, it requires a significant degree of management to ensure that local services to a defined population are tailored to meeting needs. As the model implies, it is the purchasers’ responsibility to ensure that strategies are in place for high-risk groups to help prevent the onset of chronic disease, and to enable self-management for those living with such conditions. The range of self-care support tools that purchasers might seek to encourage, therefore, lies both within and out of the personal health sectors and includes: patient education, self-skills training, self-diagnostic and self-monitoring tools, home adaptations, and peer support networks. As national health systems develop in high-income countries, the needs of an aging population and the rising burden of chronic disease and long-term care needs have begun to shift how care is provided from an acute sector paradigm (based on episodic care in hospital institutions) to one based on disease management (based in primary and community care sectors and blurring the boundary between the formal and informal care sectors).
Public Health
Until the 1970s it was commonly assumed that improvements in health experienced in most countries during the last century occurred as a consequence of advances in medical care. However, the evidence collated in the key work by Wilkinson and Marmot (2003) has shown that the most important factors to improve the health of people, patients, and populations lies primarily outside the formalized system of health care. This led the authors to a key observation that the amount of money spent on health care (in terms of percentage of GDP) is not in itself a direct and causal contributor to a nation’s health profile.
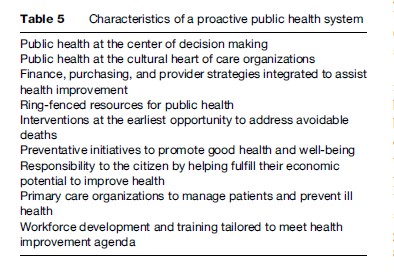
Many health-care systems internationally have made fundamental changes to the management and delivery of care in attempts to reduce inequalities in both health status and access to services following the realization that the role of a national health system must extend beyond the formalized systems of medical care to address the wider public health agenda through services and strategies aimed at improving well-being. At present, there is a struggle taking place in many health systems around the world to rebalance their policies and practices. Whereas there is a recurring policy theme internationally in the importance of developing a more proactive public health-based system, the necessary restructuring and reengineering of existing ways of purchasing and providing care services to achieve this implies radical system change (Table 5). For example, the core features of a public health system would require the provision of comprehensive public health programs for populations to improve and protect health, public health interventions that are integrated into the daily work of professionals in primary care, and the creation of multidisciplinary public health teams working in community-based managed care networks.
Stewardship
In the view of international agencies that have examined the relative performance of national health systems, it is clear that more effective health-care systems are those which are carefully and responsibly managed (WHO, 2000; OECD, 2004; Davis et al., 2007). Stewardship of a nation’s health system is important because it is people who entrust themselves (and their money) to a health service and so, in return, it becomes the responsibility of the system to protect the population by ensuring resources are used wisely. Most organizations cannot be left to themselves to deliver effective and excellent services, and improve quality, safety, and efficiency, so in most national health systems the government must fulfill the task of stewardship – whether through direct regulation of nationally funded providers or by way of the use of independent regulators in a mixed economy of public and private providers.
Stewardship of a health system through forms of regulation and governance can have three main objectives. First, policy makers may wish to stimulate capacity and productivity through entrepreneurial opportunities by encouraging competitive behavior. This might include permitting hospitals to retain operating surpluses, moving payment systems from fixed budgets to fee-for-service, or allowing hospitals to set their own fees. Second, regulators might wish to protect the system from the more negative aspects of competition through activities such as reducing adverse selection by health-care payers and providers, requiring insurance providers to accept all applicants, or setting minimum quality standards through licensing or accreditation. Third, regulation can concentrate on safeguarding social objectives, such as stipulating minimum waiting times or opening hours, setting uniform prices (tariffs), providing treatment guidelines and protocols, and undertaking quality assurance audits.
Many Western countries have introduced regulatory reforms to alter system behaviors. As a result, there has been a general increase in the number of regulatory bodies and activities at state and local levels in health care. For example, in the English NHS, a statutory duty to assess the performance of health-care organizations and publish performance ratings was established in 2004 by way of the Health Care Commission. The purpose of the approach was to ensure that providers – now enjoying greater entrepreneurial freedom and autonomy from the state – were still meeting core government standards of quality, safety, cleanliness, and waiting times (i.e., safeguarding social objectives). Such ‘steer and channel’ regulation is likely to play an important role in the short and medium term in many countries that are simultaneously encouraging competition but through rules consistent with core social objectives. Hence, well-designed regulatory mechanisms can stimulate needed entrepreneurialism while simultaneously safeguarding social objectives – the essence of stewardship.
The nature of stewardship has an important role to play in defining the characteristics of national health-care systems. Political leadership and legislation practice together defines the principles and conceptual frameworks around which health system financing, purchasing, and delivery operate. For example, in England, the core principles of a tax-funded NHS that is free at the point of delivery to all citizens according to need has remained unchallenged despite far-reaching reforms that have injected private-sector capital and management practices into the system. In France, the principle of la medicine liberale remains culturally important to citizens who value freedom of access to specialists within a socially equitable social health insurance-based system. As the WHO (2004) commented, leadership by the state – its vision, direction, and relationship with citizens – tends to define the overall strategic framework in which the component parts of a national health system operate.
What Factors Constitute A More Effective Health-Care System?
In Alan Gillies’ (2004) book that examined this question it was suggested that individuals wanted three fundamental things from their national health-care system: first, they wanted to be kept as healthy as possible; second, when this is not possible, they want to be treated and made better as soon as possible; and third, they want care provided at a minimum (or best value) cost consistent with the first two goals. Hence, Gillies argued that the best health-care systems were those that enabled the greatest possible health improvement and health-care provision within the funding available. In common with international studies examining the factors associated with better health-care systems (OECD, 2004; WHO, 2000; Davis et al., 2007) these observations reveal that it is not the level of spending that counts – as there is no single most appropriate level – but how that spending is used that matters.
Responsiveness and choice have become important criteria in the more affluent nations as they seek to meet personal demands for health care (as opposed to national needs) through patient-led care. However, as Gillies argues, the priorities that have become prevalent in Western countries are for most parts of the world an unrealistic dream. Hence, he argues that it should never be forgotten that the basic responsibility of a national health system is to deliver the basics. Reflecting back to Maxwell’s (1992) basic quality measures that define the purpose of national health systems (see Table 1), and the realization that no single principle is necessarily more important than another, how might it be possible to objectively measure, on a comparative basis between nations, which type of national health system performs better than another?
The question is problematic because data that may be used to make effective comparisons between countries are fraught with difficulties. For example, comparisons are often made between national health systems based on their respective health expenditure relative to their nation’s wealth (as characterized by the percentage of GDP allocated to financing health care). However, understanding what can be, or is actually, purchased with this funding varies markedly in real terms (purchasing power) or in terms of the coverage and entitlement to care for all citizens. Moreover, meaningful health outcome comparisons can be argued to be confounded by contextual variances in the demographic, geographical, and socioeconomic profiles of different countries. As a result, comparisons have tended to use high-level indicators of performance between countries – such as levels of infant mortality or life expectancy at birth – all factors that we know are influenced more by factors outside the influence of formal health system interventions (Wilkinson and Marmot, 2003).
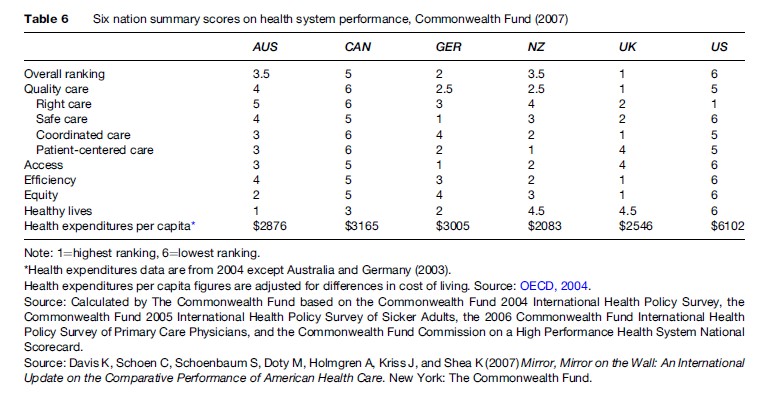
Perhaps the most famous comparative study is contained in the World Health Report 2000, which compares the health systems of 191 countries based on a ranking of eight key system measures, leading with a composite measure of these systems for overall health system performance (WHO, 2000). More recently, the Commonwealth Fund’s comparative analysis of six national health-care systems has added to the debate (Davis et al., 2007). What both uncover is that systems without universal health coverage and/or fragmented rather than coordinated care delivery fare worse in comparison to those that do, regardless of the amount of money spent on health care. For example, the United States (the most expensive health system) was ranked 37th in the World Health Report 2000 and last out of the six nation summary scores (Australia, Canada, Germany, New Zealand, UK, and the United States) in the Commonwealth Fund’s assessment (Table 6).
The OECD’s (2004) study of 29 industrialized nations suggested that the following key factors were associated with high-performing health-care systems:
- a sustainable and robust financing system;
- care that is provided to all the population and care that is coordinated so recipients are looked after ‘from cradle to grave’;
- a focus on prevention of ill health and the promotion of public health;
- an effective monitoring and regulation system; and
- strategic planning to ensure resources for health care are being put to good use, for example, harnessing the potential of advances in information technology.
Each of these reports can rightly be criticized for the methodological inadequacies in their assessments. Yet, each serves to highlight two central issues we know about the effectiveness of national health systems: first, that achieving good health outcomes in a national health system is more about how the system is designed and not necessarily related to how much is spent; and second, that different health-care systems are simultaneously trading off the achievement of different measures of system quality (e.g., in terms of access, efficiency, equity, and responsiveness).
Regardless of funding type, there is also evidence to suggest that more effective health-care systems have a stronger orientation to health promotion, disease prevention, and the provision of accessible and universal primary and community care-based services. The benefits of such a strong primary care-based component to a health system have been identified through influential analysts such as Barbara Starfield. By ranking the primary care orientation of 12 Western industrialized nations, she concluded that countries with a strong primary care base to their healthcare system achieved better outcomes, and at lower cost, than countries in which the primary care base was weaker (Starfield, 1998). In Starfield’s analysis, features that were consistently associated with good or excellent primary care included the comprehensiveness and family orientation of primary care practices, within a wider system in which governments regulated the distribution of healthcare resources by way of taxation or national insurance. Given that the burden of disease is shifting to the long-term chronically ill, national health systems must adapt to meet this challenge – a task requiring a move away from episodic care undertaken in specialist hospital institutions to long-term care management and coordination undertaken in the community. The importance of a primary care orientation to health system design with a strong public health component has never been more relevant.
Conclusions
In almost all Western countries, health-care systems are in a state of radical transformation as they simultaneously attempt to meet the demands of empowered consumers, incorporate evidence-based modes of working, apply disease management principles, and contain costs. The tensions implicit in these changes mean that the relationship between governments, insurance funds, health-care providers, medical professionals, and the public is in constant need of effective stewardship if the espoused goals of a national health system are to be achieved. Such stewardship requires effective regulation of activities to connect together the constituent parts of a national health system and enable, for example, the reconfiguration of personal and nonpersonal services to meet future health-care needs through a shift from a preoccupation with downstream care services to an upstream focus on the health of communities. However, achieving such ideals will be influenced by the two key features controlling the overall nature of a national health system: the involvement of the state (the ability of governments and legislative bodies to respond to system needs) and the limitations imposed by political and resource pressures.
Bibliography:
- Davis K, Schoen C, Schoenbaum S, et al. (2007) Mirror, Mirror on the Wall: An International Update on the Comparative Performance of American Health Care. New York: The Commonwealth Fund.
- Department of Health (2004) Improving Chronic Disease Management. London: Department of Health.
- Gillies A (2003) What Makes a Good Healthcare System? Abingdon, UK: Radcliffe Medical Press.
- Glennga˚ rd A, Hjalte F, Svensson M, Anell A, and Bankauskaite V (2005) Health Systems in Transition: Sweden. Copenhagen, Denmark: WHO Regional Office for Europe on behalf of the European Observatory on Health.
- Goodwin N, Gruen R, and Iles V (2006) Managing Health Services. Maidenhead, UK: Open University Press.
- Maxwell R (1992) Dimensions of quality revisited: From thought to action. Quality in Health Care 1(3): 171–177.
- McPake B, Hanson K, and Mills A (1993) Community financing of health care in Africa: An evaluation of the Bamako Initiative. Social Science and Medicine 36(11): 1383–1395.
- Mossialos E, Dixon A, Figueras J, and Kutzin J (2002) Funding Health Care: Options for Europe. Buckingham, UK: Open University Press.
- Organisation for Economic Co-operation and Development (OECD) (2004) Towards High Performing Health Systems: Summary Report. Paris, France: OECD.
- Sandier S, Paris V, and Polton D (2004) Health Care Systems in Transition: France. Copenhagen, Denmark: WHO Regional Office for Europe on behalf of the European Observatory on Health Systems and Policies.
- Starfield B (1998) Primary Care: Balancing Health Needs, Services and Technology. Oxford, UK: Oxford University Press.
- Wilkinson R and Marmot M (eds.) (2003) Social Determinants of Health: The Solid Facts, 2nd edn. Geneva, Switzerland: World Health Organization.
- World Health Organization (2000) The World Health Report 2000. Health Systems: Improving Performance. Geneva, Switzerland: World Health Organization.
- World Health Organization (2004) The World Health Report 2004. Changing History. Geneva, Switzerland: World Health Organization.
- Hunte D (ed.) (2007) Managing for Health. London: Routledge.
- Schrijvers G (ed.) (2005) Disease Management in the Dutch Context. Netherlands: ZuidamUithof Drukkerijen.
- Smith J and Goodwin N (2006) Towards Managed Primary Care: The Role and Experience of Primary Care Organizations. Aldershot, UK: Ashgate.
- Walshe K and Smith J (eds.) (2006) Healthcare Management. Maidenhead, UK: Open University Press.
See also:
Free research papers are not written to satisfy your specific instructions. You can use our professional writing services to buy a custom research paper on any topic and get your high quality paper at affordable price.








